Drs. Lira Rahman, Jacobus Hercules van den Heever, and Andre W. van Zyl present the application of guided dental implant surgery in prevention of inferior alveolar nerve damage in a patient with compromised bone
Introduction
 Iatrogenic injuries to the inferior alveolar nerve (IAN) can impact significantly on patients’ lives. Altered sensation and pain in the orofacial region may interfere with speaking, eating, kissing, shaving, applying makeup, tooth brushing, drinking, and just about every social interaction (Renton, 2010).
Iatrogenic injuries to the inferior alveolar nerve (IAN) can impact significantly on patients’ lives. Altered sensation and pain in the orofacial region may interfere with speaking, eating, kissing, shaving, applying makeup, tooth brushing, drinking, and just about every social interaction (Renton, 2010).
 IAN injury is the most problematic consequence of dental surgical procedures and has major medico-legal implications (Renton, 2011).
IAN injury is the most problematic consequence of dental surgical procedures and has major medico-legal implications (Renton, 2011).
Causes of inferior alveolar nerve injury include placement of dental implants, local anesthetic injections, third molar surgery, endodontics, trauma, and orthognathic surgery.
Case history
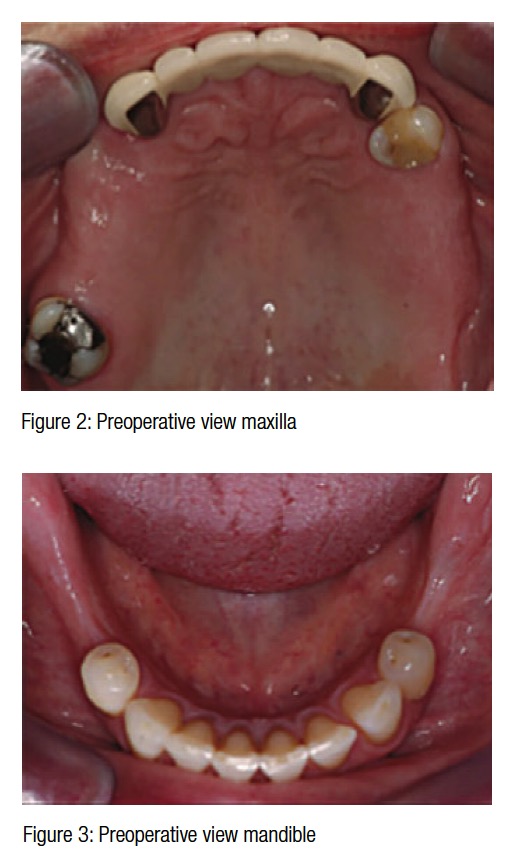
A healthy 53-year-old female patient presented with a collapsed occlusion. Her main complaints were difficulty in chewing, esthetic dissatisfaction, and a desire not to lose more teeth. Function was limited to the seven anterior teeth with no posterior support (Figures 1-3). Loss of posterior occlusion may result in the loss of neuromuscular stability of the mandible, temporomandibular joint (TMJ) dysfunction, reduced masticatory efficiency, loss of vertical dimension, and poor esthetics. Rehabilitation should aim to address all of these concerns.
 Further complications were lack of attached keratinized tissues and reduced mandibular alveolar ridge volume. Keratinized attached tissue, although a contentious topic, may have long-term benefits with regard to plaque control at the implant site (Bouri and Nouneh, 2008; Lang and Loe, 1972).
Further complications were lack of attached keratinized tissues and reduced mandibular alveolar ridge volume. Keratinized attached tissue, although a contentious topic, may have long-term benefits with regard to plaque control at the implant site (Bouri and Nouneh, 2008; Lang and Loe, 1972).
This case highlights multidisciplinary comprehensive treatment planning of a complex case using cone beam computed tomography (CBCT) and computer-designed surgical guides.
The International Team of Implantology (ITI) SAC Assessment tool determined this case as complex.
Methods and materials
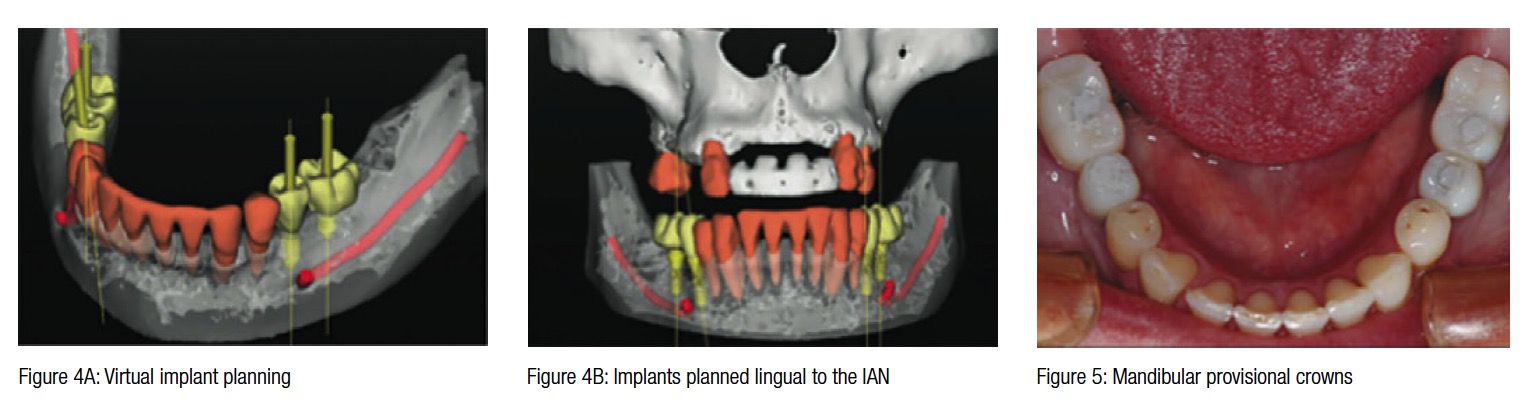
A diagnostic wax-up determined the final 3D result that could be achieved in both arches. A CBCT revealed a very thick lingual cortex with poor cancellous bone, and close proximity of the mental foramina in planned positions LL5 and LR5. Simplant® Pro (Materialise Dental) was used to create the 3D representation of the anatomical structures (Figures 4A-4B).
A stereolithographic stent (Classic SurgiGuide®, Materialise Dental) was printed from the final treatment plan. This guides the surgeon with the position and angulation of implant placement, but not placement depth.
A tooth-supported, Classic SurgiGuide was decided upon for the following reasons.
Due to the close proximity of the mental foramina to the planned implant sites in positions LL5 and LR5 and a very thick lingual cortex with almost no cancellous bone, it was planned that the implants would need to be angled toward the lingual cortex to avoid the mental foramina and the inferior alveolar nerve (IAN). It was anticipated that angling the implant lingually in a controlled manner would result in a slight deviation of the implant toward the buccal direction.
 The implication of this is that the surgeon requires a guide with a degree of “play,” which will allow him/her to make corrections during surgical placement of the implants.
The implication of this is that the surgeon requires a guide with a degree of “play,” which will allow him/her to make corrections during surgical placement of the implants.
The lack of attached keratinized tissue was addressed by performing bilateral mandibular vestibuloplasty procedures and free gingival grafts.
Straumann® Roxolid® Tissue Level Implants were placed with a 2-mm safety zone between implant and nerve (Greestein and Tarnow, 2006). Two 3.3 mm x 10 mm implants were inserted in the LL5 and LR5 sites and two 3.3 mm x 8 mm implants in the LL6 and LR6 sites using the Classic SurgiGuide. Roxolid is 50% stronger than pure titanium and shows improved integration with bone and is thus ideally suited for reduced bone situations (www.straumann.us, 2008).
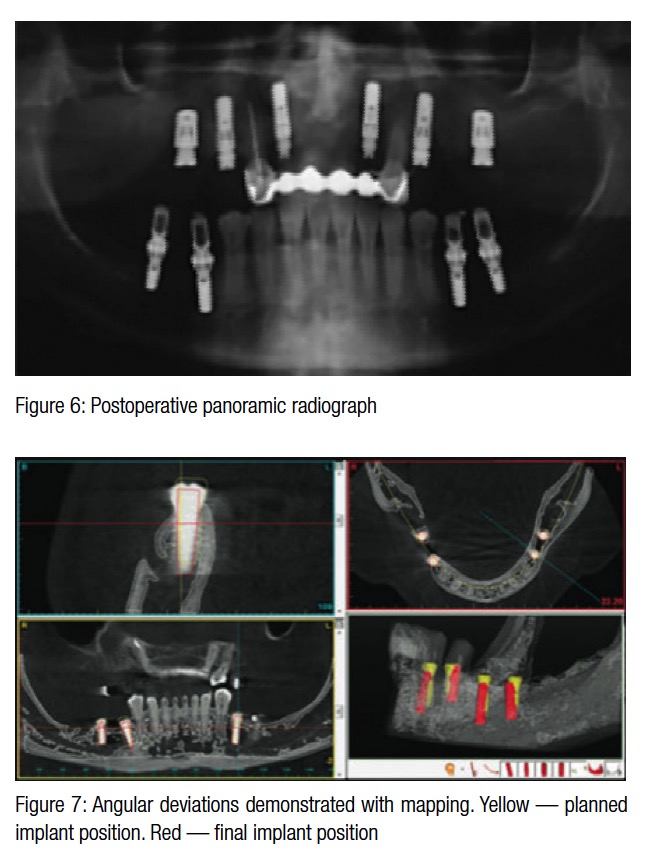
Provisional implant supported crowns are shown in Figure 5. Maxillary implants were subsequently inserted as planned (Figure 6). No postoperative nerve fallout or complications were experienced.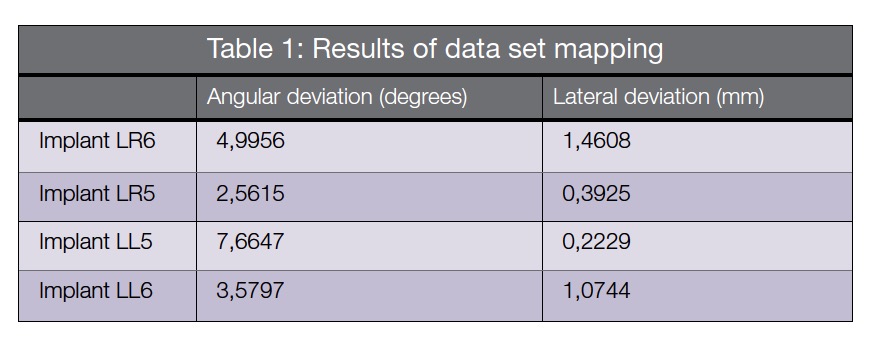
Data set mapping
A postoperative CBCT was taken and mapped with the preoperative scan to determine the correlation between planned and final implant positions (Table 1). Angular deviations of this case are within the expected deviations for Classic SurgiGuide systems (Cassetta, et al. 2013; Park, et al., 2009). The postoperative CBCT mapping of the planned and eventual positions of the implants are shown in Figure 7.
Conclusions
The preoperative planning and use of a surgical guide were beneficial in this case as it provided knowledge of the exact location of the mental foramina, IAN, alveolar ridge dimensions, and the quality and quantity of bone available. This case demonstrates the importance of correctly diagnosing complex cases using the ITI SAC Assessment tool.
The only alternative to this treatment would have been bone block augmentation in the area of the mental foramen, a procedure too risky to undertake.
Complications with such complex cases can significantly impact the lives of patients and should be approached with extreme caution by experienced clinicians only.
Acknowledgments
The authors recognize Nicolette Schroeder, Simplant S.A., and Materialise Dental (Leuven, Belgium) for assistance and contribution toward the planning of this complex case. This article was adapted from the poster, ”The application of guided dental implant surgery in prevention of inferior alveolar nerve damage in a patient with compromized bone,” which won First Prize at the ITI Congress Southern Africa 2013, July.
References
- Bouri A Jr, Bissada N, Al-Zahrani MS, Faddoul F, Nouneh I. Width of keratinized gingiva and the health status of the supporting tissues around dental Implants. Int J Oral Maxillofac Implants. 2008;23(2):323-326
- Cassetta M, Giansanti M, Di Mambro A, Calasso S, Barbato E. Accuracy of two stereolithographic surgical templates: a retrospective study. Clin Implant Dent Relat Res. 2013;15(3):448-459.
- Greestein G, Tarnow D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J Periodontol. 2006;77(12):1933-1943.
- Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontal. 1972;43(10): 623-627.
- Park C, Raigrodski AJ, Rosen J, Spiekerman C, London RM. Accuracy of implant placement using precision surgical guides with varying occlusogingival heights: An in vitro study. J Prosthet Dent. 2009;101(6):372-381.
- Renton T. Prevention of Iatrogenic Inferior Alveolar Nerve Injuries in Relation to Dental Procedures. Dent Update. 2010; 37(6):350–366.
- Renton T. Minimizing and managing nerve injuries in dental surgical procedures. Faculty Dent J. 2011;2(4):164-171.
- Gottlow J, Dard M, Kjellson F, Obrecht M, Sennerby L. Evaluation of a new titanium-zirconium implant.A biomechanical and histological comparative study in minipigs. Straumann. Study presented at Academy of Osseointegration 23rd Annual Meeting. Boston, MA. February 28-March 1 2008. https://www.straumann.us/content/dam/internet/straumann_us/resources/whitepaper/en/USLIT_285.pdf. Accessed September 17, 2015.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores


