Educational aims and objectives
This self-instructional course for dentists aims to discuss the benefits and drawbacks of different staging protocols of implant surgery as well as the pros and cons of free-hand versus guided implant surgery.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Identify the 2 main types of implant placement.
• Identify the pros and cons of each method of placement.
• Discuss the advantages and disadvantages of freehand versus guided implant placement.
• Better understand the positive aspects of guided implant surgery.
• Realize how to evaluate and assess an implant case and make an informed decision on plan of surgical treatment.
Dr. Jaclyn A. Tomsic writes about implant placement timing as well as the differences between free-hand and guided surgery techniques.
Dr. Jaclyn A. Tomsic offers guidance on the timing of implant protocols and methods for more efficient placement
Implant dentistry has evolved immensely since Brånemark initially introduced the concept of osseointegration in the late 1960s. Perhaps one of the most common and intensely debated topics today is the debate between when to pursue the traditional 2-stage protocol versus a 1-stage implant surgery.
In the traditional 2-stage approach, a tooth is extracted and ideally bone grafted for socket preservation. Traditionally, a 3-month waiting period is suggested for soft and hard tissue healing before placing a dental implant.1 At this point, with successful remodeling of the bone graft, a dental implant is placed. The implant is either initially completely submerged under mucosal tissue during the healing process, or more recently, if appropriate primary stability is achieved, a healing abutment is directly connected to the implant fixture at the time of implant surgery. In both situations, an attempt is made to avoid any functional loading during the initial osseointegration process, again typically 12 weeks or 3 months.1 If the implant is buried, it is uncovered in a second minor surgery typically 12 weeks later. If a healing abutment is in place, a final check appointment is still required to check successful osseointegration before sending to the restorative doctor. This 2-stage protocol (of placing an implant in a healed socket and subsequently restoring the implant with a prosthesis) is recognized as a highly predictable treatment modality for partially edentulous patients. This 3-month period has evolved from the original 6-month post extraction healing protocol first introduced by Brånemark.1
As products, knowledge, and experience evolve and improve over time, we have devised alternate ways to accomplish the same goal; thus the one-stage implant placement approach was born. In the 1-stage approach, an implant is placed immediately in a fresh extraction socket, often in combination with bone grafting, guided tissue regeneration, and sometimes immediate restoration. The surgeon extracts a tooth as atraumatically as possible, aiming to preserve as much surrounding bone as possible to be able to attempt immediate implant placement. Over time, this approach has also proven to be successful with no significant differences in treatment outcomes when compared to the 2-stage approach.2
“More evidence is pointing toward the use of surgical guides as providing better implant placement accuracy and addressing these two factors of angulation and position.”
Pros and cons of the 2-stage approach
The 2-stage approach has long proven to be a highly predicable and successful method.1 A titanium surface under the appropriate circumstances in the absence of local or systematic disease or infection and without any other determining factors, if left untouched, will osseointegrate and fuse directly with human bone over time. A 3-month osseointegration period has repeatedly shown to be sufficient and reliable, and many long-term studies support this.1 The major drawback of the 2-stage approach is the duration and length of time from start to finish. If starting from the day of extraction, it will take about 6 months before a patient can expect to have a tooth again. For many, this is acceptable. Others want a more efficient timeline. From this, the 1-stage protocol emerged.
Pros and cons of the 1-stage approach
The 1-stage implant placement protocol involves placement of an immediate implant.
Documented pros of immediate implant placement include the following:3
- decreased treatment time
- fewer surgical procedures
- less traumatic surgery
- greater patient satisfaction.
- Cons include the following:3
- difficulty in achieving primary stability
- higher risk of failure
- more need for bone grafts
- increased infection risk
This technique has unpredictable soft and hard tissue levels, which in my opinion, can be both a pro and a con. On the one hand, the unpredictability can make it more difficult to present a definitive treatment plan to the patient and increase the need for more regenerative procedures such as bone grafting and guided bone regeneration (GBR). On the other hand, placing an implant in an atraumatic extraction socket where the clinician has been able to preserve the keratinized tissue, gingival structures, and bone can improve implant placement accuracy and lead to better cosmetic outcomes.
Techniques for implant placement
There are essentially three different techniques for implant placement.
Free-hand placement
First is free-hand placement — when surgeons combine the clinical exam with imaging to plan and place an implant. The alveolar bone width is assessed with periapical, panoramic, and three-dimensional cone beam computed tomography (CBCT) to help evaluate and profile the surrounding structures. Periodontal probes, gauges, and calipers are used to sound the bone and measure tissue to get an idea of the height and thickness of the ridge and tissue.
Adjacent and opposing teeth help determine the correct position. Tissue flaps are reflected for direct visualization. Position pins may be used during osteotomy preparation and intraoral imaging to check distances and angulations before final implant placement, and the implant and bone grafts with PRF (platelet rich fibrin) and GBR can be easily performed.
Fully guided placement
In fully guided, A CBCT is taken and converted into a DICOM file; this is accompanied by a digital intraoral impression. This information is merged into the implant-planning software, and the surgeon and often an implant planner, such as a laboratory technician from an outside dental laboratory, place the implant virtually in the best location. Based on this design, a surgical guide is made and sent to the surgeon for use during surgery. In truly fully guided surgery, the entire osteotomy is prepped through the guide, and the implant is placed through the guide.
Half-guided surgery
Lastly there is half-guided surgery. Half guided splits the difference; it is template-based surgically guided osteotomy preparation and free-handed manual implant insertion.
This is essentially a guide with a pilot-hole guide.
Aspects of guided surgery
I will now focus on guided surgery. The two most important factors in successful implant placement are angulation and positioning. Is poor angulation and positioning really that bad? Only the clinician can be the judge of that, but what we do know are the potential risks of taking that path. Perforations of the lingual plate or IAN can occur. The prosthetic can be compromised causing poor esthetics or unfavorable occlusal forces to be transmitted to the implants. Inaccurate or non-ideal inter-implant or implant-tooth distance can lead to loss of crestal bone and papilla contour.
More evidence is pointing toward the use of surgical guides as providing better implant placement accuracy and addressing these two factors of angulation and position.
There are obviously cases in which I choose to use free-hand surgery; however, the treating clinician should always make the individual decision as to whether free-hand or a surgical guide would be best for each case.

Case presentation
This 65-year-old female presented for implant consultation due to a failed root canal No. 7, whose crown was hanging on by a thread.
Things that were considered during my exam and planning process:
- The site to be implanted was tooth borne.
- The patient had adequate inter-occlusal distance and good overjet.
- Her clinical and radiographic exam showed a robust buccal plate and adequate palatal bone.
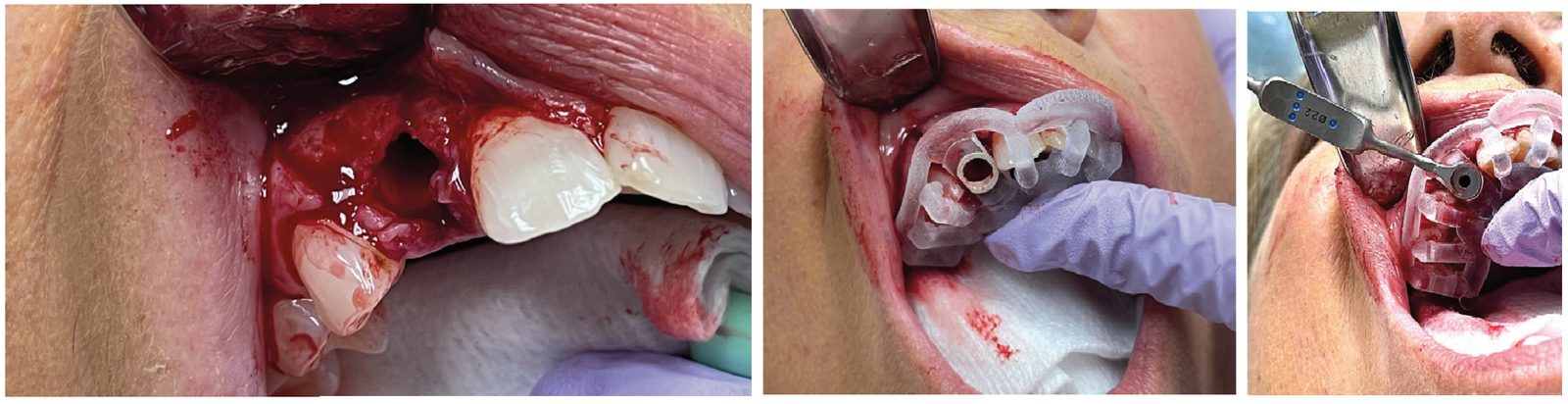
With this information, I proposed extraction and immediate implant placement using a fully guided surgical approach for placement of a Straumann® BLX implant.

I felt the immediate placement would give me the best M-D and B-P accuracy, and the use of a surgical guide would counteract the tendency of the drill to be driven off course during placement. Her atraumatic flipper was already fabricated by her general dentist and ready for placement postoperatively.
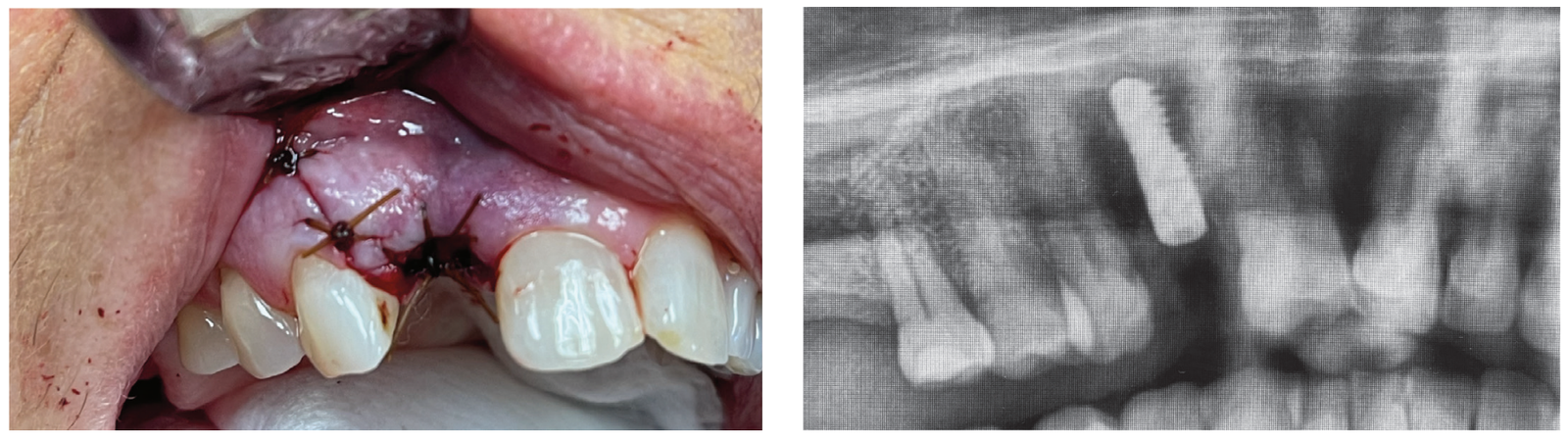
I was very happy with the outcome of this case. Takeaways from the case include:
- Position and angulation accuracy were maintained as planned.
- Drill and implant did not drive off course.
- Treatment time was efficient – surgery in <1 hour.
- Patient (and surgeon) left happy.
In conclusion, my decision to perform a fully guided surgical plan and technique in this case improved the accuracy, efficiency, and success of the surgery. I feel the outcome of this case will be better with the aid of a virtually planned case and surgical guide, especially in the setting of an immediate extraction site where the osteotomy position, shape, and angulation are harder to control than a well-healed alveolar ridge.
Implant placement timing can affect esthetics. Read Dr. David Wong’s artcle on “Surgical strategies for preventing poor implant esthetics” here: https://implantpracticeus.com/ce-articles/surgical-strategies-for-preventing-poor-implant-esthetics/
References
- Bassir SH, El Kholy K, Chen CY, Lee KH, Intini G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J Periodontol. 2019 May;90(5):493-506. doi: 10.1002/JPER.18-0338. Epub 2018 Dec 5. PMID: 30395355; PMCID: PMC6500770.
- Byrne G. Outcomes of one-stage versus two-stage implant placement. J Am Dent Assoc. 2010; 141(10):1257-1258.
- Meng HW, Chien EY, Chien HH. Immediate Implant Placement and Provisionalization in the Esthetic Zone: A 6.5-Year Follow-Up and Literature Review. Case Rep Dent. 2021 Sep 15;2021:4290193. doi: 10.1155/2021/4290193. PMID: 34567810; PMCID: PMC8457954.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Jaclyn Tomsic MD, DMD, FACS, is an oral and maxillofacial surgeon from Cleveland, Ohio specializing in topics such as: wisdom teeth, dental implants, corrective jaw surgery, facial cosmetic surgery, anesthesia, snoring and sleep apnea, the temporomandibular joint (TMJ), oral cancer, implants, and treating and preventing facial injury.
Jaclyn Tomsic MD, DMD, FACS, is an oral and maxillofacial surgeon from Cleveland, Ohio specializing in topics such as: wisdom teeth, dental implants, corrective jaw surgery, facial cosmetic surgery, anesthesia, snoring and sleep apnea, the temporomandibular joint (TMJ), oral cancer, implants, and treating and preventing facial injury.

