Educational aims and objectives
This self-instructional course for dentists aims to discuss dental implant treatment of the atrophic maxilla following the PATZI protocol.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Use the PATZI protocol to make rapid treatment decisions for the treatment of severely atrophic maxillae following a logical and systematic algorithm.
- Recognize that multiple different implant fixtures are readily available for treatment of severely atrophic maxillae.
- Recognize that the PATZI protocol offers a systematic algorithm for rapidly planning the treatment of severely atrophic maxillae.
- Identify situations in which the PATZI protocol allows for real-time alterations of planned surgical treatment based on intrasurgical outcomes.
- Recognize that the PATZI protocol may result in an infinite number of remote anchorage implant combinations to treat any atrophic maxilla.
Dr. Dan Holtzclaw explains the PATZI protocol, when remote anchorage is necessary for the implant procedure.
Dr. Dan Holtzclaw discusses a systematic algorithm that allows for real-time modifications during surgery
Introduction
Treatment of the atrophic maxilla was once thought impossible,1 but advances in dental implant technology and surgical techniques over the past 30 years have significantly remedied this situation. In 1985, Tulasne performed the first placement of root-form pterygoid implants which used remotely located dense pterygomaxillary bone for restoration of compromised posterior maxillae.2 This was soon followed by Brånemark who in 1987 utilized dense bone of the zygoma to further facilitate restoration of atrophic maxillae.3 While these protocols afforded new treatment options for severely resorbed maxillae, prosthetic restoration of these early remote anchorage implants often resulted in bulky prosthetics that compromised patient comfort and speech.4-9 These issues were improved when Stella and Warner introduced the extramaxillary zygomatic implant “slot” technique at the turn of the millennium 13 years later.10 This protocol lateralized placement of zygomatic implants, thus eliminating excessive palatal platform positioning associated with the original Brånemark protocol. Bothur next proposed use of multiple fixtures per zygoma to completely eliminate the need for bone grafting in severely atrophic maxillae.11 In 2003, Malo, et al., published the first paper documenting use of the All-On-4™ protocol for restoration of edentulated maxillae with immediate loading.12 Over the ensuing decade, Aparicio, et al., published a series of studies that culminated in the development of the Zygomatic Anatomy Guided Approach (ZAGA) which refined placement of zygomatic implants further improving prosthetic restoration of the atrophic maxillae.13-17 In 2018, Holtzclaw introduced the Pterygoid Fixated Arch Stabilization (PFAST) protocol employing immediately loading of pterygoid implants to eliminate prosthetic cantilevers which were often associated with problems that sometimes arose from the All-On-4™ protocol.18
The purpose of this paper is to highlight continued advancements in treatment of edentulated and atrophic maxillae with introduction of the PATZI protocol: (P)terygoid, (A)nterior (T)ilted (Z)ygomatic (I)mplants.
PATZI protocol concept
The PATZI protocol is a systematic algorithm for rapid treatment planning of atrophic maxillae which allows for real-time modifications during the surgical procedure.20 PATZI employs immediate loading and remote anchorage concepts developed over the past 35+ years to produce a near infinite combination of dental implant setups to accommodate nearly any situation that may present in atrophic maxillae. PATZI starts with attempted placement of pterygoid implants to employ their numerous benefits of cantilever elimination, maximizing anterior-posterior spread, and increasing composite torque value.18-21
If pterygoid implants are successfully placed, the algorithm next proceeds to achieve anterior support. Anterior prosthetic support may be attained with standard axial, nasopalatine, piriform rim, or transnasal fixtures.12,22-24 If anterior support is achieved, PATZI now proceeds to achieve mid-maxillary support via tilted implants which may be of either traditional or trans-sinus varieties.12,25 If pterygoid or mid-maxillary tilted implants are not successful, PATZI calls for placement of a posteroinferior zygomatic implant. Alternatively, failure to achieve placement of an anterior implant necessitates placement of an anterosuperior zygomatic implant. In the event that multiple zygomatic implants are required in a single malar process, the presence or absence of a pterygoid implant will influence the configuration of the zygomatic fixtures: parallel versus “A-Frame.”20
If a pterygoid implant is present, the zygomatic implants can be placed in a parallel configuration. While parallel zygomatic implants have the disadvantage of an anteriorly located posterior prosthetic platform, they have the benefits of more superior malar real estate for the placement of a second zygomatic implant and eliminate the possibility for collision with the anterosuperior zygomatic fixture. The shortcomings of the posteriorly located posteroinferior zygomatic implant are offset by the pterygoid implant which maximizes AP spread and eliminates prosthetic cantilever. If a pterygoid implant is not successfully placed, zygomatic implants are placed in an A-Frame setup with the posteroinferior fixture placed in a more posterior position. Placement in this manner distalizes the prosthetic platform of the posteroinferior zygomatic implant, shortening the resultant cantilever of the restoration.
Alternatively, the A-Frame setup brings the posteroinferior zygomatic implant apex closer to the orbit, thus reducing available real estate for the anterosuperior zygomatic fixture and increases the risk of implant collision. The PATZI protocol is employed to the left and right sides of the maxilla independently. The remainder of this article presents a series of cases that demonstrate the applicability of the PATZI protocol for treatment of atrophic maxillae.

Case 1
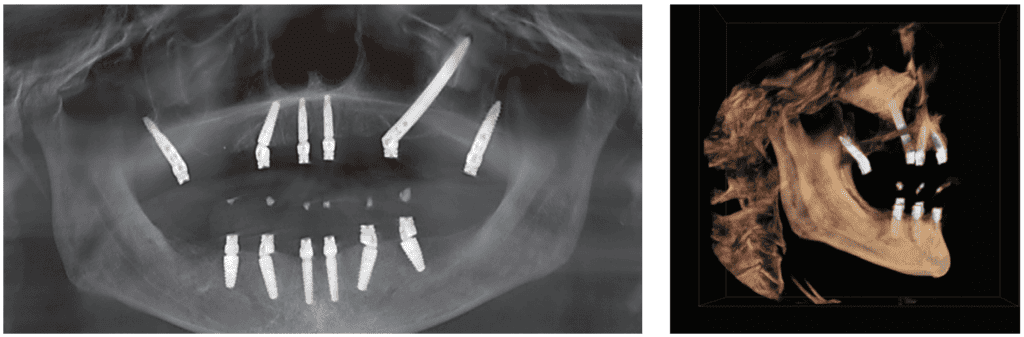
A 42-year-old female patient was referred to the author for treatment of a severely atrophic maxillae which had a history of trauma and several failed prior treatment attempts. The patient’s medical history was unremarkable. Presurgical radiographic evaluation revealed a deficient premaxilla with minimal sub-nasal bone precluding the placement of standard, nasopalatine, and piriform-rim dental implants. Evaluation of the prelacrimal recesses revealed radiopaque bone suggestive of dense quality and measurements consistent with Simmen 2 classification on the left and Simmen 1 on the right.31 In the mid-maxilla, both maxillary sinuses were severely pneumatized but appeared radiolucent with minimal thickening of the Schneiderian membranes. Evaluation of coronal CBCT slices suggested patent osteomeatal complexes bilaterally. The zygomas presented radiopacity consistent with dense bone, but were constricted in height compared to average measurements reported in published literature.32-36 Posteriorly, minimal subantral bone was noted bilaterally, and the pterygomaxillary complexes contained radiopaque bone of standard dimensions.
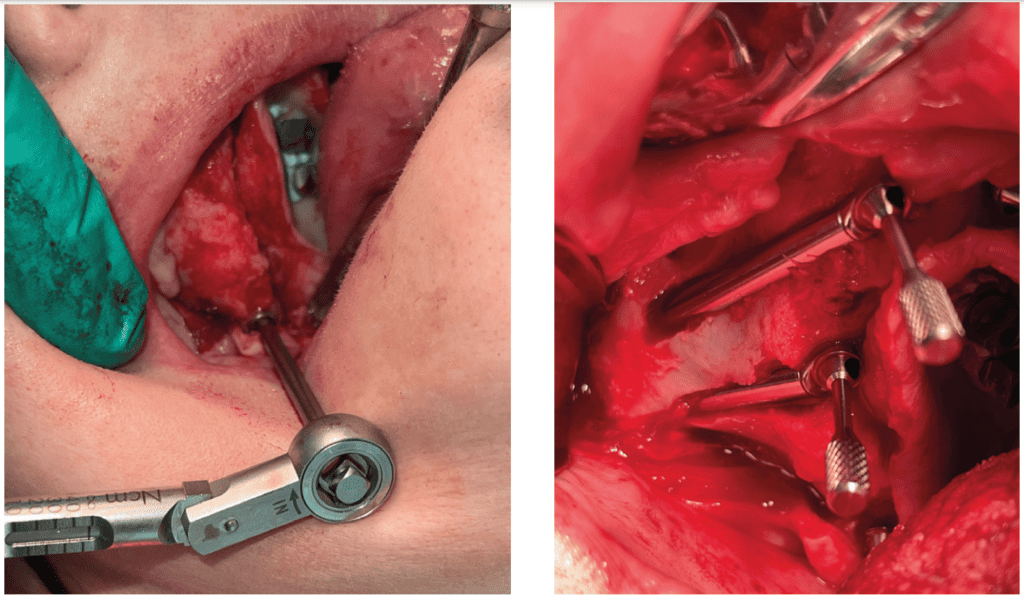
Following the induction of general endotracheal anesthesia with an anesthesiologist, local anesthesia was provided intraorally. Supplemental local anesthesia was administered extraorally at both infraorbital nerves and malar prominences. A full-thickness mucoperiosteal flap was elevated to bilaterally expose the piriform aperture, infraorbital nerve, malar prominence, and hamular notch. As the maxillary arch was already severely atrophic, no bone adjustments were required to obtain prosthetic space. Following the PATZI protocol, a 4.2 mm x 18 mm pterygoid implant was placed on the patient’s right side achieving high insertion torque of 45+ Ncm. On this same side, no bone was available for anterior or mid-maxillary implant placement, thus eliminating the possibility of implant placement according to (A) and (T) in the PATZI. Accordingly, the protocol called for placement of multiple zygomatic implants in the right malar prominence.
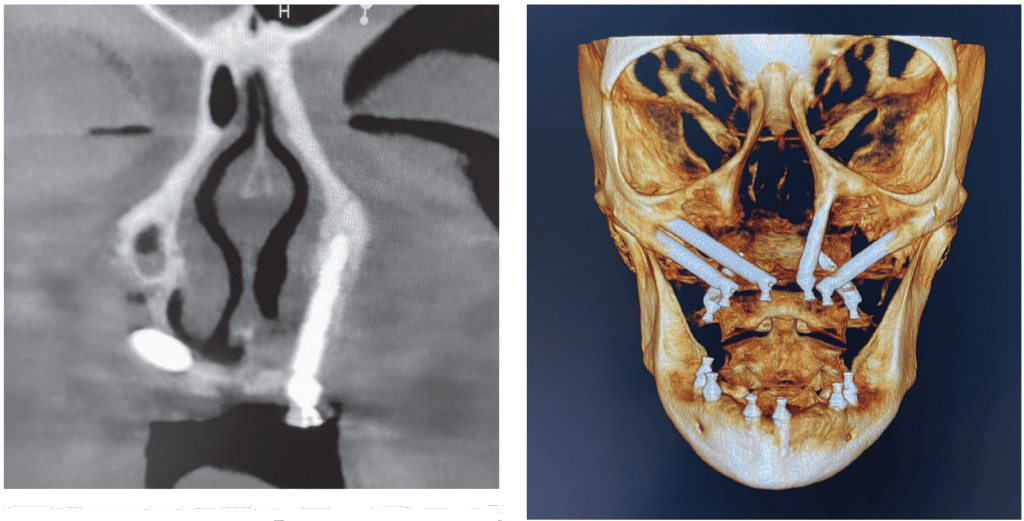
As a pterygoid implant had been successfully placed in the right pterygomaxillary region, a parallel zygomatic setup was employed. On the patient’s left side, a 4.2 mm x 18 mm pterygoid implant was placed in a similar fashion to the contralateral side in accordance with the PATZI protocol. As PATZI next calls for anterior implant support (A), a transnasal implant was attempted as bone in the left prelacrimal recess appeared adequate. The left nasal mucosa was reflected superiorly to the inferior concha and a 3.8 mm x 24 mm was placed with insertion torque exceeding 45Ncm. With pterygoid and anterior support achieved on the left side satisfying (P) and (A) of PATZI, mid-maxillary support was sought with tilted implants to satisfy (T). With no adequate bone to support tilted implants, a posteroinferior zygomatic implant was placed. With composite torque value exceeding 350+ Ncm, the maxillary arch was immediately loaded with a transitional restoration. The procedure completed without incident, and the patient was pleased with the outcome (Figures 1-6).

Case 2
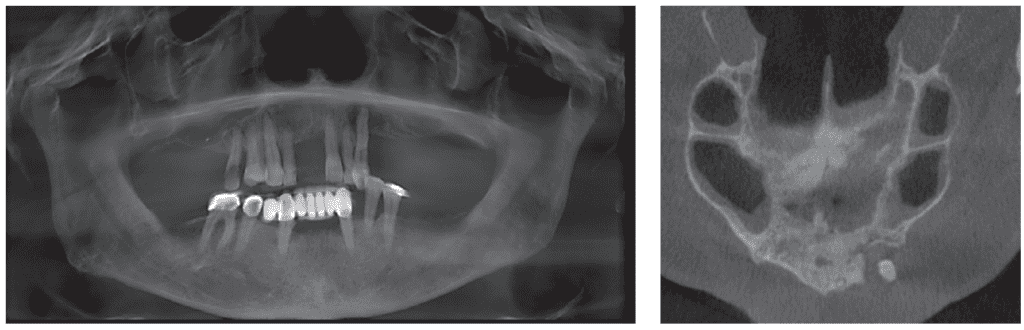
A healthy 83-year-old female patient presented to our clinic seeking full-mouth implant rehabilitation. She had been edentulous in the maxilla for more than a decade, and her mandibular prosthetic work had recently begun to deteriorate. Presurgical radiographic evaluation revealed a premaxilla with mixed amounts of alveolar atrophy. The right anterior maxilla had bone of adequate thickness for a smaller diameter implant while the left side had severe atrophy. Moderate pneumatization of the maxillary sinuses was evident with relatively radiolucent subantral bone suggesting low density. The pterygomaxillary complexes suggested areas of dense bone in the pyramidal processes and pterygoid pillars with the right side appearing more robust than the left.

Anesthesia and flap reflection were carried out in a similar fashion to that of Case 1 in this article. Following the PATZI protocol, a 4.2 mm x 18 mm pterygoid implant was first placed with 45+ Ncm insertion torque on the patient’s right side. With (P) of PATZI satisfied, anterior (A) implants were attempted next. The neurovascular bundle of the nasopalatine canal was enucleated and a 4.2 mm x 10 mm implant was placed with 45+ Ncm torque. Additional support for the patient’s anterior right side was achieved with a 4.2 mm x 13 mm implant that engaged the dense bone of the piriform rim. With minimal subantral bone remaining, a tilted implant was not possible.
With (T) of PATZI not satisfied, mid-maxillary support was achieved with a right posteroinferior zygomatic implant. This zygomatic implant was placed in the inferior aspect of the zygoma to preserve the possibility of placing a second zygomatic implant if ever needed in the future. With the patient’s right side adequately supported, attention was now turned to the left maxilla. Following PATZI, a left pterygoid implant was attempted first but without success.

With the (P) of PATZI unsatisfied, algorithm progression next dictated attempts at anterior implant placement. With bone thickness as low as 0.8 mm in the anterior left maxilla, placement of standard, nasal rim, and piriform rim implants was not possible. Evaluation of the patient’s prelacrimal recess revealed a Simmen Class 3 relationship to the nasolacrimal duct, but minimal bone thickness of only 0.9 mm precluded placement of a transnasal implant. Failure to satisfy (A) of PATZI called for placement of an anterosuperior zygomatic implant. With minimal bone in the patient’s mid-maxilla, (T) of PATZI was also unsatisfied with inability to place a tilted implant. As tilted implant placement was not possible, a posteroinferior zygomatic implant was indicated. With the additional consideration that (P) of PATZI was also unsatisfied on the patient’s left side, zygomatic implants in an “A-Frame” configuration were required to maximize AP prosthetic spread. With a composite torque value exceeding 350 Ncm, the patient’s maxilla was immediately restored with a transitional restoration which was matched to fit an implant supported restoration in the mandible. The patient healed uneventfully and was pleased with the outcome (Figures 7-12).
Case 3
A 52-year-old male presented for full arch immediate implant treatment of the maxilla and mandible. Presurgical radiographic analysis revealed multiple missing teeth and localized areas of infection in the remaining dentition. Infection around the left maxillary canine was particularly concerning as a significant amount of bone was missing in this area. Both maxillary sinuses were pneumatized posteriorly, but the pterygomaxillary complexes demonstrated dense bone of standard dimensions. The mandible contained multiple missing teeth and exhibited a horizontal periodontal bone loss pattern similar to that of the maxilla.
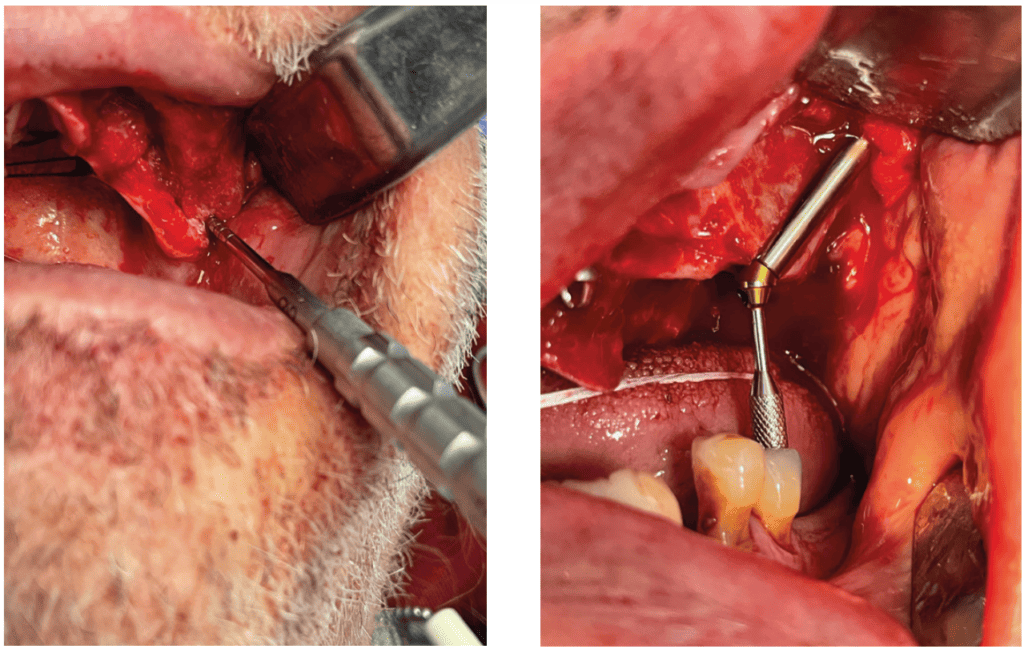
Following the administration of intravenous sedation, local anesthetic was applied intraorally, and an incision was employed from the left to right maxillary tuberosity. Following elevation of a full thickness mucoperiosteal flap, all teeth were removed and their sockets degranulated. Following the PATZI protocol, a pterygoid implant was first placed on the patient’s right side with extremely high insertion torque. With (P) of PATZI satisfied, an anterior implant was next placed in the area of the right lateral incisor, and a tilted implant was next placed in the right premolar region to accommodate (T). On the patient’s left side, the process repeated with a pterygoid implant placed first. With (P) of PATZI accommodated, an anterior implant was placed in the socket of the left central incisor. The large amount of bone loss associated with the left maxillary canine and the pneumatized left maxillary sinus precluded placement of a tilted implant. With (T) of PATZI unsatisfied, the algorithm called for placement of a posteroinferior zygomatic implant. Using the extrasinus slot technique, a 4.2 mm x 42.5 mm zygomatic fixture was placed with extremely high insertion torque. With a cumulative torque value of 300+ Ncm, the maxilla was immediately restored with a transitional restoration. The mandible was subsequently treated in a similar fashion to the maxilla. The patient healed uneventfully and was satisfied with the outcome (Figures 13-18).
Conclusion
Immediately loaded full arch treatment has a 20-year history with extremely high documented success.12,26-30 While standard All-On-4™ style implant treatment has been a readily accepted protocol, it is not applicable to all maxillary situations such as those with severe atrophy. The PATZI protocol employs a combination of standard and remote anchorage implant techniques to tackle any situation that may present in the atrophic maxilla. Additionally, this systematic algorithm allows for rapid treatment planning and the option for real-time changes based on intrasurgical outcomes. PATZI is an advanced protocol that requires the user to have full command of complex surgical techniques such as pterygoid, zygomatic, and transnasal implants. Without these implant styles, PATZI cannot be employed.
Dr. Dan Holtzclaw has much experience with the PATZI protocol and the issues that may arise. Watch his webinar on Full Arch and Remote Anchorage Implant Complications and how to deal with them. https://implantpracticeus.com/webinars/full-arch-and-remote-anchorage-implant-complications/
References
- Linkow L. A Dynamic Approach to Oral Implantology Maxillary Implants. North Haven, Connecticut: Glarus; 1977.
- Balshi TJ, Lee HY, Hernandez RE. The use of pterygomaxillary implants in the partially edentulous patient: a preliminary report. Int J Oral Maxillofac Implants. 1995 Jan-Feb; 10(1):89-98.
- Parel SM, Brånemark PI, Ohrnell LO, Svensson B. Remote implant anchorage for the rehabilitation of maxillary defects. J Prosthet Dent. 2001 Oct;86(4):377-381.
- Lopes A, de Araújo Nobre M, Ferro A, Moura Guedes C, Almeida R, Nunes M. Zygomatic Implants Placed in Immediate Function through Extra-Maxillary Surgical Technique and 45 to 60 Degrees Angulated Abutments for Full-Arch Rehabilitation of Extremely Atrophic Maxillae: Short-Term Outcome of a Retrospective Cohort. J Clin Med. 2021 Aug 16;10(16):3600.
- Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000 Nov-Dec;15(6):889-893.
- Aleksandrowicz P, Kusa-Podka´nska M, Grabowska K, Kotuła L, Szkatuła-Łupina A, Wysoki´nska-Miszczuk J. Extra-Sinus Zygomatic Implants to Avoid Chronic Sinusitis and Prosthetic Arch Malposition: 12 Years of Experience. J Oral Implantol. 2019 Feb;45(1):73-78. Epub 2018 Aug 3.
- Aparicio C, Polido WD, Zarrinkelk HM. The Zygoma Anatomy-Guided Approach for Placement of Zygomatic Implants. Atlas Oral Maxillofac Surg Clin North Am. 2021 Sep;29(2):203-231.
- Aparicio C, Manresa C, Francisco K, Aparicio A, Nunes J, Claros P, Potau JM. Zygomatic implants placed using the zygomatic anatomy-guided approach versus the classical technique: a proposed system to report rhinosinusitis diagnosis. Clin Implant Dent Relat Res. 2014 Oct;16(5):627-642.
- Aparicio C, Ouazzani W, Hatano N. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontol 2000. 2008;47:162-171.
- Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000 Nov-Dec;15(6):889-893.
- Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants. 2003 Nov-Dec;18(6):902-904.
- Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2-9.
- Aparicio C, Ouazzani W, Aparicio A, Fortes V, Muela R, Pascual A, Codesal M, Barluenga N, Franch M. Immediate/Early loading of zygomatic implants: clinical experiences after 2 to 5 years of follow-up. Clin Implant Dent Relat Res. 2010 May;12 Suppl 1:e77-82.
- Aparicio C, Manresa C, Francisco K, Ouazzani W, Claros P, Potau JM, Aparicio A. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014 Jun;16(3):447-459.
- Aparicio C, Manresa C, Francisco K, Claros P, Alández J, González-Martín O, Albrektsson T. Zygomatic implants: indications, techniques and outcomes, and the zygomatic success code. Periodontol 2000. 2014 Oct;66(1):41-58.
- Quintana R, Aparicio C. ¿Qué indicaciones tienen y qué resultados nos ofrecen los Implantes Cigomáticos? (What are then indications of the zygomatic fixture and what results do they offer us?) Cient Dent. April 2008;5(1):73-84 (Spanish).
- Aparicio C, Ouazzani W, Hatano N. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontol 2000. 2008;47:162-171.
- Holtzclaw D. Pterygoid Fixated Arch Stabilization Technique (PFAST): A Retrospective Study of Pterygoid Dental Implants used for Immediately Loaded Full Arch Prosthetics. J Implant Adv Clin Dent. 2018;10(7):6-17.
- Holtzclaw D. Pterygoid Dental Implants: The Art and Science. Austin, Texas: DIA Management Services; 2020.
- Holtzclaw D. Remote Anchorage Solutions for Severe Maxillary Atrophy: Zygomatic, Pterygoid, Transnasal, Nasal Rim, Piriform Rim, Nasopalatine, and Trans-Sinus Dental Implants. Austin, Texas: Zygoma Partners; 2023.
- Jensen OT, Adams MW, Butura C, Galindo DF. Maxillary V-4: Four implant treatment for maxillary atrophy with dental implants fixed apically at the vomer-nasal crest, lateral pyriform rim, and zygoma for immediate function. Report on 44 patients followed from 1 to 3 years. J Prosthet Dent. 2015 Dec;114(6):810-817.
- Urban I, Jovanovic SA, Buser D, Bornstein MM. Partial lateralization of the nasopalatine nerve at the incisive foramen for ridge augmentation in the anterior maxilla prior to placement of dental implants: a retrospective case series evaluating self-reported data and neurosensory testing. Int J Periodontics Restorative Dent. 2015 Mar-Apr;35(2):169-177.
- Lorean A, Mazor Z, Barbu H, Mijiritsky E, Levin L. Nasal floor elevation combined with dental implant placement: a long-term report of up to 86 months. Int J Oral Maxillofac Implants. 2014 May-Jun;29(3):705-708.
- Camargo VB, Baptista D, Manfro R. Implante transnasal (Técnica Vanderlim) como opção ao segundo implante zigomático. Coppedê A. Soluções clínicas para reabilitações totais sobre implantes sem enxertos ósseos. 2019:198–214. São Paulo: Quintessence.
- Jensen OT, Cottam J, Ringeman J, Adams M. Trans-sinus dental implants, bone morphogenetic protein 2, and immediate function for all-on-4 treatment of severe maxillary atrophy. J Oral Maxillofac Surg. 2012 Jan;70(1):141-148.
- Soto-Penaloza D, Zaragozí-Alonso R, Penarrocha-Diago M, Penarrocha-Diago M. The all-on-four treatment concept: Systematic review. J Clin Exp Dent. 2017 Mar 1;9(3):e474-e488.
- Maló P, de Araújo Nobre M, Lopes A, Ferro A, Nunes M. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5-13 years of follow-up. Clin Implant Dent Relat Res. 2019 Aug;21(4):538-549.
- Tironi F, Orlando F, Azzola F, Vitelli C, Francetti LA. Implants Placed with the All-On-4 Technique: A Radiographic Retrospective Study on 156 Implants with a 5- to 14-Year Follow-up. Int J Periodontics Restorative Dent. 2023 Sep-Oct;43(5):606-613.
- de Araújo Nobre M, Lopes A, Antunes E. The 10 Year Outcomes of Implants Inserted with Dehiscence or Fenestrations in the Rehabilitation of Completely Edentulous Jaws with the All-on-4 Concept. J Clin Med. 2022 Mar 31;11(7):1939.
- Maló P, Araújo Nobre MD, Lopes A, Rodrigues R. Double Full-Arch Versus Single Full-Arch, Four Implant-Supported Rehabilitations: A Retrospective, 5-Year Cohort Study. J Prosthodont. 2015 Jun;24(4):263-270. Simmen D, Veerasigamani N, Briner HR, Jones N, Schuknecht B. Anterior maxillary wall and lacrimal duct relationship – CT analysis for prelacrimal access to the maxillary sinus. 2017 Jun 1;55(2):170-174.
- Wang H, Hung K, Zhao K, Wang Y, Wang F, Wu Y. Anatomical analysis of zygomatic bone in ectodermal dysplasia patients with oligodontia. Clin Implant Dent Relat Res. 2019 Apr;21(2):310-316.
- Hung KF, Ai QY, Fan SC, Wang F, Huang W, Wu YQ. Measurement of the zygomatic region for the optimal placement of quad zygomatic implants. Clin Implant Dent Relat Res. 2017 Oct;19(5):841-848.
- Rigolizzo MB, Camilli JA, Francischone CE, Padovani CR, Brånemark PI. Zygomatic bone: anatomic bases for osseointegrated implant anchorage. Int J Oral Maxillofac Implants. 2005 May-Jun;20(3):441-447.
- Saltagi MZ, Schueth E, Nag A, Rabbani C, MacPhail ME, Nelson RF. The Effects of Age and Race on Calvarium, Tegmen, and Zygoma Thickness. J Craniofac Surg. 2021 Jan-Feb 01;32(1):345-349.
- Nkenke E, Hahn M, Lell M, Wiltfang J, Schultze-Mosgau S, Stech B, Radespiel-Tröger M, Neukam FW. Anatomic site evaluation of the zygomatic bone for dental implant placement. Clin Oral Implants Res. 2003 Feb;14(1):72-79.
- Nkenke E, Hahn M, Lell M, Wiltfang J, Schultze-Mosgau S, Stech B, Radespiel-Tröger M, Neukam FW. Anatomic site evaluation of the zygomatic bone for dental implant placement. Clin Oral Implants Res. 2003 Feb;14(1):72-79.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Dan Holtzclaw, DDS, MS, is Chief Clinical Officer of Advanced Dental Implant Centers and Director of Fixed Arch Services at Affordable Care, LLC, Morrisville, North Carolina. He is a Diplomate of the American Board of Periodontology and Diplomate of the International Congress of Oral Implantologists. Dr. Holtzclaw has published more than 60 articles in peer reviewed journals in addition to multiple textbooks. He served as the Editor-In-Chief of the Journal of Implant and Advanced Clinical Dentistry for 13 years in addition to serving as an editorial board member and/or editorial reviewer for several other dental journals.
Dan Holtzclaw, DDS, MS, is Chief Clinical Officer of Advanced Dental Implant Centers and Director of Fixed Arch Services at Affordable Care, LLC, Morrisville, North Carolina. He is a Diplomate of the American Board of Periodontology and Diplomate of the International Congress of Oral Implantologists. Dr. Holtzclaw has published more than 60 articles in peer reviewed journals in addition to multiple textbooks. He served as the Editor-In-Chief of the Journal of Implant and Advanced Clinical Dentistry for 13 years in addition to serving as an editorial board member and/or editorial reviewer for several other dental journals.

