Drs. David W. Engen, Gregori M. Kurtzman, and Tarek El-Bialy discuss a novel approach to implant procedures that includes applying high-frequency vibration (HFV) with VPro to stimulate bone growth.
Drs. David W. Engen, Gregori M. Kurtzman, and Tarek El-Bialy illustrate five patient cases
Introduction
Part 1 of this series discussed considerations for ridge and socket preservation in preparation for implant placement. The treatments used for these patients involve a novel approach applying high-frequency vibration (HFV) to stimulate bone growth. Orthopedically and dentally, the literature demonstrates that when bone is stimulated with HFV during healing, osteoblastic activity increases, and denser more organized bone results. When applied to extraction sockets during the healing phase in anticipation of implant placement, higher quality and quantity of bone is present to accommodate the planned implant when compared to sites that were not treated with HFV. This HFV protocol is implemented by the patient at home using a 5 minute routine daily making compliance easy. Part 2 of this series reviews five patient cases using this innovative method.
Case report No. 1
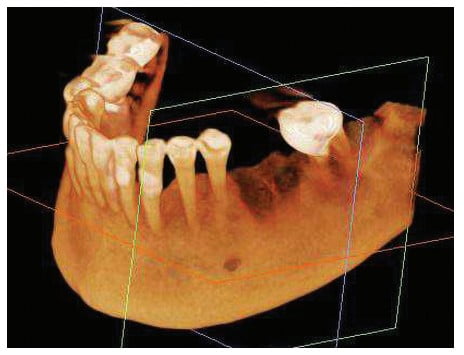
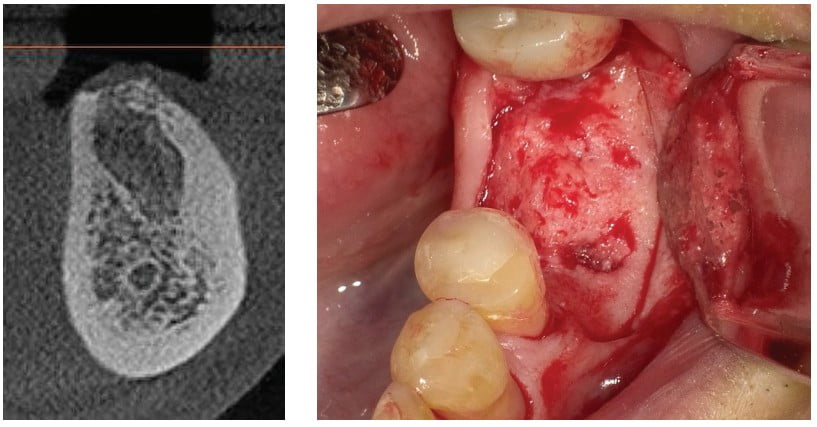
A 73-year-old male presented with an abscessed, nonrestorable lower-left first molar (tooth No. 19) with a vertical root fracture (VRF) on the mesial root (Figure 1). Surgical extraction was performed, and a post-extraction CBCT was acquired (Figure 2). The socket was intact. The patient returned 4 months postsurgically, and a pre-implant CBCT was acquired (Figures 3 and 4). The ridge had adequate buccal-lingual width to permit implant placement with sufficient buccal and lingual thickness of bone between the planned implant and the periosteum. Bone had filled in everywhere but the mesial-buccal socket, which was filled with granulation tissue (Figure 5). The granulation tissue was removed, a 6.0 mm x 11 mm implant was placed, and the void was grafted with mineralized bone putty and covered over with a collagen membrane. The implant was still able to be done single stage (Figure 6). The patient was instructed to use the VPro™ HFV oral device with a bite plane utilized daily for 5 minutes post-extraction during the 4-month healing period. Density was measured on the CBCT in Hounsfield units at an area in the extraction socket for the immediate extraction CBCT and again in the same spot on the post-healing CBCT, indicating an increase in density of the healed clot, which was present in the socket initially (Table 1). For standardization, an area on the socket wall was compared at initial CBCT, and post-CBCT was measured for standardization on the patient indicating similar density values to bone outside the socket before-and-after use of HFV (Table 2). The large osseous defect resulting from the VRF of the mesial root at the 4-month postoperative appointment bone-fill had occurred with a small residual area at the mesial root that permitted the planned implant placement.



** Values rounded to 1.0

Case report No. 2
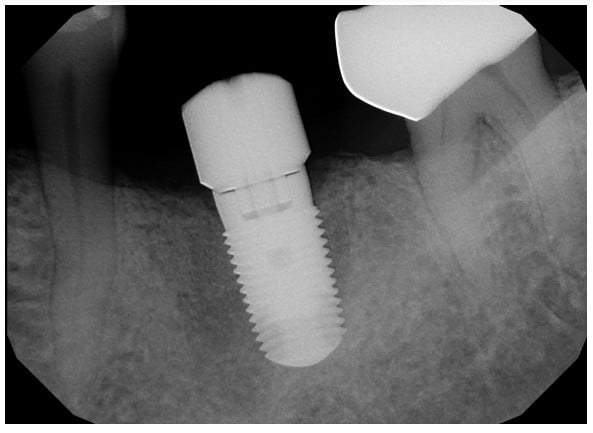
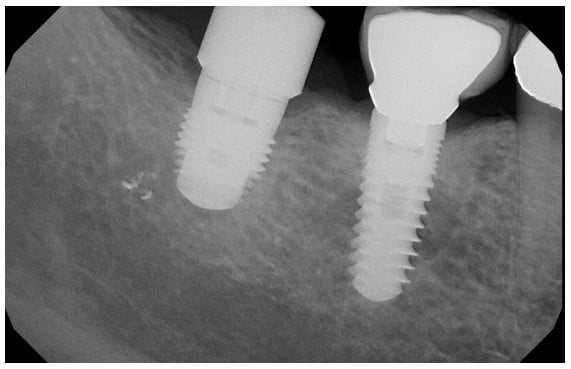
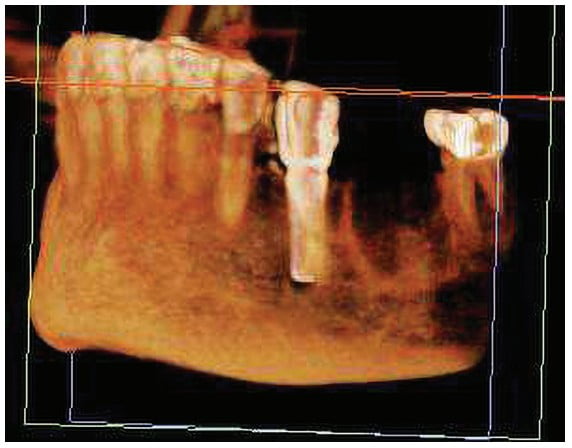
A 66-year-old female presented with a painful vertical root fracture, nonrestorable lower-right second molar (tooth No. 31) (Figure 7). Surgical extraction was performed, and a post-extraction CBCT was acquired (Figure 8). The socket was intact but with a thin buccal wall following extraction. The patient was instructed to use the VPro™ HFV oral device daily for 5 minutes post-extraction during the 4-month healing period. The patient returned 4 months later, a pre-implant CBCT was acquired, and the socket presented with osseous fill of sufficient density to retain an implant (Figure 9). A 6.0 mm x 8 mm implant was placed (Figure 10). Density was measured on the CBCT in Hounsfield units at an area in the extraction socket for the immediate extraction CBCT and again in the same spot on the post-healing CBCT, indicating an increase in density of the healed clot that was present in the socket initially (Table 1). For standardization, an area on the socket wall was compared at initial CBCT, and post-CBCT was measured for standardization on the patient indicating similar density values to bone outside the socket before-and-after use of HFV (Table 2). HFV allowed maintenance of the thin buccal wall without loss of height or thickness while yielding a dense vital socket fill ready for implant placement.

Case report No. 3
A 67-year-old female presented with a lower first molar (tooth No. 19) decayed to the core and nonrestorable (Figure 11). After surgical extraction was completed, a post-extraction CBCT was taken (Figure 12). The socket was intact. The patient was instructed to use the VPro™ HFV oral device daily for 5 minutes post-extraction during the 4.5-month healing period. The patient returned 4.5 months later, and a pre-implant CBCT was taken (Figure 13). Sufficient bone was present at the healed extraction socket to accommodate implant placement with sufficient bone thickness on the buccal and lingual between the planned implant and periosteum (Figure 14). A 6.0 mm x 11 mm implant was placed (Figure 15). Density was measured on the CBCT in Hounsfield units at an area in the extraction socket for the immediate extraction CBCT and again in the same spot on the post-healing CBCT, indicating an increase in density of the healed clot that was present in the socket initially (Table 1). For standardization, an area on the socket wall was compared at initial CBCT, and a post-CBCT was measured for standardization on the patient, indicating similar density values to bone outside the socket before-and-after use of HFV (Table 2). Sufficient osseous fill was achieved with maintenance of the crestal aspects of the extraction socket permitting a wider implant to be placed following the initial healing period.



Case report No. 4
A 63-year-old female presented with an abscessed and nonrestorable lower-left first molar (tooth No. 19) (Figure 16). The patient had a significant history of long-term use of bisphosphonates. An article by expert panelists of the American Dental Association Council on Scientific Affairs notes: “Bisphosphonates may carry a potential for severe suppression of bone turnover that may impair some of bone’s biomechanical and reparative properties.” However, the article continues, “The dentist, knowing the patient’s health history and vulnerability to oral disease, is in the best position to make treatment recommendations in the interest of each patient.”1 Surgical extraction was performed, and the socket was lined with granulation tissue that was curetted out to uncover the boney walls of the socket. The buccal plate was noted to be fully intact. A post-extraction CBCT was acquired (Figure 17). The patient was instructed to use the VPro™ HFV oral device daily for 5 minutes post-extraction during the 6-month healing period. When the patient returned 6 months later, a pre-implant CBCT was acquired (Figure 18). There was a large hole where the socket had been. Density was measured on the CBCT in Hounsfield units at an area in the extraction socket for the immediate extraction CBCT and again in the same spot on the post-healing CBCT indicating an increase in density of the healed clot that was present in the socket initially (Table 1).
For standardization, an area on the socket wall was compared at initial CBCT, and post-CBCT was measured for standardization on the patient indicating similar density values to bone outside the socket before-and-after use of HFV (Table 2). The socket was degranulated, grafted with a porcine xenograft (RegenerOSS® Xenograft, Zimmer Biomet) and covered with a pericardium membrane. Patients on long-term bisphosphonate drugs have osseous circulation issues that have been reported to potentially lead to osteonecrosis, and bone healing can be a challenge in this population. HFV aided in some socket fill and avoided potential osteonecrosis. Placement of graft material in the extraction socket of these patients at time of extraction combined with use of HFV may have yielded a higher volume of socket fill, then just leaving the clot to organize and convert to bone.

Case report No. 5
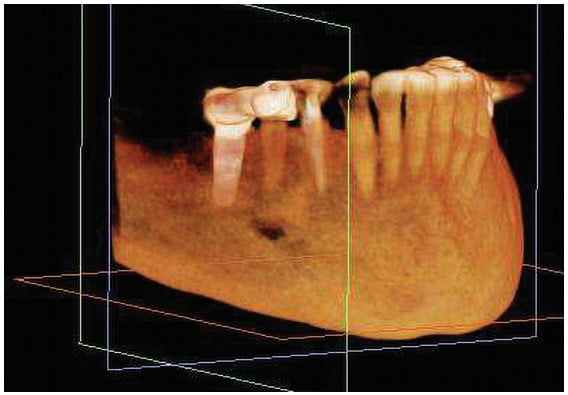
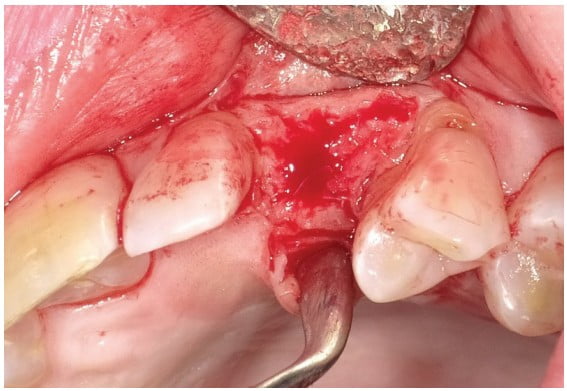
A 58-year-old female presented with deep distal decay and a nonrestorable maxillary left canine (tooth No. 11) (Figure 19). Surgical extraction was done, and a post-extraction CBCT was acquired. The patient was instructed to use the VPro™ HFV oral device daily for 5 minutes post-extraction during the 4-month healing period. The patient returned 4 months postsurgically, and pre-implant CBCT was acquired. Local anesthetic was administered, and the planned implant site was flapped to expose the prior extraction socket. The socket was filled with bone that felt dense when contacted with the periosteal elevator and appeared similar in density to adjacent bone (Figure 20). An osteotomy was performed, and a 3.5 mm x 11 mm implant was placed into the site with a healing abutment to allow osteointegration before the restorative phase would be initiated (Figure 21). Density was measured on the CBCT in Hounsfield units at an area in the extraction socket for the immediate extraction CBCT and again in the same spot on the post-healing CBCT indicating an increase in density of the healed clot that was present in the socket initially (Table 1). For standardization, an area on the socket wall was compared at initial CBCT and post-CBCT was measured for standardization on the patient indicating similar density values to bone outside the socket before-and-after use of HFV (Table 2). Healing demonstrated complete fill of the extraction socket with dense organized vital bone having converted over from the clot left in the socket following extraction.


Conclusion
The pandemic and shutdown lead to delays in treatment before the patients were able to return for follow-up and implant placement. Improvement in the osseous quality and density is typically observed with 3 months usage of the VPro. Kurtzman, et al., has noted that HFV, “has demonstrated an ability to increase bone density, stimulate growth factors increasing osteoblastic activity and angiogenesis accelerating graft conversion to host bone to allow earlier implant placement.”2 Four of the five cases presented in this article demonstrated dense bone at each extraction socket at uncovery of the healed ridge in anticipation of implant placement. The one case that required subsequent grafting was in a patient who was on long-term bisphosphonate medication, which affects osseous circulation, and some osseous fill occurred at the end of the initial healing but not sufficient for implant placement. Of the cases presented, three of the sockets received no graft material and were allowed to fill with a clot and heal naturally, aided by the HFV during the healing period. Those sockets demonstrated complete bone-fill with dense vital bone after the 4- to 6-month healing period, supporting that HFV has a positive impact on osseous healing and organization. For cases that were similarly followed without the use of HFV, significant increases in bone-fill and site density were noted in the HFV patients in comparison.
Read more about normalizing tooth mobility and improving bone with VPro for implant placement in Dr. Matthew Hallas’ article here: https://implantpracticeus.com/industry-news/high-frequency-vibration-for-normalizing-tooth-mobility-and-improving-bone-for-implant-a-case-study/
- Expert panel recommendations: American Dental Association Council on Scientific Affairs. Dental management of patients receiving oral bisphosphonate therapy. J Am Dent Assoc. 2006;137(8):1144-1150.
- Kurtzman GM, Horowitz RA, Hallas MB, El-Bialy T. Improving osseous conditions around teeth and implants utilizing high frequency vibration. [awaiting publication]
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 David W. Engen, DDS, MSD, is a Board-certified periodontist in private practice in Spokane, Washington. He has a master’s degree in bone physiology, as well as dual training in both Periodontics and Orthodontics. He is a graduate of Indiana University School of Dentistry and received his specialty training there as well. His master’s thesis was observing bone micro-damage around dental implants in the alveolar bone of dogs treated with various bisphosphonates.
David W. Engen, DDS, MSD, is a Board-certified periodontist in private practice in Spokane, Washington. He has a master’s degree in bone physiology, as well as dual training in both Periodontics and Orthodontics. He is a graduate of Indiana University School of Dentistry and received his specialty training there as well. His master’s thesis was observing bone micro-damage around dental implants in the alveolar bone of dogs treated with various bisphosphonates.
 Tarek El-Bialy, BDS MS PhD, is a tenured full-time professor of orthodontics and biomedical engineering at the University of Alberta, Canada. He received a BDS from Tanta University, Egypt, in 1987 and completed a Master’s degree in Orthodontics at Tanta University, Egypt. He received a law degree from Tanta University in 1994. He has successfully completed a certificate of specialty in Orthodontics, Master’s Degree in Oral Sciences and a PhD in Bioengineering at the University of Illinois at Chicago in 2000 and 2001. In addition, he completed an Executive Masters of Business and Administration (EMBA) at the University of Alberta, Canada in 2012. In addition, he recently (June 2019) received a doctoral degree from university of Bonn, Germany. A significant part of Dr. El-Bialy’s work was devoted to repair of orthodontically induced root resorption and biomechanics. Dr. El-Bialy is a fellow of the Royal College of Dentists of Canada (RCDC) and Diplomat of the American Board of Orthodontics. In addition, he is a senior research fellow, von Humboldt Foundation, Germany, since 2013. He also is the director of orthodontics at the RCDC board of directors. Dr. El-Bailey was the past president of the Alberta Society of Orthodontists.
Tarek El-Bialy, BDS MS PhD, is a tenured full-time professor of orthodontics and biomedical engineering at the University of Alberta, Canada. He received a BDS from Tanta University, Egypt, in 1987 and completed a Master’s degree in Orthodontics at Tanta University, Egypt. He received a law degree from Tanta University in 1994. He has successfully completed a certificate of specialty in Orthodontics, Master’s Degree in Oral Sciences and a PhD in Bioengineering at the University of Illinois at Chicago in 2000 and 2001. In addition, he completed an Executive Masters of Business and Administration (EMBA) at the University of Alberta, Canada in 2012. In addition, he recently (June 2019) received a doctoral degree from university of Bonn, Germany. A significant part of Dr. El-Bialy’s work was devoted to repair of orthodontically induced root resorption and biomechanics. Dr. El-Bialy is a fellow of the Royal College of Dentists of Canada (RCDC) and Diplomat of the American Board of Orthodontics. In addition, he is a senior research fellow, von Humboldt Foundation, Germany, since 2013. He also is the director of orthodontics at the RCDC board of directors. Dr. El-Bailey was the past president of the Alberta Society of Orthodontists.

