Dr. Paresh B. Patel discusses an implant case using a tapered implant
Although single-unit cases tend to be the most straightforward of implant restorations, tooth replacement in the anterior presents a unique array of challenges, with patient anatomy and the critical importance of esthetics in the smile zone chief among them. This has led many clinicians to adopt a conservative approach to treatment or refer such cases to a more experienced practitioner.
[userloggedin]
As implant design, CAD/CAM dentistry, and treatment protocols have advanced, however, achieving a desirable outcome in the anterior has become a less complex undertaking.

The traditional approach to single tooth replacement has involved leaving the extraction site to heal prior to implantation and allowing the implant to fully osseointegrate prior to loading. Even clinicians who have opted for immediate implant placement have often been hesitant to load the implant before the healing phase is complete. But with a better understanding of the benefits of immediate implantation and provisionalization, including preservation of the hard and soft tissue that are so fundamental to an esthetic outcome, there is substantial incentive to follow a more progressive protocol when indicated.1

The progression toward more predictable results in the anterior has been aided by the advent of the tapered dental implant, which has simplified implant positioning in situations where there is limited anatomical space or bone volume. The Hahn™ Tapered Implant (Glidewell Direct; Irvine, California) takes the proven concept of an anatomically correct body shape and combines it with a pronounced thread design, which helps the clinician both situate the implant in the ideal labial-lingual position and achieve the primary stability needed for an optimal outcome. This design is ideal for immediate implantation procedures, as maintaining the proper distance from the facial plate is of paramount importance.
There are numerous advantages to immediately placing the implant following tooth extraction, including preservation of the alveolar ridge, soft tissue, and interdental papillae.2 This is crucial for cases in the anterior, where patients are more attuned to gingival contours and margins due to the visibility of soft tissue in the esthetic zone. Once the implant has been placed in the extraction site, delivering a healing abutment prevents the soft tissue from collapsing, maintaining the patient’s natural gingival architecture.3 When the primary stability of the implant is sufficient, provisionalization affords additional benefits by training the gingiva around the shape of a temporary crown, establishing more natural-looking esthetics while the tissue heals.







Immediate implantation also provides the bone with the continued stimulation it needs to mitigate the resorption that occurs in the absence of the natural tooth.4 By maintaining a maximum amount of stability and bone volume for the eventual implant restoration, this helps support an outcome that is both functional and esthetic.
The following case presentation featuring the Hahn Tapered Implant will demonstrate how immediate extraction, implantation, and provisionalization can produce a predictable, highly esthetic result in the anterior. Techniques for achieving maximum primary stability, proper labial-lingual positioning, and a natural emergence profile will be described. By following some essential guidelines, practitioners can confidently address the challenges of single tooth replacement in the esthetic zone.
Case report
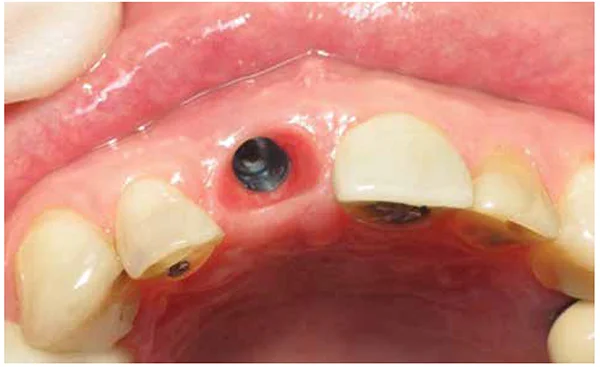
A 45-year-old female presented with a failed post-and-core crown restoration that had separated from the root of tooth No. 8 (Figure 1). An endodontist had assessed the tooth, which was stricken by recurrent decay, and provided an unfavorable prognosis for further endodontic treatment. Intraoral and radiographic evaluation indicated that the patient was an excellent candidate for immediate extraction, implantation, and temporization (Figure 2).
The patient, who did not want a conventional bridge, accepted a treatment plan for immediate tooth replacement after being presented with the restorative options. The patient found this mode of treatment appealing because it would maintain her gingival tissue and underlying bone while providing the potential for immediate provisionalization. The maxillary incisors surrounding tooth No. 8 also exhibited significant decay and would be prepared and restored with conventional crowns following completion of implant treatment per the patient’s desire to have single-unit restorations spanning teeth Nos. 7–10.
The Hahn™ Tapered Implant was selected for the procedure to ensure a maximum amount of initial stability, ease placement toward the palatal aspect of the alveolar ridge, and increase the likelihood of immediate provisionalization. The thread design of the implant is pronounced enough to thoroughly engage the bone of the extraction site, but not so pronounced that it compromises thin bone during placement or is difficult to fully seat in denser bone (Figures 3A and 3B). The tapered design of the implant would provide flexibility in positioning the implant within the available amount of bone.
At the surgical appointment, the tooth was extracted without causing any trauma to the socket site, which is crucial in this type of case, as immediate implant placement is typically contraindicated if the periodontium is compromised (Figure 4). Next, the implant osteotomy was created following a simplified surgical protocol (Figure 5). Care was taken to create an osteotomy that would situate the implant approximately 1.5 mm from the adjacent teeth and 2 mm from the facial plate, with the platform 2 mm below the adjacent CEJ (Figure 6). A 5.0 mm x 11.5 mm Hahn Tapered Implant was then threaded into place and firmly engaged the lingual wall of the socket site, helping maintain a position that was both a safe distance from the facial plate and in the ideal location for an esthetic prosthetic outcome.
The implant achieved excellent primary stability, allowing for the chairside fabrication and immediate delivery of a screw-retained provisional crown. A temporary cylinder was seated and trimmed to a height that would help keep the provisional crown out of occlusion. Then a provisional crown was fabricated with light interproximal contacts and an incisal edge approximately 1 mm out of occlusion in order to minimize the occlusal and lateral forces applied to the implant. The provisional restoration was then placed and would provide support for the soft tissue in the manner of a natural tooth throughout healing, helping contour the gingiva for an ideal outcome (Figure 7). Postoperative radiography exhibited excellent integration of the implant with the bone of the socket site (Figure 8).
Following 3 months of healing, the patient returned, so the progress of healing and osseointegration could be assessed. The screw-retained provisional was removed, revealing excellent gingival color and contours (Figure 9). Immediate provisionalization was crucial in maintaining an emergence profile that mimics that of a natural tooth. The stability of the implant was excellent. Thus, a transfer coping was seated, and final impressions were taken (Figure 10).
The lab produced master casts from the final impressions, which were scanned so they could serve as the basis for the CAD-designed custom abutment and final crown. A zirconia custom abutment with a titanium base was fabricated, and the final crown was milled from BruxZir® Anterior Solid Zirconia (Figure 11). This combination would produce ideal esthetics for the smile zone, including incisal translucency and the appearance of underlying dentin.
After receiving the case from the lab, the patient was called in for delivery of the final restoration. The custom abutment was tried in and torqued into place according to manufacturer specifications. The contours of the digitally designed custom abutment conformed precisely to the margins and sulcus form of the implant site (Figure 12). Lastly, the final crown was tried in and cemented into place, creating a natural-looking restoration that surpassed the expectations of the patient (Figure 13).
Conclusion
Immediate extraction and implantation offers a predictable approach to tooth replacement in the esthetic zone. The restorative outcome can be further enhanced by immediate provisionalization, which supports and contours the gingiva in preparation for the final crown. And because this approach reduces the total number of appointments, in addition to providing patients with an esthetic outcome, clinicians can reap the benefits of having more chair time available to see other patients.
[/userloggedin]
[userloggedout][/userloggedout]
- Noelken R, Neffe BA, Kunkel M, Wagner W. Maintenance of marginal bone support and soft tissue esthetics at immediately provisionalized OsseoSpeed implants placed into extraction sites: 2-year results. Clin Oral Implants Res. 2014;25(2):214-20.
- Guarnieri R, Ceccherini A, Grande M. Single-tooth replacement in the anterior maxilla by means of immediate implantation and early loading: clinical and aesthetic results at 5 years. Clin Implant Dent Relat Res. 2015;17(2):314-26.
- Qi Y, Zhang J, Hasi BG, Sun Y, Zhu ZH, Wang RJ. [Clinical study of healing abutment on sealing socket and preservation of the gingival natural profile in single-tooth immediate implantation]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2008;43(5):299-301.
- Covani U, Cornelini R, Calvo JL, Tonelli P, Barone A. Bone remodeling around implants placed in fresh extraction sockets. Int J Periodontics Restorative Dent. 2010;30(6):601-607.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



