Dr. Charles D. Schlesinger discusses certain technologies to facilitate faster, more predictable treatment
Introduction
Implant treatment that results in the patient walking out within an hour with temporary teeth is a huge practice builder. Patients today are looking for immediate gratification and have read or heard about teeth in a day. In order to safely and predictably perform this type of service for your patients, you must have the correct armamentarium to facilitate rapid, safe, and accurate treatment.
[userloggedin]
 Case report
Case report
A 57-year-old female missing teeth Nos. 18 and 19 with a history of osteoporosis presented to the office. Currently, she was not taking any medications, yet had been on Fosamax for 1 week before discontinuing it due to GI distress. All other medical history was without issue.
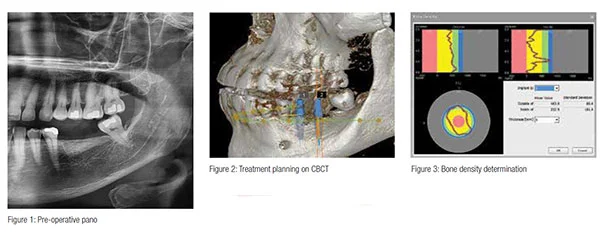
Upon her intraoral exam, it was noted that tooth No. 14 had supra-erupted approximately 1 mm due to the missing opposing dentition. Enameloplasty would be carried out at the time of implant placement to create enough intra-arch space for the abutment and final restoration. A CBCT and panoramic radiograph (Vatech America) were taken (Figure 1) and the sites evaluated for treatment (Figure 2). Using the bone density function (Hounsfield units) in the native Vatech software (Figure 3), it was determined that the patient’s previous diagnosis of osteoporosis could be a factor. The use of CBCT density information is a great predictor of implant site bone density.1
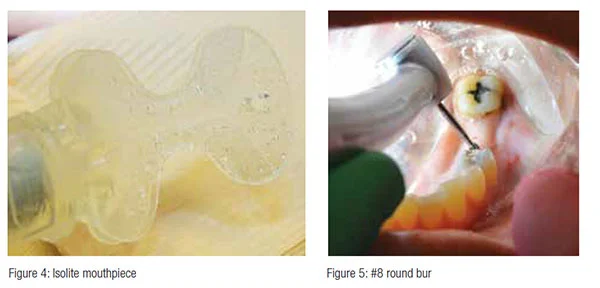
After infiltrate anesthesia with 4% Septocaine® (Septodont) of the soft tissue in the area of tooth Nos. 18 and 19, an Isolite® (Isolite® Systems) was placed into the patient’s mouth. The use of this device provides not only many benefits during restorative dentistry, but also huge advantages during implant surgery especially with the introduction of a sterile mouthpiece.
Since we work with very small instruments such as drivers and very small components, an Isolite (Figure 4) with its ability to protect the trachea and esophagus — along with providing dual suction, a mouth prop, and very bright LED illumination — helps alleviate many of the dangers and potential issues we run into in implantology. The isolation and illumination make implant surgery much faster, as the tongue and fluids are no longer issues.
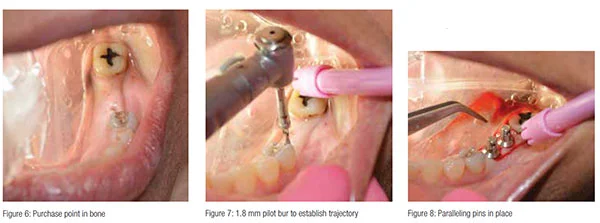
Initial positioning of the osteotomy was carried out using a No. 8 round bur on a high-speed handpiece (Figure 5). Since I was planning to place two 5.0 mm diameter implants, the anterior implant center was positioned approximately 4.5 mm distal to the premolar (Figure 6).
Once the soft tissue was penetrated and purchase point established on the crest, a 1.8 mm pilot bur was taken to a depth of 8 mm into soft tissue (Figure 7). A paralleling pin was placed, and the second access and pilot hole were drilled parallel to the first. A paralleling pin was placed to evaluate implant position and intra-implant distance (Figure 8).
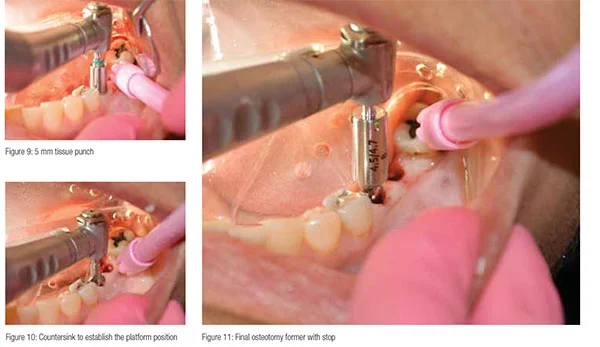
A guided 5 mm diameter tissue punch (Figure 9) was used to remove a specified amount of keratinized tissue to allow access to the crestal bone. A punch technique was chosen in this case due to the sufficient quantity of keratinized tissue available to maintain a zone of keratinized tissue around the implant collar. If the patient had presented with insufficient tissue with the presence of unattached mucosa on the ridge, a full thickness periodontal flap would behave been elevated in order to reposition keratinized tissue to the buccal. Once this access is completed, a countersink (Figure 10) was utilized to not only allow the imbedded tapered platform of the implant to seat passively, but also to assure the proper position of the restorative platform.
The 1.8 mm pilot drill was used again to final depth, and then a 4.7 mm osteotomy former was used with an 8 mm depth stop (Figure 11) to create the final osteotomies for the implants. The unique step drill design of these osteotomy formers allows a two-step drilling protocol instead of the customary serial progression as is the case with other systems. The osteotomies were checked with a small curette to assure 360° bone support. TSI implants size 5.0 mm x 8 mm (OCO Biomedical) were chosen for the case. In posterior cases, my go-to implant is the TSI (Figure 12). The dual stabilization that can be achieved will increase the chances of being able to load the implant immediately or early. The OCO implant is designed for immediate loading using Dual Stabilization™, an industry-unique design feature that biomechanically secures the tip and collar of the implant.2 While other implant companies boast their revolutionary surface treatments, OCO implants immediately “lock” into the bone at placement. The tissue-level design lends itself to an easy and predictable restorative procedure and excellent crestal bone preservation.

 The implants were inserted and torqued into place. Neither implant attained a torque value greater than 35 N/cm upon seating. Literature shows great success and predictability in immediate loading with values greater than 40 N/cm. ISQ readings were taken with an Osstell IDX (Osstell, Gothenberg, Sweden; Columbia, Maryland). A smart peg was placed and reading taken (Figure 13). Implant No. 19 registered 70 in both the BL and MD directions and No. 18 had measurements of 75 BL and 80 MD (Figure 14).
The implants were inserted and torqued into place. Neither implant attained a torque value greater than 35 N/cm upon seating. Literature shows great success and predictability in immediate loading with values greater than 40 N/cm. ISQ readings were taken with an Osstell IDX (Osstell, Gothenberg, Sweden; Columbia, Maryland). A smart peg was placed and reading taken (Figure 13). Implant No. 19 registered 70 in both the BL and MD directions and No. 18 had measurements of 75 BL and 80 MD (Figure 14).
 According to the literature, an ISQ of greater than 70 is an indication to immediately temporize.3 Though the seating torque was well below the minimum usually associated with enough primary stability to load early or immediately, it has been shown that ISQ is a predictable indicator of when to load or not.4 Since the Osstell quantifies the micromovement in a side-to-side manner, it is a more predictable manner to assess implant stability than torque alone.5
According to the literature, an ISQ of greater than 70 is an indication to immediately temporize.3 Though the seating torque was well below the minimum usually associated with enough primary stability to load early or immediately, it has been shown that ISQ is a predictable indicator of when to load or not.4 Since the Osstell quantifies the micromovement in a side-to-side manner, it is a more predictable manner to assess implant stability than torque alone.5
Since the ISQ value was as high as it was for both implants, the choice to immediately temporize was taken. Solid crown and bridge abutments of 4 mm tall were torqued into place at 30 N/cm (Figures 15 and 16) and then re-torqued after 5 minutes to accommodate for any pre-stretch of the abutment screw threads. The opposing occlusal surfaces were then reduced with a minimal amount of enameloplasty to create the proper clearance necessary for the intended restorative material.
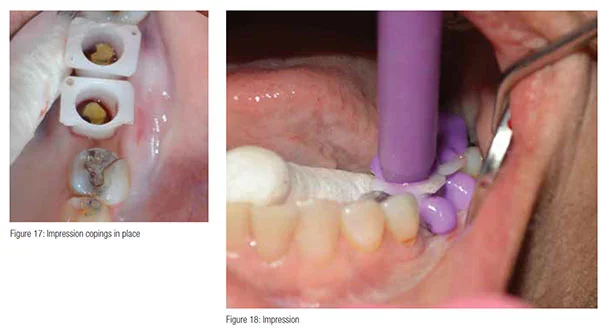
A shade was taken, and impression copings were placed onto the implants and abutments (Figure 17). The final full arch impression was taken with VPS impression material. Light body was injected into the impression copings (Figure 18), and heavy body was extruded into the impression tray. An opposing impression was taken in alginate, and a blue-bite registration was also taken at this time.
 Acrylic temporaries were fabricated over acrylic copings. The copings assure a perfect margin and will prevent any soft tissue from migrating under the temporary and potentially causing an issue at the seat appointment. The temporaries were cemented with Improv® cement (Alvelogro). The restorative margins of the implants were only 1.0 mm-1.5 mm below the intended free gingival margins making cement cleanup an easy task and assured that it is complete not only at the temporary stage, but once the final crowns are delivered. The excess cement was removed and the final occlusion rechecked, and then the patient was dismissed. She will return in 1 month for delivery of her final restorations and completion of the case.
Acrylic temporaries were fabricated over acrylic copings. The copings assure a perfect margin and will prevent any soft tissue from migrating under the temporary and potentially causing an issue at the seat appointment. The temporaries were cemented with Improv® cement (Alvelogro). The restorative margins of the implants were only 1.0 mm-1.5 mm below the intended free gingival margins making cement cleanup an easy task and assured that it is complete not only at the temporary stage, but once the final crowns are delivered. The excess cement was removed and the final occlusion rechecked, and then the patient was dismissed. She will return in 1 month for delivery of her final restorations and completion of the case.
Conclusion
This patient was able to get two implants placed and walk out with temporaries in approximately an hour. She will return to the office in approximately 2-4 weeks for the delivery of the final full contour zirconia restorations. Dentistry today is highly competitive, and the patients are highly demanding when it comes to dental treatment. Using technology such as Isolite and Osstell will make implantology safer, faster, and more predictable. The goal of any treatment is to provide dental treatment at the highest level and with the highest patient satisfaction.
[/userloggedin]
[userloggedout][/userloggedout]
- Salimov F, Tatli U, Kürkçü M, Akoğlan M, Oztunç H, Kurtoğlu C. Evaluation of relationship between preoperative bone density values derived from cone beam computed tomography and implant stability parameters: a clinical study. Clin Oral Implants Res. 2014;25(9):1016-1021.
- Saini D. Dental Implants: Dual stabilization technology. IJBAR. 2015;6(02):196-198.
- Kokovic V1, Jung R, Feloutzis A, Todorovic VS, Jurisic M, Hämmerle CH. Immediate vs. early loading of SLA implants in the posterior mandible: 5-year results of randomized controlled clinical trial. Clin Oral Implants Res. 2014;25(2):e114-119.
- Schlesinger C. Torque versus RFA in implant placement. Implant Practice US. 2016;9(4):14-20.
- Schlesinger CD. Immediately Loading Dental Implants: Doing it Right for Long-Term Success. Dent Today. 2016;35(5):84, 86-89.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Charles Schlesinger, DDS, FICOI, is the founder and CEO of The C.D. Schlesinger Group, a dental implant consulting company. For the past 10 years, he has been an internationally renowned implant educator, teaching implantology based upon his years in private practice and his work as an
Charles Schlesinger, DDS, FICOI, is the founder and CEO of The C.D. Schlesinger Group, a dental implant consulting company. For the past 10 years, he has been an internationally renowned implant educator, teaching implantology based upon his years in private practice and his work as an

