Educational aims and objectives This self-instructional course for dentists aims to discuss the usage of ultra-narrow diameter implants to treat narrow edentulous spaces without additional bone grafting procedures. Expected outcomes Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Review limitations of freehand implant surgery.
- Identify static-guided implant surgery workflows.
- Recognize limitations of conventional-sized implants in narrow edentulous spaces.
- Realize the benefits of guided implant surgery in idealizing positioning of ultra-narrow diameter implants.
Dr. Paul Mozer shows how ultra-narrow diameter implants together with guided surgery can help to avoid bone grafting and other issues in a narrow ridge.
Dr. Paul Mozer discusses guided implant surgery with narrow diameter implants
Successful implant surgery is in large measure reliant upon the accurate position of the implant and its prosthetic components.1,2 The overloading of the implant body or its prosthetics have been considered by several studies that specifically addressed the concerns that arise from poor implant positioning. Weinberg, et al., in 1995 articulated the force magnifiers that resulted from improper implant placement and described the concepts of cuspal inclination, implant inclination, horizontal implant offset, and apical implant offset.3 Directional displacement of the implant away from its intended position resulting from variations in vertical, horizontal, and depth positioning resulted in substantial increases in force transmitted to the implant and its prosthetics. These increased forces can lead to premature prosthetic component wear, prosthetic failure, bone loss, and implant loss.3
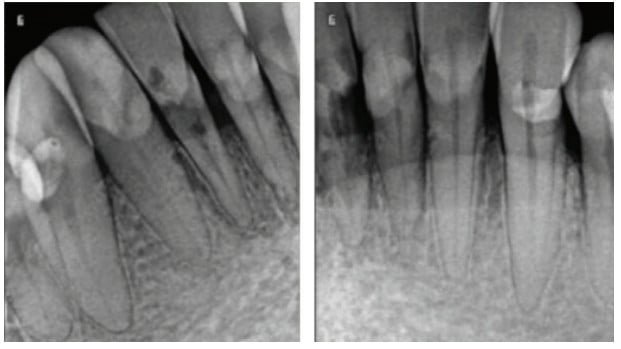
Historically, clinicians used two-dimensional panoramic X-rays, bone mapping using ridge calipers, and open-flap measurements, among other techniques to measure the width and height of the residual ridge before and during implant placement. Most often final implant size and position were determined chairside with the surgical site flapped open. These approaches alone or in combination all yielded significant gaps in critical clinical information since these methods all lacked the appreciation of the three-dimensionality of bone.4,5,6
Many studies have described the challenges of freehand implant surgery under normal conditions. Hoffman, et al., performed a model-based study in which the mean angle deviation between planned implants and final implant placement was 11 degrees with a range from 4.1 to 25.3 degrees.7 A malpositioned implant with an 11-degree angulation would have potentially significant and long-lasting consequences on the implant and its prosthetics.
Three-dimensional cone beam imaging has opened the door for clinicians to assess bone density and volume before performing the implant procedure.5,6 Computer-aided design and manufacturing (CAD/CAM) can be utilized to plan ideal implant positions in implant software and bring those ideal surgical plans to the patient using static stereolithographic (STL) static surgical guides.7,8 Surgical guides allow clinicians to increase the predictability of implant placement8 while limiting the negative outcomes of implant malposition and force multipliers. Guided surgery drill kits provided by the implant manufacturer restrict the drill path by engaging the guide sleeve within the STL surgical guide.13
Studies by Hoffman, et al., and Choi, et al., show a 50% or greater improvement in implant position accuracy utilizing static surgical guides over freehand methods. The advantages of guided surgery become critical in complicated cases where bone volume or bone density require precision that can be difficult to achieve with freehand implant placement.7,14
Edentulous areas with a narrow ridge that is deficient in width and/or height have traditionally undergone a bone augmentation procedure prior to implant placement. Augmentation with bone blocks, bone plates, or ridge-splitting procedures are technique-sensitive, costly, and can result in comorbidities such as a second surgical site dehiscence or a final implant site with a remaining width deficiency.11 Narrow interdental edentulous spaces such as maxillary lateral incisors and mandibular incisors are unique in that except for orthodontic arch expansion, the adjacent teeth prevent bone grafting as a solution to gain more space for a larger implant diameter. As implant material science has advanced, narrow diameter two-piece implant designs have allowed clinicians and patients to set aside traditional grafting techniques and utilize narrow (3.0 mm-3.25 mm) and ultra-narrow (2.75 mm) diameter implants with measurable success. A systematic review by Schiegnitz and a study by Grandi both show the success of ultra-narrow diameter 2.75 mm implants to be between 94.7 and 97.6%, results that are consistent with the success of more traditional sized implants.16,17

Clinical case
The patient presented with the diagnosis of unrestorable external resorption of teeth Nos. 25, 26, 27 in the anterior mandible. A cone beam image was taken using the i-CAT™ FLX (Imaging Sciences, Hatfield, Pennsylvania). Analysis showed very thin bone surrounding the existing teeth with a density of 1243-1383 Hounsfield units, suggesting very dense Type I bone. Treatment-planning options for a narrow ridge included the options of onlay block grafting with delayed implant placement and the disadvantages of a second surgical site, comorbidities, and technique-sensitive surgical procedures. The traditional prosthetic dental options of a lower partial denture and fixed bridge were alternatives that were less than desirable for the patient. The patient ultimately opted for implant placements.
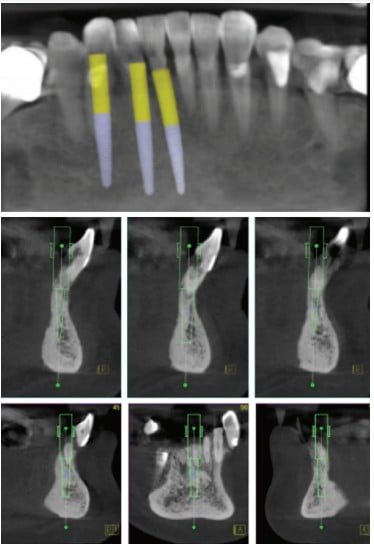
In this case, the ultra-narrow platform Adin Touareg CloseFit™ 2.75mm diameter implants (Adin Implants Afula, Israel) were treatment planned for guided surgery using 360Imaging™ (Atlanta, Georgia) surgical guides. The workflow included a three dimensional cone beam image taken at the consultation appointment along with physical polyvinyl siloxane impressions (3M™, St. Paul, Minnesota) for interim prosthesis fabrication and a digital impression of the clinical arch (Cerec Omnicam, Dentsply Sirona, Salzburg, Austria) for surgical guide planning. The collected data was sent to 360Imaging through its online courier service for analysis and treatment planning. Treatment planning was performed collaboratively between the clinician and the dentist treatment planners at 360Imaging via Zoom (San Jose, California) and screenshare technology. The teeth were digitally extracted, and the final implant positions were planned in 360dps software (360Imaging, Atlanta, Georgia). Static STL surgical guides were fabricated and delivered to the clinician’s practice within a few days.

The day of the procedure, consent was obtained, amoxicillin 2G was given to the patient before the procedure and 2.5 carpules of articaine 4% 1:100k epinephrine local anesthetic was administered (Septodont, Lancaster, Pennsylvania). The affected teeth were extracted as atraumatically as possible using forceps. The positive seating of the surgical guided was verified clinically, and three Adin Touareg CloseFit 2.75 mm ultra-narrow diameter implants were immediately placed using the static surgical guides and Adin’s keyless guided surgery kit (Adin Implants, Afula, Israel). Cover screws were placed and torqued to 15Ncm, and particulate bone grafts with BioOss® (Geistlich, Wolhusen, Switzerland) were placed with aPRF and iPRF using the Choukroun Duo Quattro PRF™ Centrifuge (Advanced Platelet Rich Fibrin, Choukroun Centrifuge Nice, France). A BioGide® cross-linked collagen membrane (Geistlich, Wolhusen, Switzerland) was placed over the grafted site and tension-free PGA (polyglycolic acid) sutures were placed. Hemostasis was observed. The previously fabricated temporary removable prosthesis was adjusted chairside and delivered to the patient, making sure that there was no positive pressure on the ridge from the interim prosthesis. The patient was placed on a postoperative regimen of Ibuprofen 800mg every 4 hours for the first 24 hours and Amoxicillin 500mg 3 times daily, warm salt water rinses 5-6 times per day, and 0.12% Chlorhexidine rinses twice daily for 7 days. The patient was seen for suture removal 10 days after the procedure, and oral hygiene instructions were reinforced.
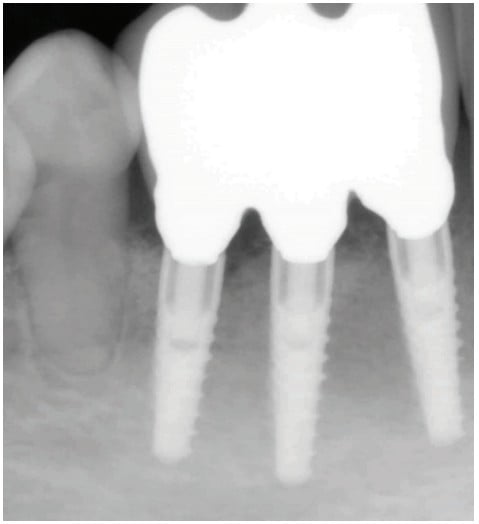
After 4 months of healing, the site was uncovered, healing abutments placed for tissue contouring, and an open tray impression was taken with Impregum™ (3M™, St. Paul, Minnesota). Three splinted screw-retained crowns were inserted and torqued to 35Ncm. The lingual screw accesses were covered with PTFE Teflon tape, resin restorations were placed, and the occlusion was adjusted where necessary. Oral hygiene was reviewed, and the patient was seen 3 weeks later for an occlusal reassessment.

In a freehand implant placement surgical approach, obtaining optimal positioning in Type I bone can be clinically challenging for a single implant. In this particular case, the patient presented with a narrow mandibular anterior edentulous space that required precision placement of three implants in narrow and dense bone. The ability to achieve the ideal placement required for multiple placements of ultra-narrow implants with screw-retained crowns would have proven very difficult. As indicated in Figure 7B, screw access was through the cingulum on the lingual aspect of the prosthetics. Static-guided implant surgery utilizing the Adin’s ultra-narrow 2.75 mm implants allows implant placements in dense thin bone to be as predictable as 5.0 mm implants in a wide edentulous ridge.
After reading about ultra-narrow diameter implants, read Dr. Gary Shapoff’s experience in his article, “Treating compromised sites with narrow implants.” Read it here: https://implantpracticeus.com/treating-compromised-sites-with-narrow-implants/.
References
- Becker CM, Kaiser DA. Surgical guide for dental implant placement. J Prosthet Dent. 2000;83(2):248-251.
- Garber DA, Belser UC. Restoration-driven implant placement with restoration-generated site development. Compend Contin Educ Dent. 1995;16(8):796,798-802,804.
- Weinberg LA, Kruger B. A comparison of implant/prosthesis loading with four clinical variables. Int J Prosthodont. 1995;8(5):421-433.
- Gahleitner A, Watzek G, Imhof H. Dental CT: imaging technique, anatomy, and pathologic conditions of the jaws. Eur Radiol. 2003;13(2):366-376.
- Nickenig HJ, Eitner S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg. 2007; 35(4-5):207-211.
- Ozan O, Turkyilmaz I, Ersoy AE, et al., Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 2009;67(2):394-401.
- Hoffmann J, Westendorff C, Gomez-Roman G, Reinert S. Accuracy of navigation-guided socket drilling before implant installation compared to the conventional free-hand method in a synthetic edentulous lower jaw model. Clin Oral Implants Res. 2005;16(5):609-614.
- D’Souza KM, Aras MA. Types of implant surgical guides in dentistry: a review. J Oral Implantol. 2012;38(5):643-652.
- Cassetta M, Stefanelli LV, Giansanti M, Di Mambro A, Calasso S. Depth deviation and occurrence of early surgical complications or unexpected events using a single stereolithographic surgi-guide. Int J Oral Maxillofac Surg. 2011;40(12):1377-1387.
- Marchack CB. CAD/CAM-guided implant surgery and fabrication of an immediately loaded prosthesis for a partially edentulous patient. J Prosthet Dent. 2007;97(6):389-394.
- Park C, Raigrodski AJ, Rosen J, Spiekerman C, London RM. Accuracy of implant placement using precision surgical guides with varying occlusogingival heights: an in vitro study. J Prosthet Dent. 2009;101(6):372-381.
- Holst S, Blatz MB, Eitner S. Precision for computer-guided implant placement: using 3D planning software and fixed intraoral reference points. J Oral Maxillofac Surg. 2007;65(3):393-399.
- Koop R, Vercruyssen M, Vermeulen K, Quirynen M. Tolerance within the sleeve inserts of different surgical guides for guided implant surgery. Clin Oral Implants Res. 2013;24(6):630-634.
- Choi W, Nguyen BC, Doan A, Girod S, Gaudilliere B, Gaudilliere D. Freehand Versus Guided Surgery: Factors Influencing Accuracy of Dental Implant Placement. Implant Dent. 2017;26(4):500-509.
- Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants—a Cochrane systematic review. Eur J Oral Implantol. 2009;2(3):167-184
- Schiegnitz E, Al-Nawas B. Narrow-diameter implants: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(Suppl 16):21-40.
- Grandi T, Svezia L, Grandi G. Narrow implants (2.75 and 3.25 mm diameter) supporting a fixed splinted prostheses in posterior regions of mandible: one-year results from a prospective cohort study.Int J Implant Dent. 2017;3(1):43.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Paul Mozer, DDS, MSc, DICOI, graduated from University at Buffalo School of Dental Medicine where he received academic distinction and clinical commendations. He conducted oral cancer research at Roswell Park Cancer Institute and completed a residency at New York Medical College. Dr. Mozer has a Master of Science Degree in Oral Implantology from the University of Frankfurt Goethe Dental School, where he is on faculty lecturing on guided implant surgery and serves as a Clinical Supervisor and Advisor to Master Thesis candidates. Dr. Mozer is also on the faculty of the AAID MaxiCourse® in Boston, Massachusetts; St. Peters Hospital in Albany, New York; and the VA Hospital in Buffalo, New York. He has conducted clinical research in static and robotic guided implant surgery and is both a Diplomate and Fellow in International Congress of Oral Implantologists. Disclosure: Dr. Mozer has no financial interest in any of the companies mentioned in this article and has not received compensation for this article. Dr. Mozer is a key opinion leader for Adin Implants and 360Imaging.
Paul Mozer, DDS, MSc, DICOI, graduated from University at Buffalo School of Dental Medicine where he received academic distinction and clinical commendations. He conducted oral cancer research at Roswell Park Cancer Institute and completed a residency at New York Medical College. Dr. Mozer has a Master of Science Degree in Oral Implantology from the University of Frankfurt Goethe Dental School, where he is on faculty lecturing on guided implant surgery and serves as a Clinical Supervisor and Advisor to Master Thesis candidates. Dr. Mozer is also on the faculty of the AAID MaxiCourse® in Boston, Massachusetts; St. Peters Hospital in Albany, New York; and the VA Hospital in Buffalo, New York. He has conducted clinical research in static and robotic guided implant surgery and is both a Diplomate and Fellow in International Congress of Oral Implantologists. Disclosure: Dr. Mozer has no financial interest in any of the companies mentioned in this article and has not received compensation for this article. Dr. Mozer is a key opinion leader for Adin Implants and 360Imaging. 

