Editor’s Intro: Dr. Dean Vafiadis outlines his full-arch restoration process using 3Shape TRIOS IOS.
Dr. Dean Vafiadis outlines his steps for full arch restoration
Introduction
Full arch restoration for patients can be treatment planned and fabricated in many different ways. Utilizing IOS 3ShapeTRIOS® scanning technology has made these treatments much easier and more accurate for mounting, fabrication, and delivery of the restoration.1,2 Using new software, file sharing, and file merging will allow the clinician and laboratory to get ideal positions of teeth, implant abutments, final restorations, and occlusal morphology to the ideal positions that are best for each patient.
This is a case report of a patient who presented with periodontal disease on the maxillary and mandibular arch. Many teeth had Class II and Class III mobility. Pocket depth ranged from 5 mm to 10 mm on many teeth. The patient had a traumatic experience with her previous dental office and had not visited a dentist in more than 7 years. Most of the lower teeth were hopeless and could not be saved. Based on patient’s needs of function, esthetics, and traveling schedule, three options were presented at her consultation visit (Figures 1-3).
Option 1
- Extract all teeth, immediate placement of 5-6 implants on the mandible and maxilla.
- Immediate provisional in occlusion.
- Final restoration would be a zirconia fixed-hybrid prosthesis.
Option 2
- Sequentially extract teeth while keeping the provisional restoration to hold the occlusal vertical dimension (OVD).
- Maintain teeth with perio-prostho concept and maintain tissue levels for better natural gum tissue.
- Keep teeth that were stable to hold the provisional.
- Final restoration would be splinted zirconia-ceramic crowns and bridges.
Option 3
- Extract all teeth and place immediate complete dentures to reduce finances.
- Final restoration would be complete upper and lower dentures.
Treatment
The patient chose option 2, and treatment proceeded as follows.





Methods and materials
Digital diagnostic scans were made. A CBCT scan was taken, and a diagnostic wax-up was fabricated for ideal provisional to new OVD position. Strategic extraction of teeth Nos. 17, 20, 21, 23, 24, 25, 26, 28, 29, and 31 was performed. After extractions were performed, a provisional restoration was placed at a new occlusal vertical dimension based on the jaw position that was analyzed with the CT scan (Figure 4).

This allowed the clinician to restore OVD and give the patient ideal mandibular movement. This would also reduce the occlusal forces to the provisional and natural teeth during the healing phases.3

The provisional restoration was made from teeth Nos. 19 to 30. Teeth remaining were 19, 22, 27, and 30. The teeth were retaining the provisional and were root-planed and scaled to have ideal periodontal healing during the splinted provisional therapy. This will also allow for cross-arch stability of the provisional and restore the new OVD position with canine guidance occlusion. Internal connection implants (Ritter™ Implants, San Antonio, Texas) were placed in sites 20, 21, 23, 25, 26, 28, and 29.

While the implants were healing, the provisional restoration maintained the newly restored vertical dimension and sealed the dental tubules of the existing remaining mandibular teeth with dentin- bonded solution (ExciTE®, Ivoclar Vivadent®, Amherst, New York). After 5 months of healing, the implants were uncovered, and healing caps were replaced for 3 weeks. Tooth No. 19 was loose and was extracted. An additional implant No. 30 was placed and allowed to heal for 4 months. The provisional was removed after all implants were osseo-integrated, digital scan bodies were placed (Core3dcentres®, Las Vegas, Nevada) for the posterior implants, and standard impression copings were placed on the anterior implants. Radiographs were taken to ensure correct position on the implant fixtures.
A 3Shape TRIOS scanner was used to scan the full arch of the mandible in addition to maxillary provisional (Figures 5 to 10).
Three individual occlusion scans were merged together in one consistent file. The first scan was with posterior right provisional used as stops in place so that ideal OVD was scanned. A second scan was with the posterior left provisional in place. The third scan was for the anterior teeth in ideal OVD position. These scans were merged instantaneously with the software to produce ideal OVD position of maxillary and mandibular arches (Figures 11 and 12).
Files were imported into 3Shape implant software, and abutment design was initiated. Implants on the posterior left and right, as well as anterior implant abutments, were designed for ideal position and distribution mesially and digitally (Figure 13).
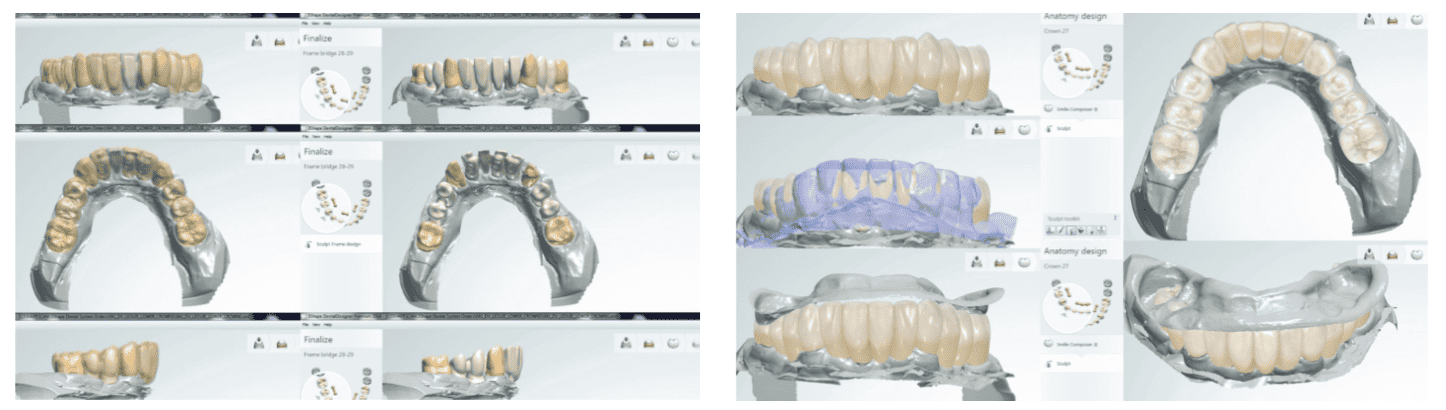
A separate scan of the provisional can be seen in purple color, merged and overlaid to anatomical position mesially and distally, so that the clinician can approve or edit designs as needed (Figure 14).
This also allows the clinician to evaluate individual alignment and interproximal position, which ultimately allows the patient access to clean the pontic sites. This is a critical step in the quality control of full arch implant cases. This step can save many “try-in” visits because of the accuracy and visualization of final designs. This also gives excellent communication between the lab technician and the clinician. In addition, more detailed analysis of the CAD/CAM abutments was made circumferentially around each abutment-tissue emergence profile. The emergence profile formula published by Goldstein, Vafiadis, and Kim, regarding the tissue-abutment-bone displacement was used to idealize the gingival levels of the abutments around the tissue of the implant.4 The XYZ axis is used to determine the ideal emergence design to avoid displacement and blanching of the tissues. Further input of a zirconia frame as designed by the technician and approved by the clinician shows proper position restorations and pontic sites. The esthetic outcome, porcelain overlay, and ideal OVD can be evaluated by the technician and the clinician. This will also minimize patient visits since the clinician can make the changes before final fabrication (Figures 15 and 16).
Delivery of final abutments and coping try-in was performed on the second restorative visit. A PVS pickup impression was made of all the zirconia copings.
A new vertical dimension record was made as well as a new face-bow transfer record to allow for ideal articulation virtually (Figure 17).
At the third restorative visit, the final design of all ideal anatomic forms of lower teeth and implants becomes a very easy and quick try-in bisque-bake visit with minimal occlusion adjustments. At the fourth restorative visit, patient acceptance for shade and shape of teeth, final stain, and glaze is performed and temporary cement is placed (Figures 18 and 19).
Temrex is used to cement all implant and teeth restorations. Final OVD is confirmed, and ideal occlusal guidance and emergence profile is evaluated. A 4-week postoperative evaluation is performed, and final cementation of all restorations is completed using Temrex (Temrex Corp., Freeport, New York) on implants and Durelon™ (3M ESPE) on teeth.



Discussion
The accuracy of the 3Shape TRIOS scanner can be realized fully when full arch restorations are being fabricated. The accuracy of the printing technology has also been improved to 16 microns (Stratasys Objet Eden206VS).5,6 3Shape software allows for ideal porcelain library to be imported and merged in matter of seconds. This allows for ideal position of anatomy emergence profile, occlusal contour, and esthetic position. The provisional overlay “purple” view was a significant advantage to show the clinician and technician the proper alignment of abutment position, posteriorly and anteriorly. The accuracy of these procedures for implant restorations can be seen by using the 3Shape TRIOS scanner. The verification of impressions and records are very consistent when using scanning technology and virtual articulation. The provisional cement was used on the implant restorations, and after 36 months in service, there has been no complication except for increased tartar in the posterior lingual areas of the anterior teeth. The patient is currently on a 3-month maintenance protocol for hygiene. There have been no failures or prosthetic complications or screw loosening up to this point.
Note: When these implants were scanned, we were using an older type of scan bodies. The current scan bodies that are being recommended today are the 3Shape scan bodies and Biodenta scan bodies for all implant systems.
Another article by Dr. Vafiadis that includes full-arch restoration also discusses digital dentistry for better diagnostic techniques and implementation. Read it here.
- Nedelcu,R Persson AS. Scanning accuracy and precision in 4 intra-oral scanners: an in vitro comparison based on 3-dimensional analysis. J Prosthet Dent. 2014;112(6):1461-1471.
- Fukazawa S. Odaira C, Kondo H. Investigation of accuracy and reproducibility of abutment position by intraoral scanners. J Prosthodont Res. 2017;61(4):450-459.
- Bachhav VC. Aras MA. Altering occlusal vertical dimension in functional and esthetic rehabilitation of severely worn dentition. J Oral Health Res. 2010;1(1):2-7.
- Goldstein G. Vafiadis D. Kim J. Finding Z: a mathematical method for predicting tissue position after implant abutment restoration placement. J Prosthet Dent. 2014;112(2):322-324.
- Sami T. Goldstein G. Vafiadis D. Malvin J. The accuracy of four intraoral scanners. Third place ACP award. Poster presented at: Digital Poster Session at the 48th Annual Session of the American College of Prosthodontists. October 31 – November 3, 2018; Baltimore, Maryland.
- Patzelt SB, Emmanouilidi A, Stampf S, Strub JR, Att W. Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig. 2014;18(6):1687-1694.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Dean C. Vafiadis, DDS, is a program director of the Full Mouth Rehabilitation CE course at NYU College of Dentistry (NYUCD). He has been on faculty at NYUCD since 1993. He currently practices in New York City, New York, where he is the president of the New York Smile Institute — a multi-specialty practice for esthetics, CAD/CAM, and implant dentistry. He currently uses CEREC®, TRIOS®, E4D, and 3M™ True Definition Scanners in his office. He has lectured around the world and has given over 300 all-day courses on esthetics, implants, and CAD/CAM technologies.
Dean C. Vafiadis, DDS, is a program director of the Full Mouth Rehabilitation CE course at NYU College of Dentistry (NYUCD). He has been on faculty at NYUCD since 1993. He currently practices in New York City, New York, where he is the president of the New York Smile Institute — a multi-specialty practice for esthetics, CAD/CAM, and implant dentistry. He currently uses CEREC®, TRIOS®, E4D, and 3M™ True Definition Scanners in his office. He has lectured around the world and has given over 300 all-day courses on esthetics, implants, and CAD/CAM technologies.

