Editor’s intro: Dr. Tarun Agarwal addresses the challenges and solutions for fixed implant hybrid cases.
Dr. Tarun Agarwal discusses the learning curve and subsequent revelations gained regarding the implant process
As a general dentist practice owner, I am constantly looking for new options to add to my practice to help patients and increase revenue. About 10 years ago, I made a firm decision to add dental implants — it’s a decision I haven’t looked back from. As that journey progressed, I felt it time to tackle my first full-arch implant case (about 3 to 4 years into my implant journey). Truthfully, I was not sure what I was doing, so I enlisted the help of an oral surgeon and sent the patient for a consult. The rest, as they say, is history.
That first case was a total disaster on so many levels. Looking back, it was the best thing that could have happened to me!
Patient confusion
I sent the patient to the surgeon without discussing fees and the process. About 6 months later, the patient returned to me with five implants in her maxillary jaw and asked when she would get her teeth. I proceeded to make up a restorative fee, and the patient said “I already paid the surgeon.” I called the surgeon, and he advised me that she had paid for the surgery. So to keep the patient happy, I was in a dilemma. I thought, What do I do now? Just wanting to get a few cases under my belt, I agreed to restore the case for the lab cost — to which the patient reluctantly agreed. And I was off to the races.
Restorative nightmare
Being a novice at implants, I quickly realized this situation was nothing like taking a one- or two-unit dental implant impression. There were preliminary impressions, verification impressions, trial bites, trial screwed-in setups, material considerations, prosthetic space considerations, and hygiene-design considerations. As a result, I spent four appointments just getting a final working impression, only to discover that due to implant positioning, we needed to place multi-unit abutments (MUA) to correct angulations. Now, every time I am doing a try-in, I am fiddling with these MUAs and making sure they are on correctly. Finally, we got done, and the result wasn’t exactly hygienic (due to lack of bone reduction) nor esthetic. Luckily, “the patient was happy.” Probably, she was just tired of the long and drawn-out process.
Team bias
What I wasn’t aware of during all of this was how the team was watching and making notes. They basically had decided to never allow us to do a case like this again. It sent a “mentality message” that is critically important to successful integration of any new procedure. This has the biggest effect on success in your practice.
At the conclusion of treatment, I must have seen this patient for 15 visits and felt stressed and stupid at each visit. Even if I was paid my full fee, it would have been a loss. To make matters worse, I didn’t estimate the lab bill properly — I didn’t know to plan for MUA costs, impression component costs, and other miscellaneous items.
I was tempted to give up before I even really got started. But I felt there had to a better way. Frankly, I was too stubborn to give up.
So I went to my classic playbook — how could I leverage technology to make this better. What I found has turned out to be amazing and practice-changing. Over the years, workflow has morphed and improved — from both simply my having done more cases and improvements in digital technologies. In this case presentation, I would like to offer an overview the process from beginning to end.
Partners for patient outcome
I follow a pretty simple philosophy of teamwork for ideal patient outcomes. This allows me to leverage various areas of expertise to achieve maximum efficiency and minimize stress. The three team members follow.
1. Restorative dentist
The restorative dentist is the “conductor of the orchestra.” After all, patients don’t really come for dental implants; they come for a smile. So the restorative outcome has to be kept in mind prior to committing to surgery.
2. Surgical dentist
The surgical dentist is the person performing the surgery and coordinating the optimal level of sedation for patient comfort. This person will ensure efficient surgery following the plan and any postoperative follow-ups.
3. Dental laboratory
The dental laboratory is a key component to make this actually happen. The lab is tasked with designing the diagnostics, designing the guide, and fabricating the actual restorations.
Technology has certainly reached a point where the general dentist can be all or a few of these components. The depth at which the general dentist is involved is dependent on comfort, surgical skill, and the patient’s medical condition.
Diagnosis and case acceptance
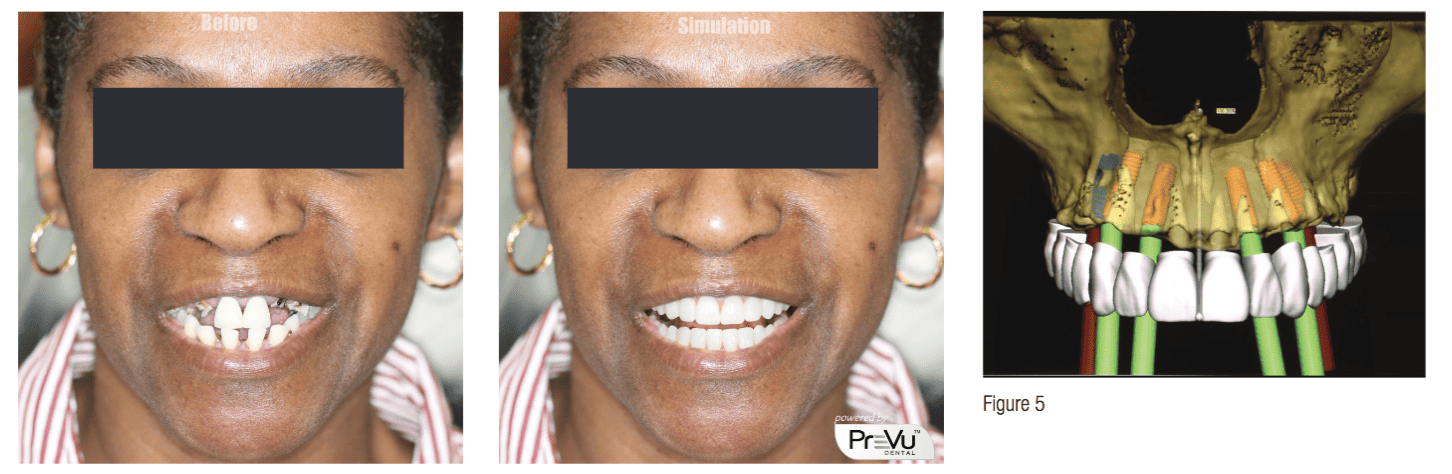
Today, diagnosis starts during the consultation. Our treatment coordinator sits with the patients to discover their needs, take a preset series of digital photographs, and a 3D CBCT. She then sends the full-face photo to our laboratory partner for smile simulation and reviews demonstration models with the patient. At this point, I meet the patient, assess his/her condition, answer any questions, and begin the diagnostic virtual planning. By the end of our consultation visit, the patient has a clear answer of what options exist and what his/her new smile will look like (after the simulation is completed and shown to patient), and I will have a clear idea of the involvement of his/her surgery. Our treatment coordinator then sits with the patient to review the game plan and begins the discussion of how to make this affordable for the patient.
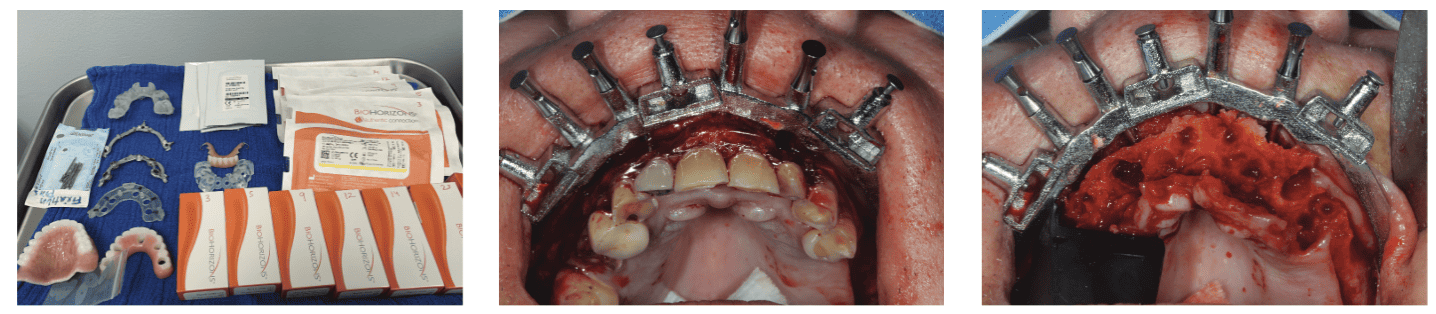
Once the patient accepts treatment and firm financial arrangements are in place, the diagnostic records are transferred to our skilled laboratory for final planning and guide fabrication. I provide the laboratory an initial implant plan and approve the final plan through remote session. The laboratory also provides me with a comprehensive list of all implant components that are necessary for this case and sends the final guides to the office.

Surgery and immediate teeth
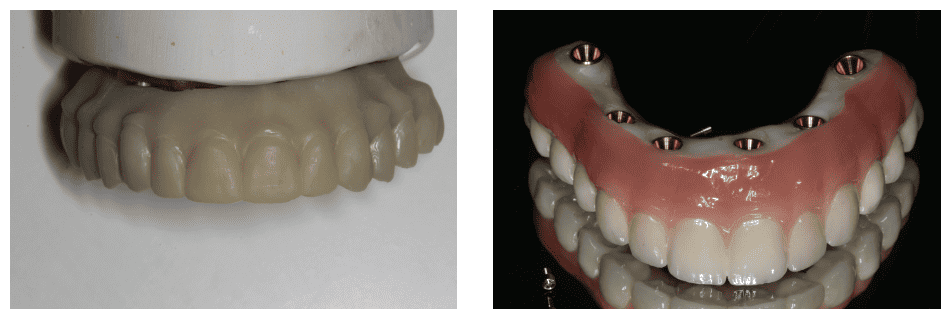
At this point, I have walked through surgery virtually and am very familiar with the potential pitfalls. All materials are set aside in order to maximize efficiency, and the patient is sedated (we choose to use a surgical center with MD anesthesiologist providing nasal intubation). The guide is fitted over the teeth and tacked into place. Guided bone reduction is completed to create proper prosthetic space and develop ideal hygienic contours. The implant guide is placed, and the dental implants are guided into place ensuring adequate primary stability. A conversion-milled prosthetic has been prefabricated and fits on top of the foundation guide to allow for immediate loading of the implants with a strong and hygienic provisional prosthetic. The bite is verified, and an immediate postoperative panoramic X-ray is taken.
Honestly, this part has become straightforward, and the average case takes about 90 minutes per arch. I have full confidence the implants are being placed in the proper position to best support the final prosthetic. The patient is scheduled for a 1-week follow-up and 3-month follow-up.
Final restorative
After allowing for integration, I begin fabricating the final restorative. As a restorative dentist, this is where my life has been made easier — due to better planning, guided surgery, immediate conversion, and leveraging digital technologies.



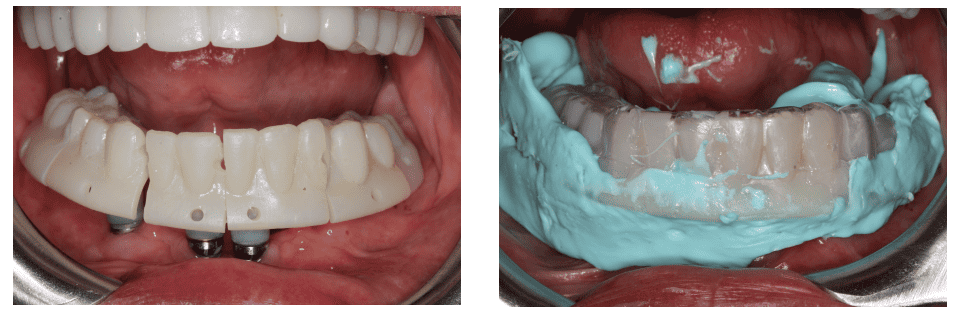
The first step is a preliminary implant level impression by actually scanning the conversion prosthetic with analogs in place and also digitally capturing the bite and opposing dentition.
The lab then makes necessary esthetic design changes and bite modifications and prints a prosthetic implant verification jig tray (iJIG), which is screwed into the mouth in pieces. A panoramic X-ray is taken to verify complete seating of each component and luted together using bis-acryl. A tissue impression is then taken with light body PVS injected under the iJIG. In a single visit, we have completed the verified impression, bite records, esthetic verification, and tissue impression. The next step is a final trial smile to verify fit, function, esthetics, and phonetics. Once verified, the lab is instructed to fabricate the final restoration.
Thanks to leveraging digital technologies and putting the right partners in place, what was once complicated and unpredictable has become enjoyable, profitable, and predictable. If you have felt the same frustrations and have given up on these types of cases, or feel that you and your surgical specialist aren’t on the same page, know that modern solutions exist to age-old problems.
Dr. Agarwal is a dynamic speaker and implant educator. After reading his article on his fixed implant hybrid procedure, read more about his journey to implants in “On cultivating, motivating, and inspiring his patients and team” here.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Tarun Agarwal, DDS, graduated dental school from University of Missouri at Kansas City in 1999. In 2001, he founded Raleigh Dental Arts with the goal of building the preeminent dental practice in the Raleigh area. He recently built a training center within the practice dedicated to sharing his expertise. He is a recognized speaker, author, and dental leader and has been featured on CBS, NBC, ABC, FOX, and News 14 Carolina.
Tarun Agarwal, DDS, graduated dental school from University of Missouri at Kansas City in 1999. In 2001, he founded Raleigh Dental Arts with the goal of building the preeminent dental practice in the Raleigh area. He recently built a training center within the practice dedicated to sharing his expertise. He is a recognized speaker, author, and dental leader and has been featured on CBS, NBC, ABC, FOX, and News 14 Carolina.

