 Dr. Adam Patel details the huge potential of piezosurgery for improving the predictability and ease of dental implant treatment
Dr. Adam Patel details the huge potential of piezosurgery for improving the predictability and ease of dental implant treatment
Piezosurgery was first introduced in 1988. Its development was encouraged by the need for high levels of precision and safety in bone surgery compared with that achieved by standard bur and saw instruments (Landes, et al., 2008).
Piezosurgery as a technique spread because of its ease of use and safety. The piezoelectric effect occurs when an electric current is passed around a stack of crystals, and they start to vibrate at a precise frequency. The piezoelectric instrument produces a modulated ultrasonic frequency of 24 to 29kHz, and a microvibration amplitude between 60 and 200 mm/sec (Sortino, et al., 2008). The amplitude of these microvibrations allows a clean, precise, and controlled cut of bony structures without causing destruction of soft tissue (including nerves, blood vessels, and oral mucosa) (Eggers, et al., 2004).

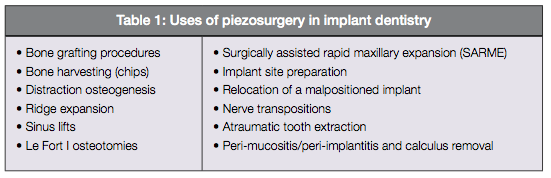
Since its introduction, piezosurgery has established an important role in various aspects of dentistry and dental implantology (Table 1). This article will discuss the role of piezosurgery in these areas, including its advantages and disadvantages.
Properties and characteristics
The piezosurgery unit provides three different power levels (endo, perio, and cortical/spongious), the highest of which is used in bone surgery. The amplitude of the working tip ranges from 60 to 200, mm/sec, with variable ultrasonic frequencies (Beziat, et al., 2007). A distinctive characteristic of piezosurgery is its ability to distinguish tissue hardness. It will act only on mineralized structures and, thus, will not cut or damage soft tissues. This occurs due to cessation of the surgical action when the scalpel comes into contact with demineralized structures (Robiony, et al., 2007).
Piezosurgery can be advantageous when exact cutting of thin bones is required. The modulated ultrasonic vibrations allow controlled cutting of bony structures. Delicate bony structures can be cut easily and with great precision. However, it is only of limited use in cutting highly dense bone and in regions with limited access (Eggers, et al., 2004). Because of its micrometric and selective cut, the piezosurgery unit produces safe and precise osteotomies without any osteonecrotic damage (Robiony, et al., 2004).
Due to its cavitational effect on physiological solutions such as blood, piezosurgery creates an effectively bloodless surgical site that makes visibility in the working area much clearer than with conventional bone-cutting instruments (González-García, 2007).
The digital modulation of the oscillation frequencies and the high-flow irrigation system of the piezosurgery unit minimizes overheating of the bone during osteotomies (Robiony, et al., 2007). Unlike conventional burs and micro saws, piezosurgery inserts do not become hot either, which again reduces the risk of postoperative necrosis and helps maintain vitality of adjacent tissue (Horton, et al., 1975).
In comparison with traditional rotary instrumentation, piezosurgery requires much less hand pressure. This leads to enhanced operator sensitivity and control, allowing the clinician to develop a better “feel” and precision for the cutting action because of the microvibration of the cutting tip (Seshan, et al., 2009).
Osseous response
Microscopic examination of bone fragments acquired during piezosurgery (Figure 1) have shown viable cells on the bony surfaces with no signs of coagulative necrosis (Robiony, et al., 2007). Research has shown a more favorable osseous response, with less bone damage when compared with diamond or carbide burs (Vercellotti, et al., 2005). A study by Preti, et al. (2007), concluded that piezoelectric bone surgery is more effective in stimulating implant osteogenesis, promoting more osteoblastic activity around the implant sites compared to sites prepared conventionally with drills.
Another study comparing piezosurgery with carbide and diamond burs to cut experimental osteotomies showed conventionally treated surgical sites lost bone level by day 14, compared to those treated by piezosurgery — which actually gained bone level. The study concluded that piezosurgery provides more favorable osseous repair and remodelling compared to burs when surgical ostectomy and osteoplasty procedures were performed (Landes, et al., 2008).
A study examined the recovery process of dogs that had gone through osteotomies with various techniques. In this study, the clinical and histological aspects of three surgery techniques — scalpel, piezosurgery, and low-speed bur — were analyzed. The recovery process after scalpel and piezosurgery were similar. However, a difference was observed in the recovery of bone tissue treated by a bur, as it produced degeneration of cellular elements along the edges, persistence of fibrovascular tissue, and a reduced reaction of osteoblasts and osteoclasts (Sortino, et al., 2008).
Healing
By applying the same surgery protocol and measurement methods, the study also compared rotary and piezosurgery with regards to time taken to complete surgery and postoperative healing. The average time of surgery was 25.83% higher in the piezosurgery group compared with rotary. The facial swelling and trismus at 24 hours post surgery with piezosurgery were respectively 40.06% and 25.3% lower compared with rotatory osteotomy technique. The results of the comparative study showed that piezo-surgery reduces the postoperative facial swelling and trismus, although increases the time of surgery (Sortino, et al., 2008).

Disadvantages
One key disadvantage of piezosurgery is the time involved: The piezoelectric scalpel requires repeated application to the bone to progressively deepen the cut and complete the osteotomy.
This increased preparation time inevitably carries financial implications, so slightly higher costs may be involved.
Piezosurgery usage in areas of highly dense cortical bone may have limited cutting strength and may not function as effectively as burs, and thus may not be suitable for all implant site preparations.
Bone grafting
There is a range of techniques available to manage deficient alveolar ridges. These include:
- Block bone grafting
- Guided bone regeneration
- Distraction osteogenesis
- Ridge expansion
Block bone grafting
The correct positioning of implants, in accordance with prosthodontic and functional principles, can be compromised by bone volume or density. The aim of augmentation is to reconstitute the original hard tissue contours as far as possible (Gellrich, et al., 2007). Atrophic alveolar ridges should be restored by bone augmentation so as to allow optimal implant positioning within the prosthetic envelope (Muñoz-Guerra, et al., 2009).
Various resources for bone grafting exist, including the use of allografts, xenografts, and alloplastic materials. However, autologous bone is still regarded as the gold standard with respect to intended bone quantity, quality, and an uneventful healing phase with reliable outcome (Gellrich, et al., 2007). Piezosurgery can be used effectively in autogenous block bone grafting procedures.
Autogenous grafts can be harvested from both intra- and extraoral sites. The most common intraoral sites include the mandibular ramus and symphysis, where delicate structures exist. One of the most significant advantages of piezosurgery over conventional burs and saws is its selective cut. This means that bone can be cut with relative ease while soft tissue, including nerves, blood vessels, and mucosal tissues, remain unharmed, even if they come into direct contact with the cutting tip (Stübinger, et al., 2006).
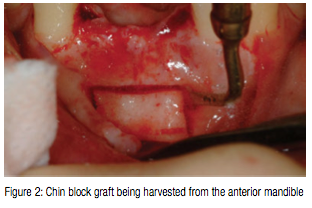
In comparison with surgical burs and microsaws, piezosurgery requires only a feather-light touch, allowing better operator sensitivity and control. As a result, the clinician develops a better feel and precision for the cutting action, can feel the transition from cortical to cancellous bone, and produces precise and clean cuts up to one centimeter deep. Consequently, the operator minimizes trauma and waste to the adjacent bone, creating grafts of optimum dimensions. Figure 2 demonstrates a chin block graft being harvested from the anterior mandible. Because piezosurgery does not traumatize the bone, it prevents the considerable bone necrosis often caused by surgical burs and microsaws (Vercellotti and Pollack, 2006). Histological research has shown a clear lack of postoperative cellular damage to the resection edges, bony matrix, or bone marrow.
There is also evidence of the presence of vital osteoblasts near the cut section of bone — meaning that bone cut with piezosurgery stays vital, and any bone chips that are harvested will contain vital osteoblasts as well as bone matrix, which, in turn, will increase healing rate.
In addition, less periosteal stripping occurs when using piezosurgery, so there is subsequently less postoperative pain and swelling, and wound healing is improved (Landes, et al., 2008). The risk of post-
operative necrosis is further reduced because piezosurgery inserts do not get hot (Vercellotti and Pollack, 2006). The overall patient experience may be less traumatic, with reduced donor and recipient site morbidity — and fewer complaints about vibration compared to with conventional burs and microsaws.
Guided bone regeneration
Piezosurgery is also very useful for harvesting bone chips, which are produced at the optimum grain size for effectiveness and remain on the bone surface ready for collection. Two surgical tips are available for removal of cortical bone, eliminating the need for bone traps. These bone chips can be used alone or in combination with other graft material for guided bone regeneration purposes. Landes, et al. (2008), assessed bone chips collected using piezosurgery and conventional burs and found no difference in the detrimental effect on the viability and differentiation of cells, but found piezosurgery was more economical in regard to quantity of bone harvested.
Distraction osteogenesis
Distraction osteogenesis is a method of regaining both hard and soft tissue without grafting. It is the biological process of new bone formation through the application of graduated tensile stress by incremental traction. With ridges that require four to five millimeters of vertical height augmentation, or where the overlying soft tissue does not support osseous augmentation, distraction osteogenesis is a useful treatment alternative, with piezosurgery being an effective tool for distraction osteotomies (Lee, et al., 2007).
When performing distraction osteo-genesis in certain areas, it is critical to complete the osteotomies delicately, because they are performed close to dental and periodontal structures, and to soft tissues that provide vascularization. The advantage is that we can osteotomize as precisely as possible due to its micrometric and linear vibrations, and cause minimal damage to hard and soft tissues (Vercellotti, 2000).
The use of piezosurgery can permit ideal osteotomy preparation without flap damage, providing abundant vascularization that leads to successful new bone formation. Furthermore, it is possible to get direct visibility over entire osteotomies. The only minor limitation is the slightly longer time required for the operation.
Ridge expansion
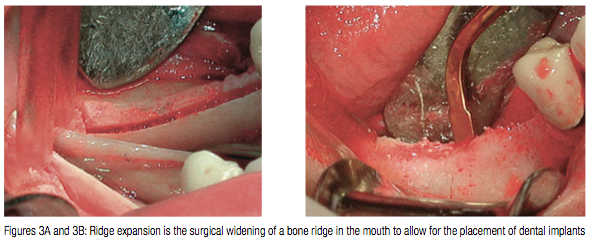
Ridge expansion is the surgical widening of a bone ridge in the mouth to allow for the placement of dental implants (Figure 3). It can allow for a shortened treatment time and eliminates the issue of donor-site morbidity, as grafting is not required. Piezosurgery was originally designed for augmentation in implant surgery, including sinus lifts and procedures such as ridge expansion (Eggers, et al., 2004). It can be used to cut the crestal and proximal facial cortices in a precise and tactile controlled manner. Motorized osteotomes are then used to widen the split ridge and create space. This technique allows for the expansion of narrow, anatomically limiting, atrophic ridges, creating space for immediate placement of implants. The facial and lingual cortices provide necessary support with vital osteocytes for osteogenesis (Kelly and Flanagan, 2013).

Sinus lifts
Atrophy of the maxilla and progressive pneumatization of the maxillary sinus can compromise implant placement in the posterior maxilla. Atrophy can lead to inadequate height, width, and quality of bone restricting ideal implant positioning and risking perforation of the sinus floor (Muñoz-Guerra, et al., 2009). There can often be as little as a few millimeters of bone between sinus and the oral cavity.
Piezosurgery can be used as an alternative or adjunct to standard instrumentation during a sinus lift procedure (Figure 4). The sinus is accessed through a window prepared in the lateral wall of the sinus, conventionally made using a diamond bur and then infracturing of the bony window.
However, a round piezosurgery tip may be used to prepare the window instead, which brings the advantage of being able to touch the sinus lining without tearing it. This eliminates the need to leave a thin layer of bone around the window and tap it in (and thus further reduces the chance of perforation).
A blunt inverted cone tip can then be used to raise the sinus lining, reducing the risk of damage to the membrane even further. In cases of sinus lift, studies have shown it can reduce the membrane perforation rate from 30% with the conventional approach to 7% with the piezosurgery (Wallace, et al., 2007).
Le Fort I osteotomies
In severely atrophic alveolar ridges, both the maxilla and mandible can present a jaw discrepancy, with a skeletal Class III tendency and a loss of vertical dimension that may hinder treatment with dental implants (Muñoz-Guerra, et al., 2009). Severe atrophy of the edentulous maxilla can cause insufficient bone volume and an unfavorable vertical, transverse, and sagittal relationship, due to the tri-dimensional resorption pattern of long-term maxillary edentulism (Muñoz-Guerra, et al., 2009).
Maxillary sinus augmentation and onlay grafting procedures can allow the correction of bone defects, but are often insufficient to correct severe maxillary retrusion and increased interarch distance. Le Fort I osteotomies allow for forward or downward repositioning of the maxilla to correct intermaxillary vertical and transverse discrepancies (Bell, et al., 1977). Correction of osseous deficiencies using this technique permits ideal implant placement and creates a more natural soft tissue profile that impacts on the overall prosthodontic outcome.
The precise nature of piezosurgery provides exact, clean, and smooth cut geometries (Stübinger, et al., 2005). This is an extremely important attribute, considering an atrophic maxilla is likely to present with a thin and fragile bone structure that may increase the risk of accidental fracture.
The application of piezosurgery in these instances is advocated over other mechanical instruments because it minimizes the chances of accidental damage (Muñoz-Guerra, et al., 2009). The risk to critical anatomical structures, such as the palatine nerve and artery, is also minimized because the surgical action stops when the piezosurgery insert comes into contact with demineralized structures (Robiony, et al., 2007).
However, it must be noted that the success rate of implants placed in a reconstructed maxillae following a Le Fort I technique and bone grafting is significantly lower than that of implants placed in an edentulous, but non-reconstructed, maxillae (Chiapasco, et al., 2007). Piezosurgery has also been used in various other craniofacial surgical procedures in addition to Le Fort osteotomies, including calvarian bone grafting and mandibular sagittal splits (Beziat, et al., 2007).
Surgically assisted rapid maxillary expansion
Surgically assisted rapid maxillary expansion (SARME) is another well-established procedure to correct maxillary transverse discrepancies. Piezosurgery can be used to carry out the surgical aspect of this technique and carries the same surgical advantages as those mentioned previously within this article.

Implant site preparation
Piezosurgery is efficient at preparing implant site osteotomies due to its selective cut, micro-streaming, and cavitational effects, which preserve and maintain the soft tissue — essential for the overall healing and esthetics of the implant (Sortino, et al., 2008).
Micro-streaming is the continuous whirling movement of fluid created by a vibrating insert that favors a mechanical action of debris removal. Intraoperative visibility is enhanced with piezosurgery by the implosion of gas bullae into blood vessels during the osteotomy, which have a hemostatic effect — the cavitational phenomenon (Sortino, et al., 2008).
Primary implant stability and osseo-integration are directly indicative of implant prognosis. Primary implant stability can provide an early indication of future osseointegration. A recent study by Baker, et al. (2012), has suggested that there are no statistically significant differences between primary implant stability provided by using the piezosurgery in comparison with a conventional rotary unit. However, due to the study being ex vivo in nature and the relatively small sample size, further studies are recommended.
In a minipig model, bone healing at intervals of 1, 2, 4, and 8 weeks in sites prepared with piezosurgery was compared to sites prepared with conventional drills. The study (Preti, et al., 2007) concluded that piezosurgery was more effective in stimulating implant osteogenesis, promoting more osteoblastic activity around the implant sites compared to sites prepared conventionally with drills.
Another randomized control trial suggested that piezosurgery implant site preparation has the potential to modify biological events during the osseo-integration process, resulting in a limited decrease of implant stability quotient values and in an earlier shifting from a decreasing to an increasing stability pattern in comparison with traditional drilling technique (Stacchi, et al., 2013).
Relocation of malpositioned implants
Implant relocation (Figure 5) is a relatively new surgical technique used to move integrated implants along with their surrounding bone into a more desired position. Inadequately positioned implants can either be left as “sleeper” implants, if their support is not essential for rehabilitation, or surgically removed and then replaced. The disadvantage of surgically removing the implant is that bony defects may be created, which compromise the ideal placement of another implant.
Another option is to surgically remove the implant with its surrounding bone into a more appropriate position. This peri-implant osteotomy can be accomplished by using conventional burs, saws, or piezosurgery (Stacchi, et al., 2008).
The advantage of using piezosurgery for this procedure is that maximum intraoperative control can be maintained to ensure a precise cut and minimal bone ablation. In addition, the healing response is likely to be more favorable in comparison to cuts using burs or saws (Preti, et al., 2007).
Nerve transpositions
Piezosurgery can be used for nerve lateralization or transposition procedures. The precise and selective surgical cut of piezosurgery is extremely important when performing surgery close to nerves such as the inferior alveolar nerve. Eriksson, et al. (2006), reported that an interruption of the structures of a nerve would result in proliferation of axons, a patho-physiological cause of paresthesia and dysesthesia.
An in vitro study compared piezosurgery with conventional bur surgery for transposition of the inferior alveolar nerve to assess the effects on both soft and hard tissues. The study concluded that piezosurgery was more invasive to the bone than a conventional diamond bur, but the amount of injury was much lower than when using a conventional rotary bur (Metzger, et al., 2006).
Atraumatic tooth extraction
When an implant is to be placed into a socket or area where a tooth is to be extracted, it is imperative to ensure minimal trauma to the surrounding bone to maintain as much bone as possible for integration of the implant. Piezosurgical extraction consists of cutting the fibers of the periodontal ligament with vibrating tips of up to 10 mm in depth. The teeth can then be mobilized with an elevator. This method can be very useful with teeth that are ankylosed. Extractions performed in this way can be atraumatic, and render subsequent implant placement more predictable and easier compared to using burs (Blus and Szmukler-Moncler, 2010).
Peri-mucositis, peri-implantitis, and calculus removal
Piezosurgery can be used in the treatment of peri-implantitis. It can be used for soft tissue debridement to remove the secondary flap after incision through retained periosteum. Using a thin tapered tip and altering the power setting, the piezo-surgery device can also be used to debride the field of residual soft tissue and for root surface scaling to ensure thorough removal of calculus. The piezosurgery system also allows removal of calculus from titanium osteosynthetic material quickly. Debris and infected bone can be removed from implant surfaces without damaging the implant. This feature can also be beneficial when hard tissue has ingrown into screw slots, as it allows safe removal without damaging the screw itself to allow for screwdriver application (Robiony, et al., 2007).
Conclusion
Before the widespread use of piezo-surgery for osteotomies is accepted, possible side effects such as thrombogenesis or impaired blood circulation need to be examined. An area of particular concern is the poorly vascularized mandible, where thrombosis of its intraosseous vessels may lead to obvious clinical problems of reossification of the osteotomy gap (Landes, et al., 2008).
Long-term follow-up in larger patient numbers will prove whether seldom, yet serious, complications such as hemorrhage, aseptic necrosis, and facial nerve palsy may occur with smaller incidence compared with conventional techniques (Landes, et al., 2008). As this article demonstrates, however, there is an important role for piezosurgery in various clinical scenarios within dental implant treatment. Piezosurgery can benefit the operator by allowing clear-cut precise osteotomies to be performed in a clear bloodless field without the risk of damaging soft tissues and nerves. The use of piezosurgery can equally benefit the patient by reducing postoperative swelling and trismus and speed up the recovery process. In addition, the lack of osteonecrosis caused by piezosurgery and the positive effects on bone healing and osteogenesis mean that piezosurgery is a valuable tool to have within your dental implant armamentarium.
References
- Baker JA, Vora S, Bairam L, Kim HI, Davis EL, Andreana S. Piezoelectric vs. conventional implant site preparation: ex vivo implant primary stability. Clin Oral Implants Res. 2012;23(4):433-437.
- Bell WH, Buche WA, Kennedy JW III, Ampil JP. Surgical correction of the atrophic alveolar ridge. A preliminary report on a new concept of treatment. Oral Surg Oral Med Oral Pathol. 1977;43(4):485-498.
- Beziat JL, Vercellotti T, Gleizal A. What is piezosurgery? Two years experience in craniomaxillofacial surgery. Rev Stomatol Chir Maxillofac. 2007;108(2):101-107.
- Blus C, Szmukler-Moncler S. Atraumatic tooth extraction and immediate implant placement with Piezosurgery: evaluation of 40 sites after at least 1 year of loading. Int J Periodontics Restorative Dent. 2010;30(4):355-363.
- Chiapasco M, Brusati R, Ronchi P. Le Fort I osteotomy with interpositional bone grafts and delayed oral implants for the rehabilitation of extremely atrophied maxillae: A 1-9-year clinical follow-up study on humans. Clin Oral Implants Res. 2007;18(1):74-85.
- Eggers G, Klein J, Blank J, Hassfeld S. Piezosurgery: an ultrasound device for cutting bone and its use and limitations in maxillofacial surgery. Br J Oral Maxillofac Surg. 2004;42(5):451-453.
- Eriksson L, Hillerup S, Reibel J, Persson S, Brun A. Traumatic changes of the inferior alveolar nerve and Gasserian ganglion after removal of a mandibular third molar: report of a case. J Oral Maxillofac Surg. 2006;64:(12)1821-1825.
- Gellrich NC, Held U, Schoen R, Pailing T, Schramm A, Bormann KH. Alveolar zygomatic buttress: A new donor site for limited preimplant augmentation procedures. J Oral Maxillofac Surg. 2007;65(2):275-280.
- González-García A, Diniz-Freitas M, Somoza-Martín M, García-García A. Piezoelectric bone surgery applied in alveolar distraction osteogenesis: a technical note. Int J Oral Maxillofac Implants. 2007;22(6):1012-1016.
- Horton JE, Tarpley TM Jr, Wood LD. The healing of surgical defects in alveolar bone produced with ultrasonic instrumentation, chisel, and rotary bur. Oral Surg Oral Med Oral Pathol. 1975;39(4):536-546.
- Kelly A, Flanagan D. Ridge expansion and immediate placement with piezosurgery and screw expanders in atrophic maxillary sites: two case reports. J Oral Implantol. 2013;39(1):85-90.
- Landes CA, Stübinger S, Rieger J, Williger B, Ha TK, Sader R. Critical evaluation of piezoelectric osteotomy in orthognathic surgery: operative technique, blood loss, time requirement, nerve and vessel integrity. J Oral Maxillofac Surg. 2008;66(4):657-674.
- Lee HJ, Ahn MR, Sohn DS. Piezoelectric distraction osteogenesis in the atrophic maxillary anterior area: a case report. Implant Dent. 2007;16(3):227-234.
- Metzger MC, Bormann KH, Schoen R, Gellrich NC, Schmelzeisen R. Inferior alveolar nerve transposition — an in vitro comparison between piezosurgery and conventional bur use. J Oral Implantol. 2006;32(1):19-25.
- Muñoz-Guerra MF, Naval-Gías L, Capote-Moreno A. Le Fort I osteotomy, bilateral sinus lift, and inlay bone-grafting for reconstruction in the severely atrophic maxilla: a new vision of the sandwich technique, using bone scrapers and piezosurgery. J oral Maxillofac Surg. 2009;67(3):613-618.
- Preti G, Martinasso G, Peirone B, Navone R, Manzella C, Muzio G, Russo C, Canuto RA, Schierano G. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007;78(4): 716-722.
- Robiony M, Polini F, Costa F, Zerman N, Politi M. Ultrasound bone cutting for surgically assisted rapid maxillary expansion (SARME) under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(3):266-269.
- Robiony M, Polini F, Costa F, Vercellotti T, Politi M. Piezoelectric bone cutting in multipiece maxillary osteotomies. Technical note. J Oral Maxillofac Surg. 2004;62(6):759-761.
- Seshan H, Konuganti K, Zope S. Piezosurgery in periodontology and oral implantology. J Indian Soc Periodontol. 2009;13(3): 155-156.
- Sortino F, Pedullà E, Masoli V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: comparison of postoperative recovery. J Oral Maxillofac Surg. 2008;66(12):2444-2448.
- Stacchi C, Costantinides F, Biasotto M, Di Lenarda R. Relocation of a malpositioned maxillary implant with piezoelectric osteotomies: a case report. Int J Periodontics Restorative Dent. 2008;28(5):489-495.
- Stacchi C, Vercellotti T, Torelli L, Furlan F, Di Lenarda R. Changes in implant stability using different site preparation techniques: twist drills versus piezosurgery. a single-blinded, randomized, controlled clinical trial. Clin Implant Dent Relat Res 15(2):188-197
- Stübinger S, Kuttenberger J, Filippi A, Sader R, Zeilhofer HF. Intraoral piezosurgery: preliminary results of a new technique. J Oral Maxillofac Surg. 2005;63(9):1283-1287.
- Stübinger S, Robertson A, Zimmerer KS, Leiggener C, Sader R, Kunz C. Piezoelectric harvesting of an autogenous bone graft from the zygomaticomaxillary region: case report. Int J Periodontics Restorative Dent. 2006;26(5):453-457.
- Vercellotti T. Piezoelectric surgery in implantology: a case report — a new piezoelectric ridge expansion technique. Int J Periodontics Restorative Dent. 2000;20(4):358-365.
- Vercellotti T, Nevins ML, Kim DM, Nevins M, Wada K, Schenk RK, Fiorellini JP. Osseous response following resective therapy with piezosurgery. Int J Periodontic Restorative Dent. 2005;25(6):543-549.
- Vercellotti T, Pollack AS. A new bone surgery device: sinus grafting and periodontal surgery. Compend Contin Educ Dent. 2006;27(5):319-325.
- Wallace SS, Mazor Z, Froum SJ, Cho SC, Tarnow DP. Schneiderian membrane perforation rate during sinus elevation using piezosurgery: clinical results of 100 consecutive cases. Int J Periodont Rest Dent. 2007;27(5):413-419.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores


