Drs. Roberto Rossi, Ulf Nannmark, Andrea Pilloni, and Nino Squadrito, CDT, demonstrate how to preserve and condition the soft tissue with a combined approach
 Periodontal disease is often responsible for the loss of attachment around teeth and therefore a major cause of ridge deficiency after the teeth are extracted. The world has become more and more aware of esthetics in dentistry, and any procedure aimed to preserve the hard and soft tissue becomes useful to satisfy the needs of increasingly demanding patients.
Periodontal disease is often responsible for the loss of attachment around teeth and therefore a major cause of ridge deficiency after the teeth are extracted. The world has become more and more aware of esthetics in dentistry, and any procedure aimed to preserve the hard and soft tissue becomes useful to satisfy the needs of increasingly demanding patients.
This article will present a case of advanced periodontitis treated with a ridge preservation technique and later planned and finalized with the use of guided implant surgery, immediate loading, and thus, soft tissue conditioning in order to minimize the effects of the disease.
The literature
Tooth loss in many cases is one of the primary causes of alveolar bone remodeling and loss. Schropp and colleagues showed the changes in the soft and hard tissues after teeth extraction in clinical and radiographic prospective study (2003).
The tissue changes after removal of a premolar or a molar in 46 patients were evaluated over a period of 12 months by measuring study casts, linear radiographic analysis, and subtraction radiography. Their results showed that the major changes occurred during 1 year after extraction.
Jahangiri and colleagues reviewed the understanding of the biology of tooth extraction, wound healing, and residual ridge remodeling (1988). Defects in socket matrix formation or cellular activity will lead to stalled healing. The review of residual ridge remodeling describes the long-term result of tooth extraction and formation of residual ridges in which the quantity of bone tissue continuously decreases. The authors suggested that any potential regulatory factor of residual ridge resorption should have an adverse effect either on the increased catabolic activity by osteoclasts or on the decreased anabolic activity by osteoblasts.
A recent study by Barone and colleagues described the tissue changes of extraction sockets with a comparison of spontaneous healing versus a ridge preservation technique with secondary soft tissue healing (2013). The study group was treated with careful extraction and insertion of corticocancellous porcine bone and a collagen membrane, while the control sites received only sutures to stabilize the blood clot. Test sites showed a vertical bone remodeling of 0.3 ± 0.76 mm, 1.1 ± 0.96 mm, and 0.9 ± 0.98 mm at the mesial, buccal, and distal sites, while the control group showed a remodeling of 1 ± 0.7 mm, 2.1 ± 0.6 mm, and 1 ± 0.8 mm at the same sites. Horizontal changes were 3.6 ± 0.72 mm in the control sites and 1.6 ± 0.55 mm in the study group.
This study concluded that alveolar ridge preservation technique performed with
collagenated porcine bone graft and a resorbable membrane was able to limit the contour changes after tooth extraction. Another important issue was that test sites showed a better preservation of facial keratinized gingiva when compared to control sites. Also, grafted sites allowed the placement of longer implants and wider implants when compared to non-grafted sites.
In 2008, Allegrini and colleagues reviewed the literature on socket preservation and concluded that the maintenance of the alveolar bone after extraction depends on a careful surgical procedure and the use of a biomaterial capable of maintaining the prior space, which is helpful in bone tissue healing.
In 2012, Lindhe and colleagues evaluated an important factor: changes in the pattern of bone resorption in periodontitis and non-periodontitis subjects. The paper was to discuss the tissue of the fully healed extraction sites in patients who had lost teeth as a result of periodontal disease or from other causes. This study indicated that the edentulous posterior maxilla was comprised of 58% lamellar bone, 15% woven bone, 7% osteoid, and 10% bone marrow. More than 50% was mineralized bone. Also, Vignoletti and colleagues presented a systematic review of the surgical protocols for ridge preservation after tooth extraction (2012).
Fourteen publications on PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) were evaluated, each looking at randomized controlled clinical trials and prospective cohort studies with a follow-up of at least 3 months reporting on changes on both the hard and soft tissue (height and width) of the alveolar process (mm or %) after tooth extraction (up to February 2012). Data from nine of these 14 studies were grouped in the meta-analysis. The results showed a statistically significant greater ridge reduction in bone height for control groups as compared to test groups and a significant greater reduction in bone width for control groups.
The authors concluded that the potential benefit of socket preservation therapies is demonstrated in less vertical and horizontal resorption of the alveolar bone crest. The scientific evidence does not provide clear guidelines in regard to the type of biomaterial, or surgical procedure, although a significant positive effect of the flapped surgery was observed. After the ridge preservation has been performed, a study suggested a protocol for planning and treating such cases with guided implant surgery (Rossi, et al., 2010).
The authors showed how the combination of presurgical computed planning and immediate loading might lead to excellent soft tissue conditioning and minimal surgical traumatism for the hard and soft tissue, and this could be helpful in the maintenance and/or development of interproximal papille.
Case presentation
A 32-year-old female patient presented with signs of severe periodontitis, a perio-dontal probing depth of more than 6 mm, bleeding on probing, and periodontal screening and recording (PSR) of four in the molar areas. The area in the first quadrant was elected to be treated with extractions and simultaneous bone grafting for ridge preservation (Figure 1).

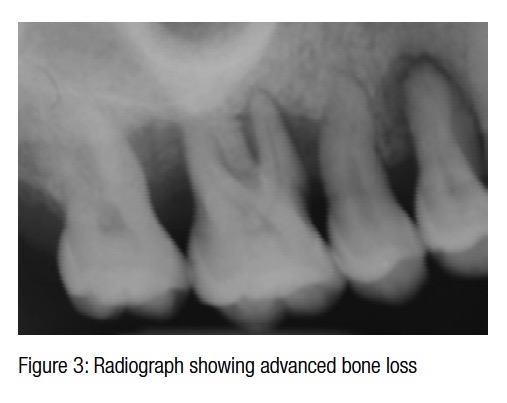 The periapical radiograph of the quadrant shows pockets up to 12 mm on the first bicuspid, 8 mm on the distal of the second bicuspid, and 9 mm and 10 mm on the mesial and distal of the first molar. The teeth were healthy and did not have any cavities (Figures 2-3). Bone loss was reaching around the apex of the roots of the first bicuspid and the first molar, and the mobility was 2+. Local anesthesia is first administered with a computerized controlled device (Single Tooth Anesthesia, STA™, Milestone Scientific, Inc.) with articaine with epinephrine 1:200.000.
The periapical radiograph of the quadrant shows pockets up to 12 mm on the first bicuspid, 8 mm on the distal of the second bicuspid, and 9 mm and 10 mm on the mesial and distal of the first molar. The teeth were healthy and did not have any cavities (Figures 2-3). Bone loss was reaching around the apex of the roots of the first bicuspid and the first molar, and the mobility was 2+. Local anesthesia is first administered with a computerized controlled device (Single Tooth Anesthesia, STA™, Milestone Scientific, Inc.) with articaine with epinephrine 1:200.000.
 Once the teeth and the surrounding soft tissue were anesthetized, the teeth were separated from the gingiva with a microblade and later extracted (Figure 4). The granulation tissue on the extraction sockets was carefully curetted, and the sockets were first irrigated with chlorhexidine and later grafted with corticocancellous collagenated porcine bone graft (Figure 5) (mp3, Osteobiol®).
Once the teeth and the surrounding soft tissue were anesthetized, the teeth were separated from the gingiva with a microblade and later extracted (Figure 4). The granulation tissue on the extraction sockets was carefully curetted, and the sockets were first irrigated with chlorhexidine and later grafted with corticocancellous collagenated porcine bone graft (Figure 5) (mp3, Osteobiol®).
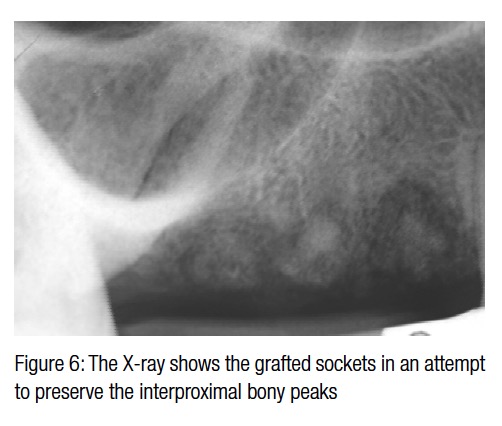
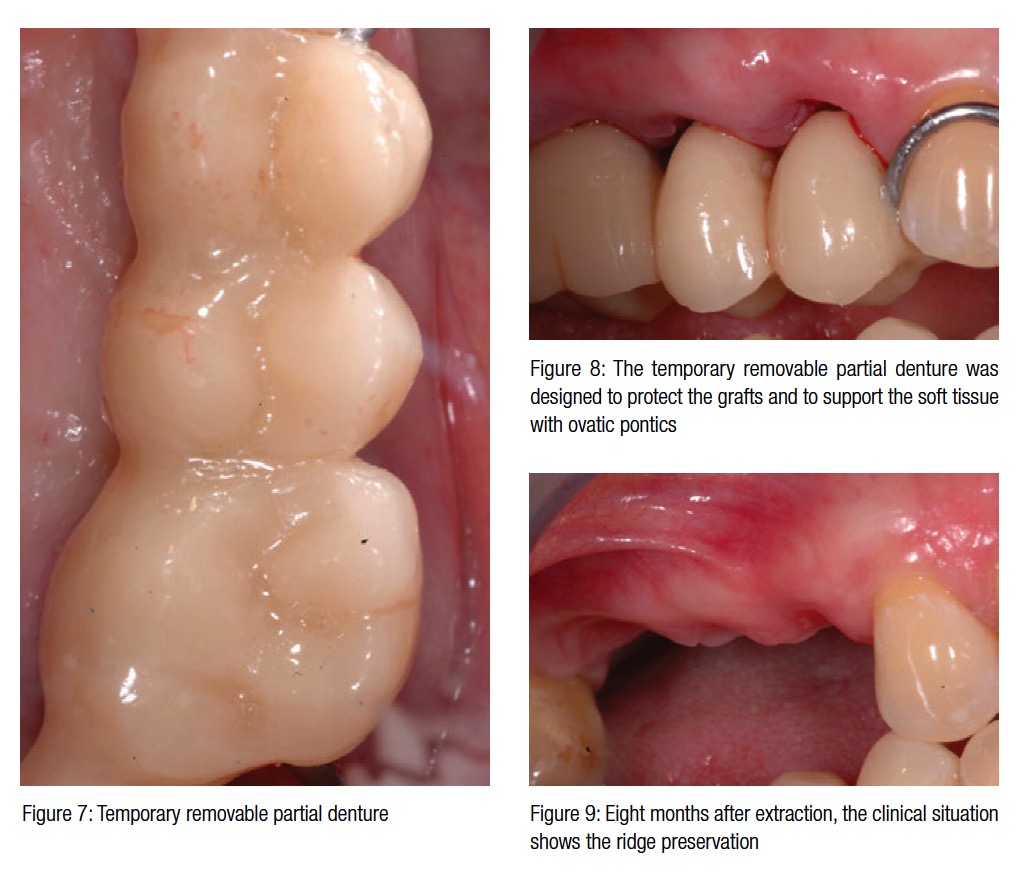
The periapical radiograph shows the attempt to completely fill up the residual sockets (Figure 6). The simultaneous application of a removable partial denture (Figures 7-8) with ovatic pontics had the goals of, first, sealing the grafted sockets and, second, supporting the soft tissue in an attempt to preserve a scalloped gingival architecture. The re-evaluation at 8 months (Figure 9) shows how the temporary denture helped guide the healing, protecting the bone grafts and also maintaining the natural scalloped architecture.
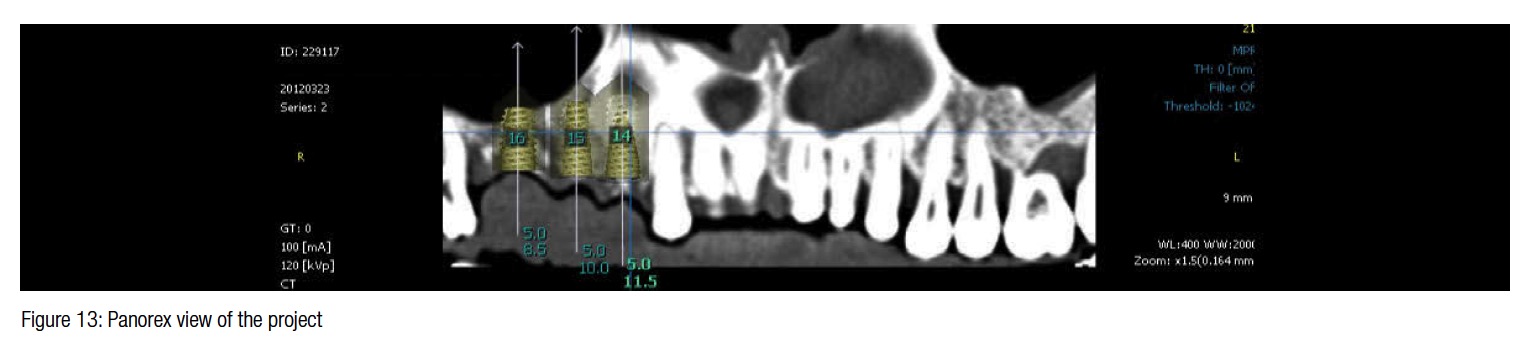
 At this point, the case was studied with a navigation system (OsstemGuide™, Hiossen Osstem), and the treatment plan was to place three dental implants in place of the roots of the teeth previously removed. The case analysis shows how the ridge preservation and integration of the bone grafts allowed the placement of three implants of 5 mm diameter (Figures 10-13).
At this point, the case was studied with a navigation system (OsstemGuide™, Hiossen Osstem), and the treatment plan was to place three dental implants in place of the roots of the teeth previously removed. The case analysis shows how the ridge preservation and integration of the bone grafts allowed the placement of three implants of 5 mm diameter (Figures 10-13).

The surgical guide was created using computer technology and verified prior to the surgical appointment. On the day of surgery, the protocol calls for stabilization of the surgical guide on the residual teeth but with some flow composite on the upper right canine. The width of the crest was maintained after extractions and with a ridge preservation technique. To further enhance the chance for soft tissue conditioning, only a small core of connective tissue and epi-thelium was removed with a tissue punch prior to implant insertion (Figures 14-16).

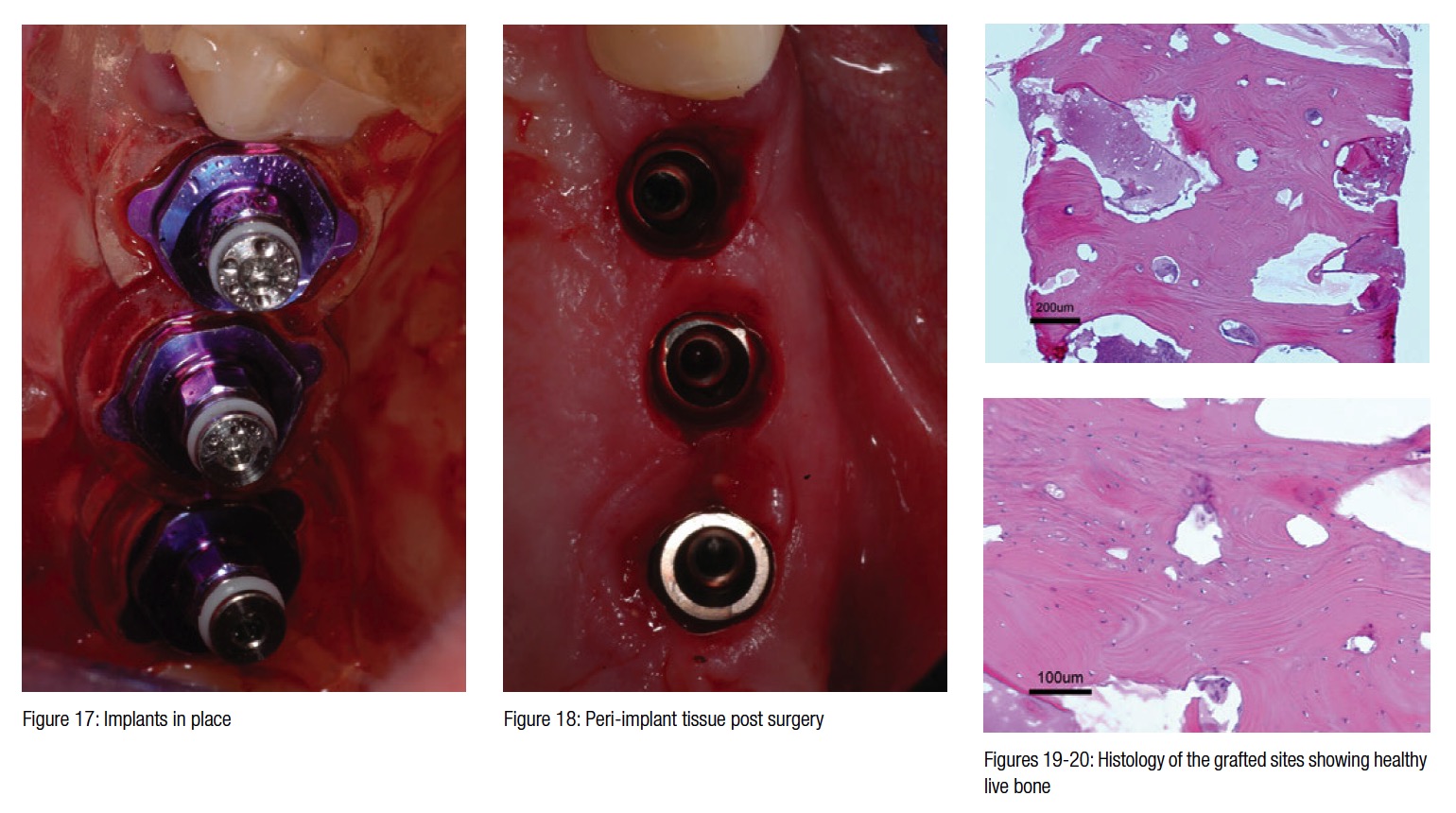
At the time of surgery, three biopsies were taken from the previously grafted sites, and histomorphometric analysis showed new vital bone in place of the graft previously placed. Figure 19 shows the entire biopsy at X4 magnification; bone trabeculae can be seen in almost all parts of the section, but also remnants of the biomaterial. The middle part of the section consists of soft tissue, a combination of mostly yellow bone marrow with small islands of red marrow (hematoxylin-
eosin staining).
Figure 20 shows part of the previous section at a higher magnification (X20). The bone tissue is well organized and well supplied by blood vessels. In the upper left, a part of biomaterial can still be seen in between the bone and the soft tissue. In the right upper corner, a small piece of bio-material is totally surrounded by bone. No signs of inflammation can be seen in the soft or hard tissue (Figures 19-20).


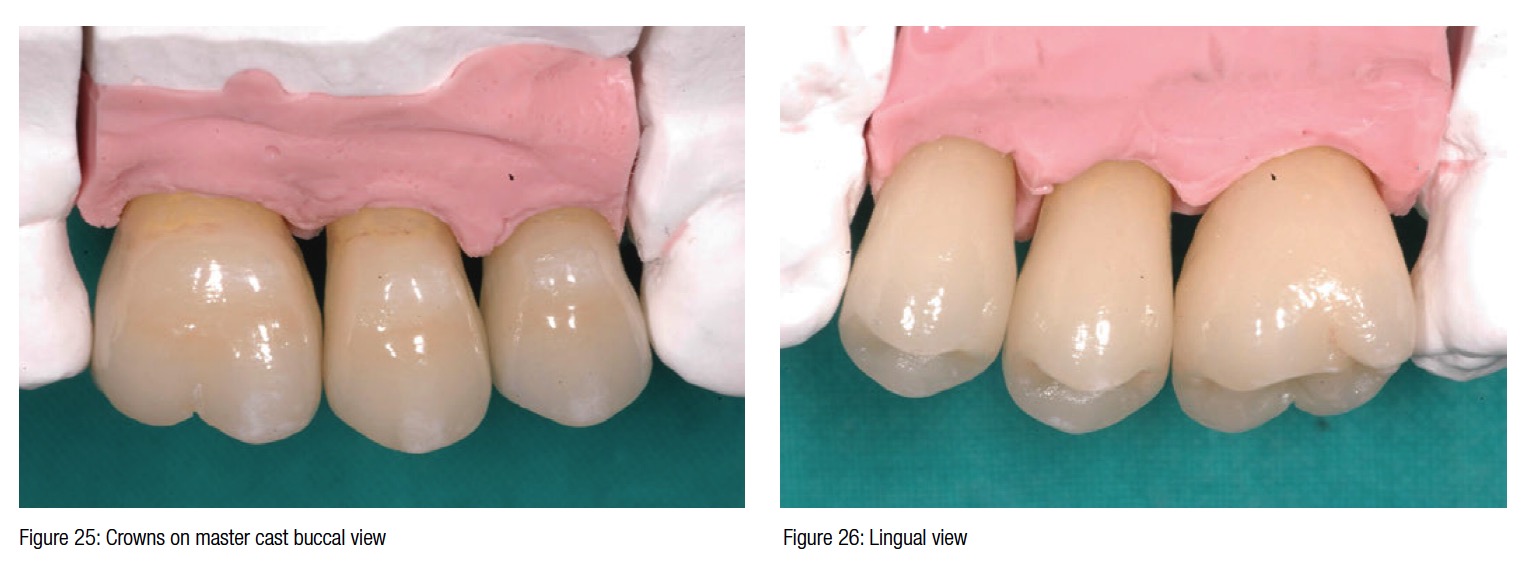
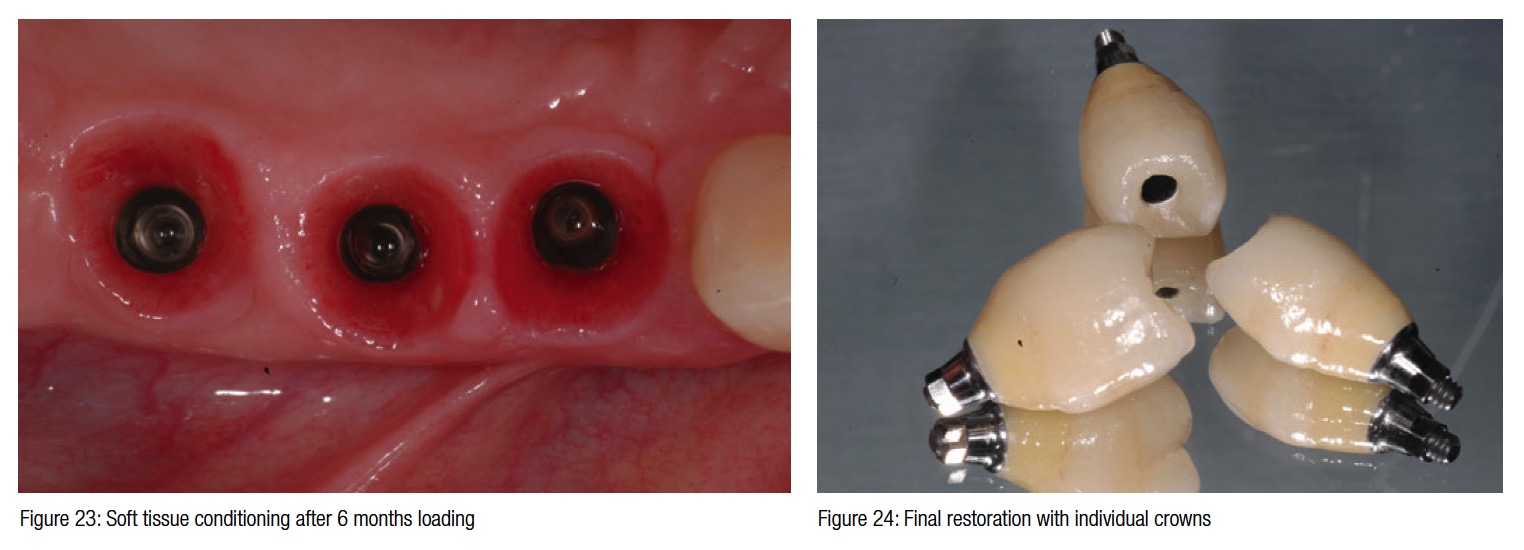
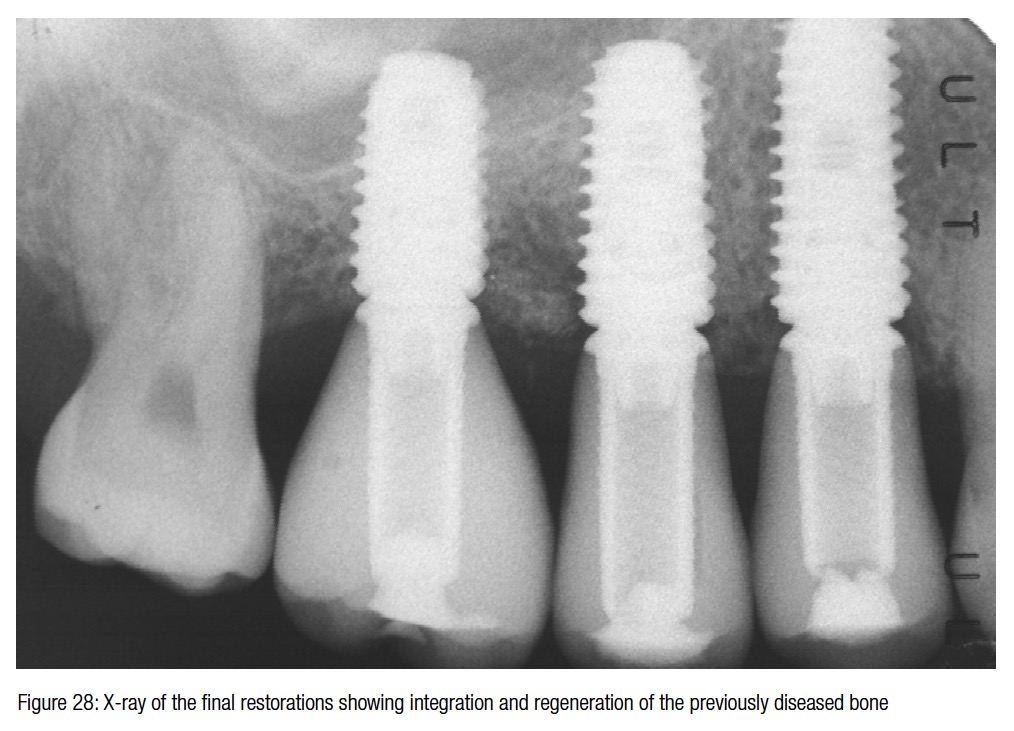
The surgical trauma was very minimal, and the possibility to install a temporary bridge on the implants on the same day further enhanced the chances of conditioning the peri-implant soft tissue (Figure 21). The post-surgical X-ray shows the precision and the perfect abutment to implant connection. Six months later in a follow-up visit, the temporary bridge was removed to reveal the ridge preservation and the soft tissue conditioning. At this time, three individual crowns were fabricated and delivered to replace the missing teeth and showing excellent color, shape, and soft-tissue integration (Figures 24-27). The radiograph taken a year and a half after teeth extraction shows the amount of regeneration and the sustained osseointegration.
Conclusion
Esthetics are becoming more and more important in modern dentistry, and the
preservation of the soft and hard tissue is one of the primary goals. Any time we ran into cases of advanced or aggressive periodontitis where the bone loss and the PSR was four, we noticed a severe collapse of the soft tissue as a consequence of the advanced bone loss.

Modern periodontal and implant literature became very aware of this problem, and many different techniques have been introduced to solve and minimize this problem (Jahangiri, et al., 1988; Allegrini, et al., 2008; Lindhe, et al., 2012; Vignoletti, et al., 2012; Ladsberg and Bichacho, 1994; Kutkut, Andreana, and Monaco, 2012).
 Many different authors have presented similar protocols with different bio-materials, from autogenous bone, to allografts, to synthetic and xenografts, but all of these procedures, despite using different materials, share a similar goal of minimizing the collapse of the soft and hard tissue and thus trying to preserve the natural esthetics (Horowitz, Holtzclaw, and Rosen, 2012; Horvath, et al., 2013; Scheyer, Schupbach, and McGuire, 2012; Pagni, et al., 2012; Cardaropoli, et al., 2012; Hämmerle, et al., 2012).
Many different authors have presented similar protocols with different bio-materials, from autogenous bone, to allografts, to synthetic and xenografts, but all of these procedures, despite using different materials, share a similar goal of minimizing the collapse of the soft and hard tissue and thus trying to preserve the natural esthetics (Horowitz, Holtzclaw, and Rosen, 2012; Horvath, et al., 2013; Scheyer, Schupbach, and McGuire, 2012; Pagni, et al., 2012; Cardaropoli, et al., 2012; Hämmerle, et al., 2012).
The relationship between the height of the interproximal bone peak and the teeth’s contact point has been well described in the literature (Nordland and Tarnow, 1988); therefore, the maintenance or reconstruction of the bone in that area becomes of paramount importance in supporting the soft tissue and, thus, esthetics. A combination of ridge preservation techniques with subsequent guided implant surgery will reduce the surgical trauma to the soft tissue, help condition the interproximal areas from baseline, and the use of immediate crowns with proper anatomical shapes will help conditioning the peri-implant soft tissue after also supporting its maturation (Rossi, et al., 2012).
Since dentistry is moving forward into esthetics, a protocol that will help restore the hard tissue in cases of aggressive perio-dontitis will also help in the preservation and improvement of the soft tissue, giving clinicians a new therapeutic option.
References
- Allegrini S Jr, Koening B Jr, Allegrini MR, Yoshimoto M, Gedrange T, Fanghaenel J, Lipski M. Alveolar ridge socket preservation with bone grafting – review. Ann Acad Med Stetin. 2008;54(1):70-81.
- Barone A, Ricci M, Tonelli P, Santini S, Covani U. Tissue changes of extraction sockets in humans: a comparison of spontaneous healing vs. ridge preservation with secondary soft tissue healing. Clin Oral Implants Res. 2013;24(11):1231-1237.
- Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: a randomized controlled clinical trial with histologic analysis. Int J Periodontics Restorative Dent. 2012;32(4):421-430.
- Hämmerle CH, Araújo MG, Simion M, Osteology Consensus Group 2011. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res. 2012;23(suppl 5):80-82.
- Horowitz R, Holtzclaw D, Rosen PS. A review on alveolar ridge preservation following tooth extraction. J Evid Based Dent Pract. 2012;12(suppl 3):149-160.
- Horváth A, Mardas N, Mezzomo LA, Needleman IG, Donos N. Alveolar ridge preservation. A systematic review. Clin Oral Investig. 2013;17(2):341-363.
- Jahangiri L, Devlin H, Ting K, Nishimura I. Current perspectives in residual ridge remodeling and its clinical implications: a review. J Prosthet Dent. 1988;80(2):224-237.
- Kutkut A, Andreana S, Monaco E. Esthetic consideration for alveolar socket preservation prior to implant placement: description of a technique and 80-case series report. Gen Dent. 2012;60(6):e398-403.
- Landsberg CJ, Bichacho N. A modified surgical/prosthetic approach for optimal single implant supported crown. Part I – The socket seal surgery. Pract Periodontics Aesthet Dent. 1994;6(2):11-17, 19.
- Lindhe J, Cecchinato D, Bressan EA, Toia M, Araújo MG, Liljenberg B. The alveolar process of the edentulous maxilla in periodontitis and non-periodontitis subjects. Clin Oral Implants Res. 2012;23(1):5-11.
- Nordland WP, Tarnow DP. A classification system for loss of papillary height. J Periodontol. 1998;69(10):1124-1126.
- Pagni G, Pellegrini G, Giannobile WV, Rasperini G. Postextraction alveolar ridge preservation: biological basis and treatment. Int J Dent. 2012;2012:151030.
- Rossi R, Morales RS, Frascaria M, Benzi R, Squadrito N. Planning implants in the aesthetic zone using a new implant 3D navigation system. Eur J Esthet Dent. 2010;5(2):172-188.
- Scheyer ET, Schupbach P, McGuire MK. A histologic and clinical evaluation of ridge preservation following grafting with demineralized bone matrix, cancellous bone chips, and resorbable extracellular matrix membrane. Int J Periodontics Restorative Dent. 2012;32(5):543-552.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323.
- Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res. 2012;23(suppl 5):22-38.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores


