Dr. Reza Faridrad presents a case using the All-on-4 concept for insufficient bone in the posterior maxilla and mandible.
It has been more than 20 years since the concept of All-on-4® (Nobel Biocare®) (Malo, Lopes, and De Araujo Nobre, 2011) has been introduced into the profession. The treatment of the resorbed edentulous jaws using a fixed implant-supported prosthesis (Malo, Lopes, and Costa, 2008) has always been a challenge for dentists.
[userloggedin]
There are still debates among the profession about the credibility of this treatment modality. Needless to say, that there are other implant companies, such as Zimmer and Bredent (fast and fixed), following the similar philosophy.
There is no doubt in my mind that the All-on-4 concept is the treatment of choice (both for me and my patients) when there is insufficient bone in the posterior maxilla and mandible (Rangert, et al., 2005; Malo, Rangert, and Nobre, 2005; Malo, Rangert, and Nobre, 2003; Malo, et al., 2011). Needless to say that the zygomatic implants and quad-zygoma options are available for more severely resorbed maxilla (when there is insufficient bone in the premolar and molar regions). These options will save time for both the patient and the operator without the need for bone-grafting procedures.
The success of All-on-4
The success and survival rate of the All-on-4 treatment has been assessed by many clinicians (Malo, et al., 2011; Malo, et al., 2011) and research groups.
Poor planning and rushing into treatment is not uncommon among the profession when it comes to edentulous jaws.
There are three types of failures:
- Short-term — during and shortly after the procedure (e.g., bleeding, lack of primary stability, etc.)
- Midterm — problems arising in the first few weeks (e.g., infection and mobility in the fixture, loosening of the internal hex screw, problems with the occlusion, poor esthetic results, etc.)
- Long term — problems arising after a few months and years (e.g., peri-implantitis and loss of hard and soft tissues, etc.).
Case study
In this case, I have tried to illustrate how the All-on-4 concept helped me to treat a patient and give her teeth, smile, and, more importantly, chewing ability back. Her previous dentist (implantologist) had decided to treat the case in a staged manner using the immediate placement protocol. Seventy-year-old Mrs. TB was referred to me for a second opinion in 2012. Mrs. TB was treated by a visiting implantologist from California, in Belgium in 2008.

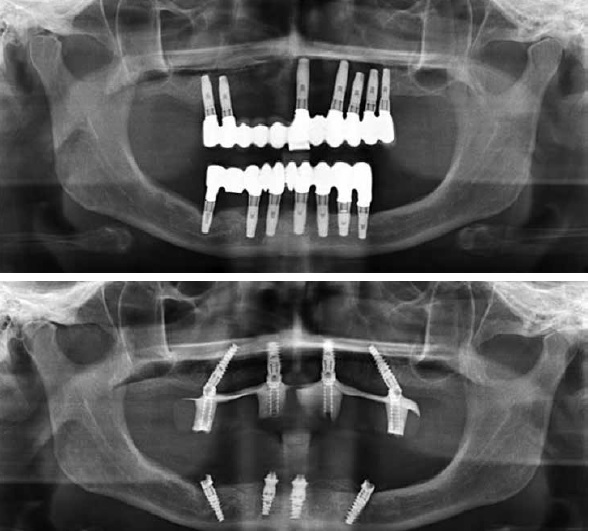
The patient presented to me with fixed-bridge restorations fitting over the 14 fixtures (unknown manufacturer), seven in the maxilla and seven in the mandible. The halitosis and poor plaque control around the fixtures with readily bleeding soft tissue around those fixtures was a horrible experience. The patient was distressed, and she was in a lot of pain and discomfort. Her chief complaint, not surprisingly, was pain, bleeding, and not being able to chew and eat properly. Nearly all the fixtures were exposed, and the bone loss was well past the first thread (Figures 1-5). There was no mobility in the bridges, but I noticed that the UL1 was looking out of place, and its shade was not matching the rest of the porcelain work. It became clear that this part was soldered onto the bridge separately. The bruxism took its toll, and the sign of it was evident on the worn down ceramic of the lower bridge occlusally (Figure 6).



An Orthopantomogram (OPG) X-ray and CBCT examinations revealed severe bone loss on the upper fixtures with poor planning for placement. It has been confirmed with the patient that these fixtures were positioned immediately in the extraction sockets for the upper left canine and premolars. In the mandible, the LR5 fixture was perforated and inserted in the right inferior dental nerve canal, and the patient already had anesthesia of the right lower lip. During all the visits the patient had with her dentist (implantologist), she was always reassured that the numbness would be temporary, that the implants and restorations were in a very good shape with minimal bone loss around them, and the dentist was actually very happy with the result.
Treatment plan
After agreeing to the proposed treatment plan, on the day of surgery, the patient had all the fixed bridgework and 14 implant fixtures removed under IV sedation. This procedure took around 7 hours as one of the upper and two of the lower fixtures were osseointegrated, and some of the heads of the internal hex screws were blunted and were already damaged. They were impossible to be undone.
The high-speed handpiece, trephine, forceps, and implant removal kit were used in order to remove all the previous restorations (Figures 7-10).
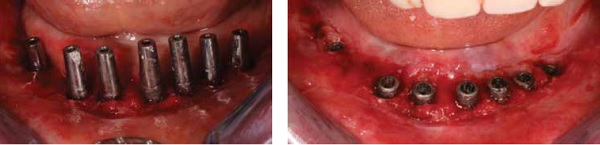


The alveolar ridge was reduced and trimmed according to the All-on-4 protocol. The fixtures (four upper and four lower) were inserted in the position LR4-5 area and angled away from the mental foramen and previously perforated ID canal. Needless to say, that the patient had some improvement in her numb lip, and she described it as “less heavy” (Figure 19).
All the created sockets and damaged ridges were augmented with Bio-Oss® (Geistlich), covered using Geistlich bilayer GBR membrane, and primary closure was achieved using Vicryl® (Ethicon) undyed suture material. After taking impressions, the temporary bridges were made by the technician on site and fitted. The vertical height and occlusion were checked and adjusted. This part of the job took approximately 6 hours. The patient was experiencing less soreness and bleeding from the soft tissue over the ridge as her erosive lichen planus appeared to be less symptomatic; although the condition affected all her mouth, it stayed unchanged on her buccal mucosa and pharyngeal areas. There was obvious improvement over the ridges and floor of the mouth (Figures 12-18 and Figure 20).



The final bridges were made and fitted 6 months later, and the patient has fully recovered from her previous experience and managed to eat and chew effectively (after 8 years) with minimal flare-ups from her inflamed oral soft tissues. The bleeding index from the soft tissues around the fixtures was minimal, and the halitosis issue was also resolved (Figures 21-27).



Conclusion
The All-on-4 concept for total rehabilitation is clinically effective but challenging. The survival rates of the implants and restorations is high according to the short-, medium-, and long-term studies.
The All-on-4 can be offered routinely to most patients in need of a complete edentulous rehabilitation. The use of NobelGuide (Nobel Biocare®) for computer planning can simplify the treatment if the patient is totally edentulous.
[/userloggedin]
[userloggedout][/userloggedout]
- Malo P, de Araújo Nobre M, Lopes A, Moss SM, Molina GJ. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142 (3):310-320.
- Maló P, de Araújo Nobre M, Lopes A, Francischone C, Rigolizzo M. “All-on-4” immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long term (5 years) outcomes. Clin Implant Dent Relat Res. 2012;14Suppl.:e139-150.
- Malo P, Lopes I, De Araújo Nobre. The All-on-4 concept. In: Babbush CA, Hahn JA, Krauser JT. Dental Implants: The Art and Science. Maryland Heights, Missouri: Saunders Elsevier;2011:435-447.
- Malo P, Lopes I, Costa R. Oral fixed rehabilitation of atrophic jaws. In: Francischone CE. Osseointegration and multidisciplinary treatment. Sao Paulo, Brazil: Quintessence Editora Itda;2008:Chapter 13.
- Malo P, Rangert B, Nobre M. All-on-4 Immediate function concept with Brånemark system implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(5 Suppl 1):2-9.
- Malo P, Rangert B, Nobre M. All-on-4 immediate-function concept with Brånemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;(7 Suppl 1):S88-S94.
- Rangert B, Aparicio C, Malevez C, Bedrossian E, Renouard F, Malo P, Calandriello R. Graftless rehabilitation of the atrophied maxilla – tilted implants, short implants and immediate function. In: Jensen OT. The Sinus Bone Graft. Denver, Colorado: Editorial Quintessence, SL; 2005:296-320.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Reza Faridrad, Dip Dent (lst), MSc (OMFS), MFDS RCS (Eng), qualified in 1995 and has 3 years of postgraduate education in oral and maxillofacial surgery at Eastman Dental Institute. He was awarded a prestigious master’s degree from UCL in 2001. He has 4 years’ hospital experience in oral and maxillofacial surgery and orthodontics in London (UCH), Liverpool (Aintree Hospitals), Gloucester, and Cheltenham general hospitals. Dr. Faridrad has allocated his time to dental implant treatments, mentoring, visiting surgeons, and accepts referrals for complex cases as well as dealing with failed dental implant treatments. Contact Dr. Faridrad by emailing
Reza Faridrad, Dip Dent (lst), MSc (OMFS), MFDS RCS (Eng), qualified in 1995 and has 3 years of postgraduate education in oral and maxillofacial surgery at Eastman Dental Institute. He was awarded a prestigious master’s degree from UCL in 2001. He has 4 years’ hospital experience in oral and maxillofacial surgery and orthodontics in London (UCH), Liverpool (Aintree Hospitals), Gloucester, and Cheltenham general hospitals. Dr. Faridrad has allocated his time to dental implant treatments, mentoring, visiting surgeons, and accepts referrals for complex cases as well as dealing with failed dental implant treatments. Contact Dr. Faridrad by emailing 
