Dr. Todd Sheffler shows how different types of lasers have had beneficial effects on his implant practice.
Dr. Todd J. Sheffler discusses how lasers can optimize patient comfort and improve clinical efficacy
Failing dental implants are a significant concern for the implant dentist. No clinician places an implant with the expectation that is going to fail, yet the weighted mean prevalence of peri-implantitis is 22%.1 Various criteria for implant success or failure have been proposed over the last 40 years, starting in 1979.2 Consensus on the definition of success remains elusive. Regardless of the definition, optimizing the factors for implant success should be a priority when placing implants.
Many methods have been developed over the years to increase implant success. Implant manufacturers have manipulated designs of their implants for greater bone-to-implant contact (BIC). Manufacturers have developed new grafting materials and methods to increase implant success. New coating technologies have also been developed as well as new shapes and thread designs.
Dental laser companies have also made advances in the dental implant arena. Most of the early procedures involving lasers and implants focused on simple adjunct processes such as uncovering implants and hygiene maintenance around implants, i.e., laser pocket disinfection. After multiple laser manufacturers demonstrated the safety and success of laser pocket disinfection, research then switched to other implant-related procedures. As the incidence of failure grew, and no definitive treatment evolved, treating peri-implantitis via laser energy drew the attention of the entire industry. Nearly all laser manufacturers have published specific treatments to address peri-implantitis and implant mucositis.
I first incorporated dental lasers into my practice over 20 years ago. Throughout the years, I have purchased all types of dental lasers used in the United States. The goal has always been to optimize patient comfort with improving clinical efficacy. If a specific procedure does not benefit workflow or patient experience, it does not have a place in my practice. Using a laser “off-label” for applications similar to FDA-cleared uses requires a fundamental understanding of how each individual type of laser interacts with tissues.
As my experience with different lasers has deepened, I have incorporated specific benefits of each laser into my clinical workflow, increasing anesthesia-free restorations to reducing postoperative soreness. Leveraging this knowledge of laser physics, laser tissue interaction, and device specific parameters, I have adapted and evolved procedures to safely use lasers during implant placement and optimize the environment for implant success. Using this approach, we are seeing failure rates significantly lower than the industry average rates. Despite the increase in implant failures during the primary healing phase due to COVID exposure and elevated IL-6 levels currently being discussed, using a specific sequence of laser-based techniques during implant placement has improved success with this subset of patients as well.
Wavelengths, absorption, and physics — oh my!
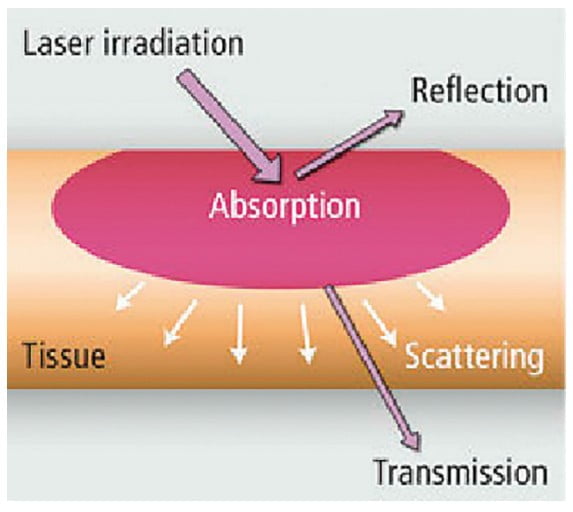
There are four different types of lasers commonly used today in dentistry — diode, erbium, CO2, and Nd:YAG. Each laser type represents a different wavelength, and each wavelength has its own absorption characteristics. I use all of these wavelengths in my practice. Laser light can be absorbed by tissue, reflected back, passed through tissue without absorption (transmission), or scattered in tissue (Figure 1). Diode and Nd:YAG wavelengths are absorbed in melanin and hemoglobin but pass through water and hydroxyapatite. Erbium and CO2 wavelengths are both absorbed in water and hydroxyapatite (Figure 2). Beyond wavelength, variable factors of each laser include pulse duration, length of pulse, spot size of beam, and energy density. One must understand these fundamentals of laser physics to understand the indications for lasers in surgery and accurately anticipate effects. This is critical when treating patients with various tissue types or on certain medications.
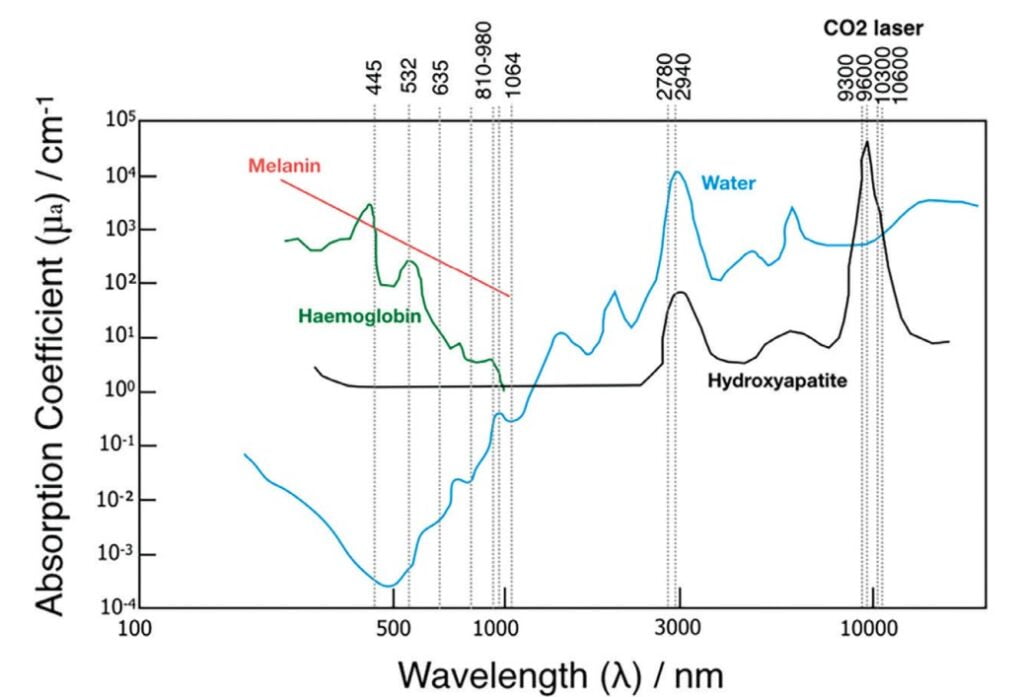
The most common dental laser is a diode laser, primarily due to price point. Diode lasers are electronic lasers where electrons are pumped through a p-n junction causing energy to be released as photons and operate in the 550-950 nm range. Diode lasers can be used in contact mode and non-contact mode. Diode lasers produce high heat and are absorbed in hemoglobin, melanin, water, and pigmented tissue. Most surgical procedures with a diode laser require an “initiated tip”; diodes do not have enough peak power on their own to efficiently cut tissue without initiation of the tip. Diode lasers are limited to soft tissue procedures.
Erbium lasers have a wavelength just under 3000 nm. These lasers are highly energy-efficient and accurate for photothermal ablation. Er:YAG has a 2940 nm wavelength and Er, Cr:YSSG is 2780 nm. While very similar, there is a difference in the water absorption between the two wavelengths. Overall, they behave in a comparable fashion. Their photothermal coagulation depths are significantly shorter than gingival blood vessel diameters. This makes erbium lasers great at cutting soft tissue but poor at coagulating.
CO2 lasers have gained popularity in the dental market in the past several years. CO2 lasers are primarily hard tissue lasers that function in the 10,600 nm wavelength. CO2 lasers are very efficient and exhibit excellent hemostasis as well as excellent tissue incision. CO2 lasers are ideal for incisional and excisional biopsies, frenectomies, gingivectomies, and for ablation and vaporization of leukoplakia and dysplasia.
Nd:YAG lasers are a near-infrared wavelength of 1064 nm. This wavelength is absorbed by pigment in the tissue, primarily hemoglobin and melanin. This wavelength can penetrate deeply into tissues, has excellent biostimulation properties, and can safely coagulate blood. Longer pulse duration settings can be used to stimulate fibrin formation. Nd:YAG lasers can be used for multiple soft tissue procedures such as periodontal treatments, gingivectomy, frenectomy, impression troughing, and biopsy.
Advantages of lasers in an implant practice
Lasers have several advantages over conventional surgical tools from patient perception to increased clinical convenience. No dental procedure starts without the consent of the patient. Before the patient can consent, they need to present into your office. We have found that highlighting technology in our marketing, including minimally invasive laser procedures, is an effective practice differentiator. Patients expect a certain level of technology. When we discuss laser treatment and indirectly show we have kept up with advances in the industry, patients exhibit a higher level of trust and acceptance. Indeed, both lasers and implants are perceived to be “fashionable treatments of modern dentistry.”
Clinically, lasers increase hemostasis, reduce damage to soft tissue resulting in less swelling and less postoperative pain for patients, and are effective at decontamination. These clinical benefits translate into a better patient experience. Studies have reported that laser technology is more effective at eliminating bacteria compared to chemical products, another appealing benefit to our patient base.
The body of evidence for procedures throughout the life-span of dental implants continues to support the usage of lasers around dental implants. Clinical papers by Kesler, Romanos, and Koren3 indicate the Er;Cr:YSGG laser can achieve osseointegration with less osseous tissue damage compared to conventional bur drilling in implant site preparation. Miller found laser ablation to be more effective at debridement around an implant compared to traditional acid wash.4 Misischia, et al., compare bacterial reduction of four lasers on titanium surfaces.5 Crippa, et al., discuss decontamination of infected or inflamed extraction sites via laser energy prior to immediate implant placements and the potential implications for long-term success.6 Kusek7 and Montoya-Salazar, et al.,8 presented cases of laser treatment with immediate implant placement, indicating shorter healing times than conventional methods.
Patient’s perspective
When your goal is to optimize patient comfort while improving clinical efficacy, getting patient feedback is essential. Patient-reported outcomes measures (PROMs) was one of the five major topics discussed at the 6th International Team for Implantology (ITI) conference. The consensus paper stressed that “understanding how patients respond to implant treatment is essential and that using PROMs can help clinicians in treatment planning.”
Over the last 20 years, I’ve placed thousands of dental implants. As my knowledge of laser physics expanded, I have utilized each laser to positively affect the implant site. What we have found in our practice is that patient acceptance rate is higher when incorporating laser procedures. Also, we are able to better control surgical variables and decrease healing times.
Expanding the focus of dental lasers
When effective solutions are found to address critical issues, the focus shifts from triage to prevention. Laser manufacturers have addressed how to save ailing implants and how to keep them healthy. The next evolution for dental laser manufacturers and laser dentists including myself, is exploring how to increase successful osseointegration with higher rates of BIC. The solution might be laser-assisted implant placement.
Biolase has published a case report by demonstrating immediate placement with loading in the esthetic zone using the Er,Cr:YSSG wavelength.9 LightScalpel’s (CO2 10,6000 nm) published case report combines laser degranulation and bacterial reduction with manual debridement before implant placement.10 Millennium Dental (PerioLase MVP-7, 1064 wavelength) has a new protocol which looks promising, but is not yet published. I have been using an approach to laser-assisted implant placement that is showing very promising results. Patient feedback is extremely positive, and the short-term implant success rates are higher with this approach.
Optimizing laser-implant procedures
Laser-assisted implant placement in my office has made for more successful implant outcomes, created happier patients who refer more frequently, a stronger implant warranty, and a doctor with less stress. We continue to follow the success of implants placed using this technique, and hopefully in the near future, I will be able to publish the details of my approach to laser-assisted implant placement.
Read more about the power of lasers in Peter Vitruk’s article, “Soft tissue laser dental surgery basics,” at https://implantpracticeus.com/ce-articles/soft-tissue-laser-dental-surgery-basics/
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015 Apr;42 Suppl 16:S158-711.
- Schnitman PA, Shulman LB. Recommendations of the consensus development conference on dental implants. J Am Dent Assoc. 1979 Mar;98(3):373-377.
- Kesler G, Romanos G, Koren R. Use of Er:YAG laser to improve osseointegration of titanium alloy implants–a comparison of bone healing. Int J Oral Maxillofac Implants. 2006 May-Jun;21(3):375-379.
- Miller RJ. Treatment of the contaminated implant surface using the Er,Cr:YSGG laser. Implant Dent. 2004 Jun;13(2):165-170.
- Misischia WP, Xenoudi P, Yukna RA, Schurr MJ. Bacterial reduction effect of four different dental lasers on titanium surfaces in vitro. Lasers Med Sci. 2021 Oct;36(8):1759-1767.
- Crippa R, Aiuto R, Dioguardi M, Peñarrocha-Diago M, Peñarrocha-Diago M, Angiero F. Laser Therapy for Infected Sites and Immediate Dental Implants in the Esthetic Zone: A Case Report and Review of Literature. Case Rep Dent. 2020 Jan 7;2020:2328398.
- Kusek ER. Immediate implant placement into infected sites: bacterial studies of the Hydroacoustic effects of the YSGG laser. J Oral Implantol. 2011 Mar;37 Spec No:205-11.
- Montoya-Salazar V, Castillo-Oyagüe R, Torres-Sánchez C, Lynch CD, Gutiérrez-Pérez JL, Torres-Lagares D. Outcome of single immediate implants placed in post-extraction infected and non-infected sites, restored with cemented crowns: a 3-year prospective study. J Dent. 2014 Jun;42(6):645-652.
- Savion A. Laser-assisted surgery before implant placement: a clinical case report. J Laser Assisted Dent. 2022:24-30. https://savion-c.co.il/wp-content/uploads/2022/10/LASER-ASSISTED-SURGERY.pdf. Accessed January 23, 2023.
- Linden E, Vitruk P. Seeing the Light: SuperPulse 10.6 micrometers CO2 laser-assisted, closed flap treatment of peri-implantitis. Implant Practice US. 2015;8(4):30-34.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Todd J Sheffler, DDS, is a 1991 graduate of the Baltimore College of Dental Surgery/The University of Maryland School of Dentistry. After graduating, Dr. Sheffler completed a General Practice Residency at the Baltimore VA Medical Center, where he was trained in surgical techniques and implant placement.
Todd J Sheffler, DDS, is a 1991 graduate of the Baltimore College of Dental Surgery/The University of Maryland School of Dentistry. After graduating, Dr. Sheffler completed a General Practice Residency at the Baltimore VA Medical Center, where he was trained in surgical techniques and implant placement.

