Drs. Spyridon I. Vassilopoulos and Michael Mastoris treat a case involving a frequent phenomenon
during childhood
Backround
Tooth loss after trauma is a frequent phenomenon during childhood, especially in the anterior maxillary area. Periapical lesions left untreated for a prolonged period of time can provoke an extended resorption of the labial plate, complicating future implant placement.
Introduction
Tooth loss after trauma is a frequent phenomenon during childhood and adolescence. Periapical lesions following tooth necrosis and other post-traumatic complications left untreated for a prolonged period of time can provoke an extended resorption of the labial plate of the alveolar ridge. When dental implants are included in the treatment plan, augmentation procedures of the resorbed buccal plate may be required in order to achieve initial stabilization of the implant in an anatomically appropriate location, especially in the anterior maxillary area, where implants have to satisfy both the long-term functional stability of the prosthetic restoration and the increased esthetic demands of the patient.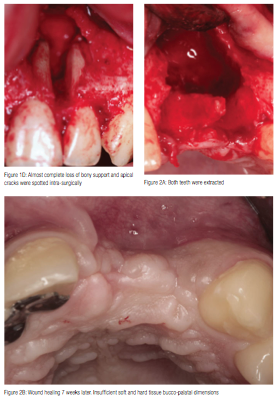
Case report
A 15-year-old, systematically healthy, regular smoker male, was referred to the practice by his pediatric dentist in October 2010 (Figure 1A). His chief complaints were swelling on the maxillary left labial area, accompanied by mobilization of teeth Nos. 21 and 22, and pain on percussion. Patient stated that he had an accident during a basketball game 5 years previously. Clinical examination revealed that teeth Nos. 21 and 22 were non-vital with degree III mobility and purulence associated to deep probing pocket depths of > 11 mm mesiodistally. Preoperative radiographical examination utilizing cone beam computed tomography (CBCT) (Accuitomo, J.Morita, Japan) showed a U-shaped periapical lesion extending 0.5 mm away from the floor of the nasal cavity (Figures 1B and 1C). The patient was instructed to follow a smoking cessation program prior to any surgical intervention.
Because of the increased possibility of root fractures or cracks on either or both of the involved teeth, a diagnostic, full thickness mucoperiosteal flap was elevated in advance of root canal therapies (Figure 1D). After meticulous degranulation of the defect, apical cracks were spotted, and both teeth were extracted (Figure 2A). Possible remnants of inflammation in addition to the insufficient soft tissue volume overlying the extremely resorbed buccal part of the alveolar ridge led to the delay of any bone regeneration attempt until complete wound healing was achieved. A temporary Rochette-type bridge was delivered to the patient in order to satisfy his increased functional, phonetic, and esthetic needs.
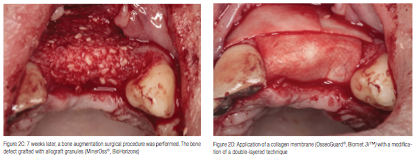
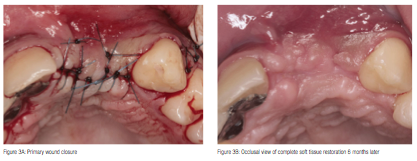
Seven weeks later, the uneventfully healed soft tissues were depressed buccally, indicating the extension of the underlying bone loss (Figure 2B). A bone augmentation surgical procedure was performed starting with infiltration of local anesthetic (4% articaine, 1:100,000 epinephrine) and, subsequently, elevation of full thickness buccal and palatal flaps extending from cuspid to cuspid with vertical releasing incisions buccally. The exposed bone defect was grafted with a mixture of allograft mineralized cortical and cancellous chips (MinerOss®, BioHorizons) (Figure 2C). A resorbable collagen membrane (OsseoGuard®, Biomet 3i) was trimmed and carefully adapted over the grafted site (Figure 2D), and then stabilized under the flaps without the need of tucking or suturing. In order to achieve full coverage of the regenerative materials, the site was closed with mucosal advancement flap using releasing incisions of the periosteum, as necessary. Mattress sutures were placed to secure the membrane under the flap and reduce the tension of the flap, while a second superficial layer of simple interrupted sutures facilitated primary closure of the surgical wound (Figure 3A). The patient was given medication consisting of amoxicillin, (500 mg, q.i.d/7 days), nimesulide, (100 mg, b.i.d/5 days), and chlorhexidine gluconate mouth rinse (0.12%, b.i.d/21 days).
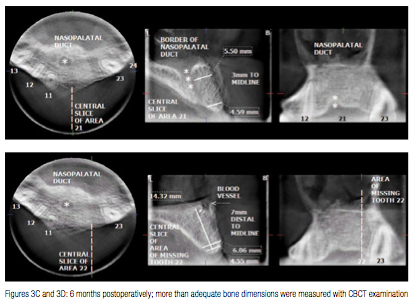
Six months post-surgically, the patient returned for evaluation. Clinical examination revealed complete soft tissue restoration bucco-palataly (Figure 3B). CBCT and hand-wrist films were also obtained. Although more than adequate bone dimensions were noted, confirming the success of the buccal bone augmentation (Figures 3C and 3D), the nearly complete radial epiphyseal closure in conjunction with patient’s chronological age (15, 8/12 years old) dictated the delay of implant placement.
Comments
The loss of bone volume after tooth extraction, according to Schropp, et al. (2003)2, amounts 5-7 mm horizontally (approximately 50% of the original alveolar bone with) and only 1 mm vertically, within the first 10 months. In the case of more extended horizontal alveolar bone crest deficiencies caused by tooth necrosis or other untreated post-traumatic complications, simultaneous implant placement should be avoided since there is not enough bone to achieve both primary implant stability and an optimal prosthetic-driven implant positioning. Under these circumstances, a staged protocol, which will address the lateral bone augmentation first and the implant placement in a second stage, is highly recommended.3 Furthermore, for the growing patient, this “waiting” period of 6-8 months until adequate maturation of the regenerated bone occurs, can spare the time needed for the completion of growth. Bone augmentation procedures can be applicable during growth, since the regenerated bone will follow the developing pattern of the growing maxilla. Implants placed into regenerated bone show similar success rate with implants placed into pristine bone.4 Even in severely resorbed alveolar ridges, guided bone regeneration techniques utilizing allografts and/or xenografts in conjunction with bioabsorbable or non-resorbable barrier membranes can create an osteoconductive scaffold, providing volume enhancement and effective site development for successful bone remodeling and future implant placement. Avoiding the second surgical trauma in order to obtain an autologous bone block graft from the donor site may be beneficial for the young patient since it reduces the operative time needed and the post-surgical discomfort.5
In order to evaluate the total amount of bone loss and osseous destruction in three dimensions, cone beam computed tomography (Accuitomo, J.Morita, Japan) examination of that area was performed. The anatomic area to be scanned was restricted, so that only the region of interest was examined, resulting in a radiation dose similar to a panoramic radiograph. This major advantage offers the possibility of repeating the examination, especially in young patients, in order to evaluate the outcome of the surgical procedure and the quality/quantity of newly formatted bone as well as the blending of the grafting material.6
For the growing child or adolescent, early implantation is not recommended, since osseointegrated implants behave like ankylosed teeth, jeopardizing the long-term esthetic and functional outcome of the implant supported restoration, particularly in the anterior maxillary area. Thilander, et al.,7 followed 15 adolescents (13 to 19 years old) with 27 implants for a period of 10 years. Mean infraocclusion of the implants was 1.0 mm (range 0.1 to 2.2 mm), possibly causing marginal bone loss around the adjacent teeth. A clear correlation was recorded between body length growth and the extent of implant infraocclusion after 3 years of loading. Interestingly, from the fourth year on, the relative infraocclussion increased (mean of 0.5± 0.6 mm) despite the fact that no further length growth or craniofacial alterations could be measured. Growth of the maxilla in a vertical direction occurs as a combined result of suture growth; bone remodeling in the orbits, the nasal cavity, and the maxillary sinuses; and continued teeth eruption. Vertical growth of the maxilla continues beyond the age at which transverse and sagittal growth cease. To prevent implant infraocclusion or bucco-lingual disharmony or, even more, a potential interfering with growing pattern of the jaws,8 it is advisable to delay implant placement until the age of 17 or 18 years for girls and somewhat later for boys.9
Acknowledgments: This case report was awarded with J. Morita prize “Case report’’ at the 23rd Congress of the International Association of Paediatric Dentistry, June 2011, Athens, Greece.
Conflict of interest: Authors have declared no conflict of interest.
References
1. Schwartz-Arad D, Levin L, Ashkenazi M. Treatment options of untreatable traumatized anterior maxillary teeth for future use of dental implantation. Implant Dent. 2004; 13(2):120-128.
2. Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323.
3. Behr M, Driemel O, Mertins V, Gerlach T, Kolbeck C, Rohr N, Reichert TE, Handel G. Concepts for the treatment of adolescent patients with missing permanent teeth. Oral Maxillofac Surg. 2008;12(2):49-60.
4. Oesterle LJ, Cronin RJ Jr, Ranly DM. Maxillary implants and the growing patient. Int J Oral Maxillofac Implants. 1993;8(4):377-387.
5. McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007:78(3);377-396.
6. Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Grondahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008;37(2):72-79.
7. Thilander B, Odman J, Lekholm U. Orthodontic aspects of the use of oral implants in adolescents: A 10-year follow-up study. Eur J Orthod. 2001;23(6):715-731.
8. Odman J, Grondahl K, Lekholm U, Thilander B. The effect of osseointegrated implants on the dento-alveolar development. A clinical and radiographic study in growing pigs. Eur J Orthod. 1991;13(4):279-286.
9. Heij DG, Opdebeeck H, van Steenberghe D, Kokich VG, Belser U, Quirynen M. Facial development, continuous tooth eruption, and mesial drift as compromising factors for implant placement. Int J Oral Maxillofac Implants. 2006;21(6):867-878.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Drs. Spyridon I. Vassilopoulos and Michael Mastoris treat a case involving a frequent phenomenon
Drs. Spyridon I. Vassilopoulos and Michael Mastoris treat a case involving a frequent phenomenon 
