Drs. Ann Marie Hofbauer and Salah Huwais offer another case study using a novel biomechanical site preparation technique
In 1981, Dr. Albrektsson, a member of Dr. Brånemark’s team, stated that there are six factors for reliable osseointegration: implant material and design, its surface condition, bone status, surgical technique, and implant loading condition. (Albrektsson, et al., 1981). In 2004, 23 years later, he re-emphasized the need for site preparation improvement, saying, “It seems probable that improvements in surgical technique will present good prospects for improving clinical results” (Albrektsson, et. al., 2004).
[userloggedin]
Bone is a unique composite of protein molecules and mineral structure that form together contradictory properties: stiffness yet flexibility, lightness yet strength (Seemen, et al., 2008). As it is inhomogeneous (not uniformed), anisotropic (directionally independent), and viscoelastic, bone is flexible enough to absorb energy and change shape (deform) without failing, yet it is able to widen in compression and able to lengthen with tension. If load exceeds the bone’s ability to deform elastically, it can deform further and change permanently by plastic deformation (Matrin, et al., 2008).
Bone behavior “strength” is directly related not only to its bulk of mineral density but also to its collagen integrity (Lang, et al., 2002). So, maintaining that bulk will determine the implant’s stability and its long-term success.
Osseodensification is a novel bio-mechanical site preparation technique. It produces low plastic deformation due to its non-extraction site preparation method, which preserves the bone to enhance
the host.
It utilizes a multi-fluted Densifying Bur technology (Versah™, LLC) that creates and expands a pilot hole without excavating significant amounts of bone tissue through a unique, highly controllable, fast, and efficient procedure with minimal heat elevation. The taper design allows the surgeon to modulate pressure and irrigation, while providing a unique real-time haptic feedback that makes the Densifying Bur intuitive for every skilled implant surgeon.
When the densifying bur is rotated at 800-1500 RPM in the counterclockwise non-cutting direction (Densifying mode), downward surgical pressure coupled with steady external irrigation creates a gentle compression wave inside the osteotomy that works with the fluting to generate a densified layer through compaction and autografting the surrounding bone while plastically expanding the bony ridge at the same time (Meyer, Huwais, et al., 2014). The Densifying Burs can also be rotated in the clockwise cutting direction (Cutting Mode) to cleanly cut bone if needed. This dual use capability allows for clinical versatility — it may enable the implant surgeon to autograft the maxillary sinus and efficiently expands any ridge in either jaw with enhanced implant stability.
Our previous case report involved a ridge expansion and two implant placements in the mandible. This case report is about expanding an inadequate 3-mm ridge in the maxilla to place a 4.2-mm implant with enhanced primary stability.
Case report: maxillary ridge expansion with implant placement
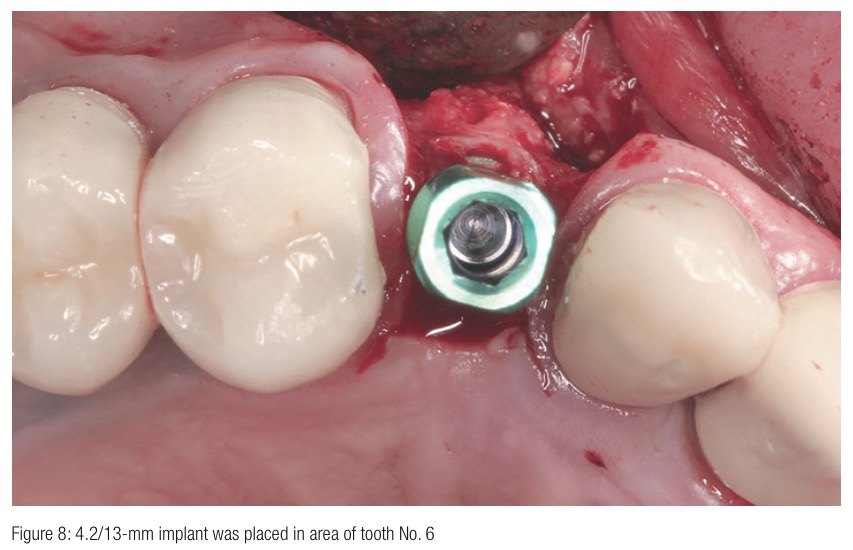
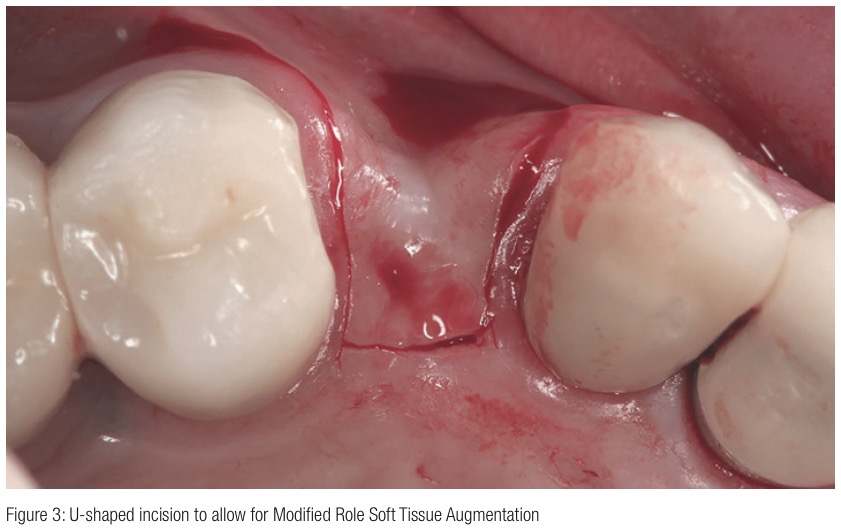
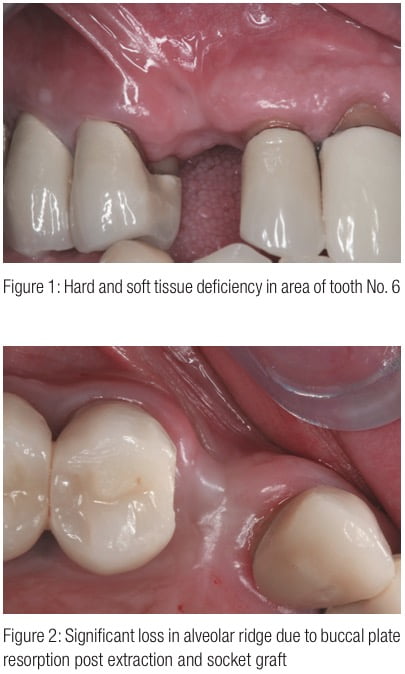 The patient is a 65-year-old male presenting with missing tooth No. 6. Radiographic and clinical examination revealed a significant hard and soft tissue deficiency due to alveolar ridge resorption (Figures 1 and 2). Patient medical history was non-contributory. Dental history included surgical extraction of tooth No. 6 with socket preservation graft. Treatment options with their potential risks and benefits were presented to the patient. A final treatment plan was decided to utilize one implant placement for single crown restoration. Consent was given by patient to utilize osseodensification site preparation for ridge expansion with immediate implant placement and ridge augmentation if needed.
The patient is a 65-year-old male presenting with missing tooth No. 6. Radiographic and clinical examination revealed a significant hard and soft tissue deficiency due to alveolar ridge resorption (Figures 1 and 2). Patient medical history was non-contributory. Dental history included surgical extraction of tooth No. 6 with socket preservation graft. Treatment options with their potential risks and benefits were presented to the patient. A final treatment plan was decided to utilize one implant placement for single crown restoration. Consent was given by patient to utilize osseodensification site preparation for ridge expansion with immediate implant placement and ridge augmentation if needed.
The upper right anterior area was anesthetized using infiltration with 1.8 ml 4% Septocaine® (Septodont) with 1:100,000 epinephrine. Interproximal papillae were conserved. U-shaped incisions with extended vertical releases were made (Figure 3) to allow for Modified Roll Soft Tissue Augmentation technique. A full thickness flap was reflected, and a 3.0-mm crestal alveolar ridge width was confirmed by direct measurement (Figure 4).
 A 1.7-mm initial pilot osteotomy was created to a depth of 13 mm utilizing a high-speed surgical handpiece and a surgical motor (W&H). The pilot drill was rotating at 1200 RPM in a clockwise (CW) rotation. Using the pilot drill as a paralleling pin, an X-ray was taken to confirm the angulation between the adjacent teeth and the implant.
A 1.7-mm initial pilot osteotomy was created to a depth of 13 mm utilizing a high-speed surgical handpiece and a surgical motor (W&H). The pilot drill was rotating at 1200 RPM in a clockwise (CW) rotation. Using the pilot drill as a paralleling pin, an X-ray was taken to confirm the angulation between the adjacent teeth and the implant.
Once the correct position of the implant was confirmed, osseodensification was utilized using Densah™ Bur VT1828 (Versah™, LLC) running in a non-cutting counterclockwise (CCW) direction at 1200 RPM (Densifying Mode) with a bouncing motion to expand the osteotomy to 2.8 mm (Figure 5).
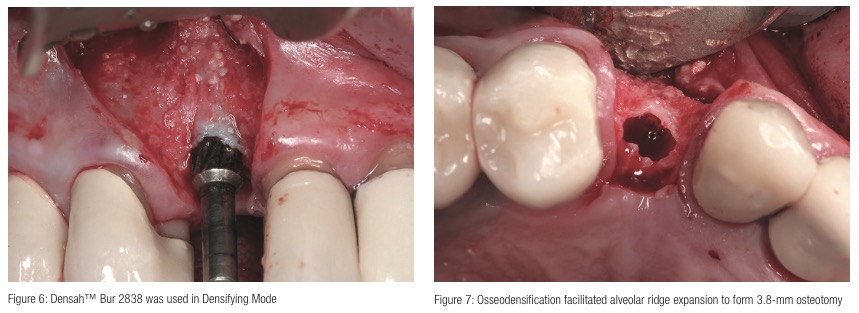
Sequential use of Densah™ Bur VT2838 running in a non-cutting counterclockwise (CCW) direction at 1200 RPM (Densifying Mode) with a bouncing motion was utilized to expand the osteotomy to a 3.8-mm diameter (Figure 6).
Osseodensification facilitated maxillary ridge expansion to form an osteotomy of 3.8-mm diameter without any buccal bone dehiscence (Figure 7), which allowed for total implant length placement in autogenous bone.
One 4.2/13 Legacy2™ (Implant Direct™) was placed with an insertion torque > 50 Ncm (Figure 8).

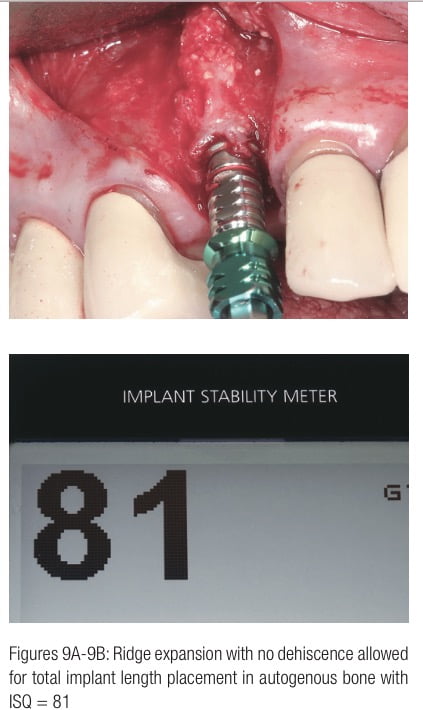 Implant stability was tested with an (Osstell®) ISQ implant stability meter. Buccal-lingual ISQ reading was 81. A healing abutment was placed, and the Modified Roll technique was used as soft tissue augmentation in the buccal of implant No. 6 site (Figure 11A).
Implant stability was tested with an (Osstell®) ISQ implant stability meter. Buccal-lingual ISQ reading was 81. A healing abutment was placed, and the Modified Roll technique was used as soft tissue augmentation in the buccal of implant No. 6 site (Figure 11A).
Buccal-lingual ISQ readings were obtained weekly for 6 weeks. At 3 weeks post placement, ISQ reading for implant No. 6 was 67. Although many studies have suggested that implants with ISQ 67-68 have the stability needed for loading, our team chose to wait for further soft tissue maturation.
At 6 weeks post placement, ISQ reading was increased substantially to 79/83. This increase in stability allowed us to start the restorative phase.
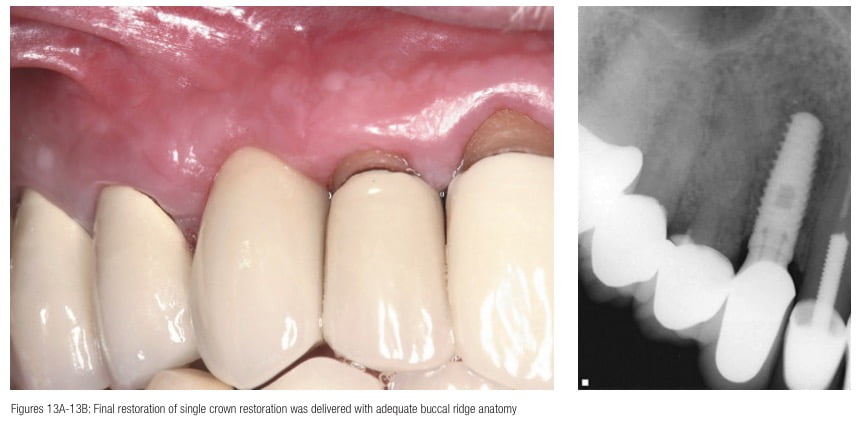
The patient was referred back to his restorative dentist for final restoration at 6 weeks. Final restoration of a single crown was delivered with adequate buccal ridge anatomy (Figure 13).
Supportive and follow-up care
The patient returned at 1 year for clinical and radiographic follow-up. Examination revealed healthy hard and soft tissue with no sign of inflammation or infection. The patient maintained buccal bone anatomy, and adequate coronal bone level was evident.
The 2-year radiograph taken by the patient’s restorative dentist demonstrated no change in alveolar bone height (Figure 16).
Discussion
In this case, osseodensification utilizing Densah™ Bur technology has facilitated ridge expansion in the maxilla with maintained alveolar ridge integrity, allowing for total implant length placement in autogenous bone with adequate primary stability. Despite compromised bone anatomy, osseodensification preserved bone bulk and promoted a shorter healing period. According to Trisi, et al., 2009, immediate implant loading can be recommended when insertion torque value (ITV) is at least 45Ncm, and ISQ is at least 68. Ossseo-densification technique can be recommended to enhance primary stability and possibly allow for earlier loading due to higher ITV and ISQ.
Conclusion
Osseodensification utilizing the Densah™ Bur technology produces stronger osteotomy for any implant. It preserves the bone to enhance the host. This allows for clinical versatility, which may facilitate enhanced implant stability and efficient expansion of any ridge in either jaw.
- Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155-170.
- Albrektsson T, Wennerberg A. Oral implant surfaces: Part 1— review focusing on topographic and chemical proper- ties of different surfaces and in vivo responses to them. Int J Prosthodont. 2004;17(5):536-43.
- Seeman E. Bone quality: the material and structural basis of bone strength. J Bone Miner Metab. 2008;26(1):1-8.
- Martin TJ, Seeman E. Bone remodelling: its local regula- tion and the emergence of bone fragility. Best Pract Res Clin Endocrinol Metab. 2008;22(5):701-722.
- Lang TF, Guglielmi G, van Kuijk C, De Serio A, Cammisa M, Genant HK. Measurement of bone mineral density at the spine and proximal femur by volumetric quantitative computed tomography and dual-energy X-ray absorp- tiometry in elderly women with and without vertebral fractures. Bone. 2002;30(1):247-250.
- Meyer E, Huwais S. Osseodensification is a novel implant preparation technique that increases implant primary stability by compaction and auto-grafting bone. American Academy of Periodontology. [abstract]. San Francisco, CA. 2014.
- Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G. Implant micromotion is related to peak inser- tion torque and bone density. Clin Oral Implants Res. 2009;20(5):467-471.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores