Educational aims and objectives
This self-instructional course for dentists aims to discuss survival rates for pterygoid dental implants in immediately loaded fixed-arch protocols.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize how to overcome some shortcomings of the posterior maxilla for implant placement.
- Be informed about a study where a total of 1,058 pterygoid dental implants were placed in 563 patients.
- Identify the pterygomaxillary complex and possible ways to maximize implant placement in that area.
- Realize survival rates and other pertinent data for dental implants placed in pterygoid region for full-arch immediately loaded procedures.
- Identify some history of pterygoid
- Realize some unique implant insertion angles for this technique.
Dr. Dan Holtzclaw and colleagues take a look at survival rates of pterygoid implants in immediately loaded full-arch protocols.
Drs. Dan Holtzclaw, Juan Gonzalez, Aldo Espinosa, Sam Sauza, Raouf Hanna, Peyman Raissi, Chris Epperson, Cory Ryan, Nirjal Patel, Amel Hassan, Peter Fereg, Jumoke Adedoyin, and Dan Fenton report on survival rates and other pertinent data
Abstract
Background
While contemporary root-form implants have been used in the pterygomaxillary region for over 30 years, few studies have evaluated immediate-loading protocols for these fixtures. The current study reports on the use of pterygoid implants in full arch immediate load protocols over an 8-year period.
Methods
A retrospective chart review was performed for all patients treated with immediately loaded fixed-arch protocols that involved pterygoid dental implants. Qualifying patients had data collected for age, sex, insertion torque, implant diameter, and length. Cone beam computed tomography scans were analyzed to confirm implant engagement into the pterygoid region, and CBCT angle measurement tools were used to determine both the anteroposterior and mediolateral inclinations of dental implants relative to the occlusal plane. All pterygoid implants in this study were loaded within 4 hours of placement using screw-retained transitional restorations. Definitive restorations were delivered an average of 8 months after implant placement and were followed annually at yearly maintenance appointments.
Results
A total of 1,058 pterygoid dental implants were placed in 563 patients with a mean survival rate of 98.02%. Mean follow-up time was 24.51 months (range 6-94 months). The mean anteroposterior implant insertion angle relative to the occlusal plane was 66.94 ± 8.82° while the mean mediolateral implant insertion angle relative to the occlusal plane was 57.66 ± 10.31°. Mean insertion torque value for pterygoid implants placed in this study was 50.38 ± 13.30 Ncm.
Conclusion
Pterygoid dental implants can achieve high survival rates in immediately loaded fixed-arch protocols with proper angulation placement.
Introduction
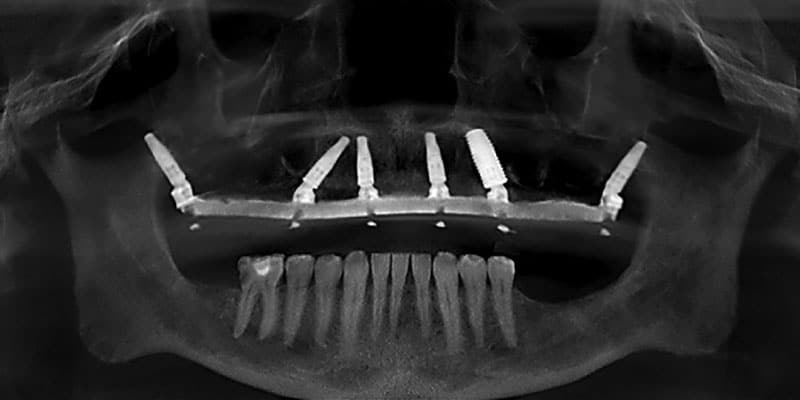
The posterior maxilla presents numerous challenges for dental implant treatment. When edentulous, pneumatization of the maxillary sinus reduces the amount of available bone for implant placement (Figure 1).1,2 When dentate, immediate implant placement following maxillary molar extraction is complicated by large diameter residual sockets, variable quantities of interradicular bone, and sinus floor proximity.3 Additionally, bone in the posterior maxilla is of poor density and provides minimal cortical anchorage for dental implant stability.4-6 To overcome these shortcomings of the posterior maxilla for implant placement, a number of ancillary techniques have been employed including lateral window sinus lifts,7,8 crestal sinus lifts,9,10 bone condensation,11 short length-wide diameter dental implants,12 and offset placement of implants into the palatal root socket.13 Many of these procedures result in additional appointments, extended healing periods, supplementary expense, and increased patient morbidity.14

For full-arch immediate implant loading, the unique anatomic features of the posterior maxilla have influenced procedure designs. In the traditional All-On-4® full-arch immediate-loading protocol, the distal implants are angled up to 45° anteriorly in an effort to avoid the maxillary sinus, increase anterior-posterior (AP) spread, and anchor into the denser bone of the mid-maxilla versus the softer bone of the posterior maxilla (Figure 2).15-18 Occasionally, extensive pneumatization of the maxillary sinus results in anterior migration of the mesial sinus wall which can negatively affect placement of the angled implant for this procedure.1,2 In such situations, anterior placement of the distal angled implant leaves the undesirable choice of either a truncated restoration that may result in functional and esthetic issues, or an excessively long cantilevered restoration that may produce increased forces on the distal implant.19 For the experienced dental implant surgeon, the “pterygoid” dental implant affords an opportunity to overcome the shortcomings of the posterior maxilla while still allowing for immediate loading in most cases (Figure 3). Use of the pterygoid region for dental implant treatment dates to the 1970s with subperiosteal techniques and the 1980s with more contemporary root-form fixtures.20-24 Although pterygoid implants have been reported in dental literature for nearly 50 years, very few studies have evaluated the use of these implants for immediately loaded full-arch procedures. Accordingly, the aim of this study is to report on survival rates and other pertinent data for dental implants placed in the pterygoid region for full-arch immediately loaded procedures.
Materials and methods
A retrospective chart review was performed in the offices of the authors for all patients treated with immediately loaded dental implants that were placed into the pterygoid region. To qualify as a “pterygoid” implant, fixtures were required to engage the pyramidal process of the palatine bone and/or the pterygoid lamellae of the sphenoid bone. Cone beam computed tomography (CBCT) scans were analyzed to confirm implant engagement into the pterygoid region, and CBCT angle measurement tools were used to determine both the anteroposterior and mediolateral inclinations of dental implants relative to the occlusal plane. Implant survival was defined according to criteria defined by Malo, et al.28 Basic data such as patient age, sex, implant diameter, and implant length were obtained from chart review. All pterygoid implants in this study were loaded within 4 hours of placement using screw-retained transitional restorations. Definitive restorations were delivered an average of 8 months after implant placement and were followed annually at yearly maintenance appointments.

Results
A total of 1,058 pterygoid dental implants placed in 563 patients qualified as pterygoid implants for the purposes of this study. 306 patients were female and 257 were male with a mean age of 62.78 ± 12.04 years (range 31-92 years). Bilateral pterygoid implants were placed into 495 patients while 68 patients had pterygoid implants placed unilaterally. After a minimum follow-up time of 6 months and maximum time of 94 months (mean 24.51 months), 21 pterygoid implant failures were noted producing a survival rate of 98.02%. Complications were minimal and included the following: minor hemorrhaging during osteotomy creation, post-surgical trismus in 7 patients, and 1 patient could not tolerate the prosthesis extending back to the pterygoid implant. The mean anteroposterior implant insertion angle relative to the occlusal plane was 66.94 ± 8.82° (Figure 4), while the mean mediolateral implant insertion angle relative to the occlusal plane was 57.66 ± 10.31° (Figure 5). Mean insertion torque value for pterygoid implants placed in this study was 50.38 ± 13.30 Ncm (Figure 6).

Discussion
Full arch immediately loaded dental implants have become a proven treatment modality over the past 20 years following the introduction of the “All-On-4®” concept by Malo in 2003.15,16,18,25-30 This treatment concept involves restoring an arch with at least four dental implants, the distal of which are tilted up to 45 degrees, and immediately loading the transitional prosthesis.15 In the maxilla specifically, angling the distal implants affords the benefit of avoiding the maxillary sinus and obviating the need for additional procedures such as sinus augmentation.27-29 As the anterior wall of the maxillary sinus determines the position of the distal angulated implant in All-On-4® style procedures, challenges can arise with extensive sinus pneumatization where the anterior wall of the maxillary sinus has migrated anteriorly. Studies by Khojastepour and Zhang show that the anterior wall of the maxillary sinus terminates at the first premolar or anteriorly in 93.67 – 98.60% of patients.57,58 Such situations restrict placement of the distal implant creating limitations on the A-P spread between implants. The restoring clinician is then faced with the prosthetic dilemma of excessive cantilever length that may compromise implant stability or prosthetic truncation which may create both functional and esthetic compromises for the patient.19 In such situations, use of pterygoid dental implants can help.14,19,31
In the 1970s, Linkow and others regularly employed the pterygoid region to provide support for full-arch subperiosteal implant restorations.20-24 Tulasne32 is generally credited as the first to describe use of root form dental implants in the pterygomaxillary complex with recommendations that “pterygoid” implants should cross the maxillary tuberosity to reach the dense cortical bone of the pterygomaxillary plate allowing sufficient anchorage in the posterior maxilla in the absence of grafting materials.33 Early use of root-form machined surface dental implants in the pterygoid region during the late 1980s and 1990s achieved success rates of 86.3 – 89%.34-36 Pterygoid implant studies over the next 20 years attained improved success rates as they employed roughened surface treatments as opposed to the smooth surfaced implants of older studies, and new techniques were developed for their placement.14,37-42
Until recently, nearly all published pterygoid implant studies have focused on delayed loading techniques.14,43,44 Although some studies have reported isolated use of pterygoid implants for immediate loading,19,31,59 few studies have exclusively evaluated this technique in sufficient numbers to determine any definitive conclusions. The implant success rate of 98.02% reported in the present study of immediately loaded pterygoid dental implants is similar to the reported success rates of previously published pterygoid implant studies that employed delayed loading protocols.14,37-43 Reports of implant failures in previously published pterygoid implant studies typically occurred prior to prosthetic attachment during the unloaded healing phase.14,43,44 As these implants were not loaded and submerged during healing, failure to osseointegrate was likely due to misaligned insertion angles that caused inadequate engagement of the dental implant into the dense bone of the pterygomaxillary complex. Vrielinck, et al.,45 confirmed as much when they reported most pterygoid implant failures in their study were due to “the apical part of the implant deviating in a more lateral position” to the initially intended drilling target of the pterygomaxillary bony complex. In the present study, all implant failures had similar findings to those of Vrielinck, et al.,45 with failed implants having excessive lateral or anterior placement relative to their intended target (Figure 7).

Anteroposterior implant insertion angles in the present study are similar to those of previously published studies. The 66.94º mean anteroposterior insertion angle of the current study falls between the 52.3º anterior insertion angle and 75.1º posterior insertion angle reported by Uchida, et al., in a computed tomography cadaveric study of potential pterygomaxillary implant insertion angles.46 A 2016 study by Rodriguez, et al., evaluating virtual planning of pterygoid implant insertion angles using CBCT scans had similar findings with a mean anteroposterior insertion angle of 74.19 degrees.47 In a 2014 study employing similar virtual planning methods, Rodriguez, et al., reported an average anteroposterior insertion angle of 72.5º and an average mediolateral angulation of 81.3º.48 The 57.66º mean mediolateral insertion angle of the current study is nearly 24 more medial to those reported by Rodriguez, et al., in their 2014 virtual planning study.48 The few studies that have analyzed the pterygoid implant failures cite excessive lateral implant insertion angles relative to the pterygomaxillary complex.14,45 Analyzed mediolateral relative to the occlusal plane, these “excessive lateral insertion angles” translate to an implant position that is too buccal with the implant essentially deflecting off the side of the pterygomaxillary complex. By angling an average of 24° more medial than the 2014 Rodriguez publication, the authors of the current study felt that they were able to engage the pyramidal process more consistently. The high mean insertion torque values reported in this study were likely a result of consistent engagement of the pyramidal process with this more medial angulation. Failure to engage the pterygomaxillary complex with pterygoid implants can result in severe complications. A 2013 case report by Nocini49 described displacement of a dental implant into the infratemporal fossa during computer guided placement of a pterygoid implant. Another study utilizing computer designed drill guides for pterygoid implant placement reported mean apical insertion deviation of 7.77 mm (range 1.1 – 16.1 mm) and mean insertion angle deviation of 10.18º (range 1.7 – 18.0º).45 Implant insertion deviations of this magnitude not only have the potential to completely miss engagement of the pterygomaxillary complex resulting in increased chances of implant failure, they also increase the potential of damaging adjacent vascular structures such as the pterygoid venous plexus and maxillary artery.19

The pterygomaxillary complex is composed of three distinct bony structures: the low density maxillary tuberosity, the high density pyramidal process of the palatine bone, and the high density pterygoid processes of the sphenoid bone (Figure 8).50 The dense bone of the pterygomaxillary pillar where the sphenoid and palatine bones meet is where pterygoid implants gain the majority of implant insertion torque as CBCT analysis of this area shows bone density 139.2% higher than that of the maxillary tuberosity.47 Failure to engage the dense bone of the pyramidal and/or pterygoid processes may lead to lower implant insertion torque and a higher chance of failure.19,51-54 Average insertion torque for the pterygoid implants in this study was 50.38 Ncm. CBCT analysis showed that nearly all implants in this retrospective study actively engaged the dense bone of the pyramidal process which likely accounts for the high insertion torque and low failure rate of implants in this study. When appropriately placed, pterygoid implants can engage up to 8 mm of dense Type I bone in the pyramidal process and pterygoid pillar (Figure 9).60,61 A study of edentulous dry skulls evaluating anatomical measurements of the pyramidal process found an average height of 13.1 mm (range 8.3 mm – 21.4 mm), mean anteroposterior width of 6.5 mm (range 3.3 mm – 9.7 mm), and mean mediolateral width of 9.5 mm (range 4.2 mm – 11.8 mm).55 Based on these measurements for this intended target area of pterygoid implants and respect for adjacent vascular structures, implant diameter recommendations of 3.5 mm – 4.3 mm have been proposed in various studies of pterygoid dental implants.14,19,31,37,40,42,56 In the current study, utilized implant diameters were 3.5 mm, 3.75 mm, 4.2 mm, and 4.3 mm with the majority of implants being either 3.75 mm or 4.2 mm in diameter. Dental implant lengths in the current study ranged from 13 mm to 25 mm. These implant lengths are consistent with previously published pterygoid implant studies and other studies evaluating anatomic features of the pterygomaxillary complex relative to implant length.14,19,31,37,40,42,56 A recent systematic review and meta-analysis of pterygoid dental implants by Araujo, et al.,14 established a minimum implant length of 13 mm for fixtures to be considered pterygoid implants due to the fact that implants of at least this length or longer would be necessary to engage the dense bone of the pyramidal process. In a retrospective evaluation of 992 dental implants placed into the pterygoid region over a 28-year period, Balshi, et al., reported that longer implant lengths up to 18 mm had higher survival rates compared to shorter length implants, and these fixtures could be safely placed in this region without complication.37 Going even further in length, other studies have employed pterygoid implants with lengths up to 25 mm without complication.31,59 The results of the current study concur with these previous publications that implants up to 25 mm in length can be safely placed in the pterygoid region on a case by case basis.
For the experienced dental implant surgeon, the “pterygoid” dental implant affords an opportunity to overcome the shortcomings of the posterior maxilla while still allowing for immediate loading in most cases.
Conclusion
The present study demonstrates that immediately loaded dental implants engaging the pterygomaxillary complex have survival rates comparable to delayed-loading protocols for pterygoid implants in previously published studies. To adequately engage the target area containing dense bone in the pterygomaxillary pillar, it is important to know the anatomic features of this region and unique implant insertion angles for this technique.
Whether you are interested in pterygoid implants or less complex procedures, you can read some case studies from our experienced authors! https://implantpracticeus.com/category/case-studies/
References
- Tolstunov L, Thai D, Arellano L. Implant-guided volumetric analysis of edentulous maxillary bone with cone-beam computerized tomography scan. Maxillary sinus pneumatization classification. J Oral Implantol. 2012 Aug;38(4):377-90.
- Abdel-Wahed NA, Bahammam MA. Cone Beam CT-Based Preoperative Volumetric Estimation of Bone Graft Required for Lateral Window Sinus Augmentation, Compared with Intraoperative Findings: A Pilot Study. Open Dent J. 2018 Oct 25;12:820-826.
- Demircan S, Çankaya AB. Is immediate implant placement possible in the maxillary molar area? An anatomical study. Quintessence Int. 2016;47(10):853-859.
- Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991 Jan;62(1):2-4.
- Hao Y, Zhao W, Wang Y, Yu J, Zou D. Assessments of jaw bone density at implant sites using 3D cone-beam computed tomography. Eur Rev Med Pharmacol Sci. 2014;18(9):1398-1403.
- Goiato MC, dos Santos DM, Santiago JF Jr, Moreno A, Pellizzer EP. Longevity of dental implants in type IV bone: a systematic review. Int J Oral Maxillofac Surg. 2014 Sep;43(9):1108-1116.
- Testori T, Weinstein T, Taschieri S, Wallace SS. Risk factors in lateral window sinus elevation surgery. Periodontol 2000. 2019 Oct;81(1):91-123.
- Raghoebar GM, Onclin P, Boven GC, Vissink A, Meijer HJA. Long-term effectiveness of maxillary sinus floor augmentation: A systematic review and meta-analysis. J Clin Periodontol. 2019 Jun;46 Suppl 21:307-318.
- Summers RB. A new concept in maxillary implant surgery: the osteotome technique. 1994 Feb;15(2):152, 154-6, 158 passim; quiz 162.
- Attar BM, Alaei S, Badrian H, Davoudi A. Clinical and radiological evaluation of implants placed with osteotome sinus lift technique: 19-month follow-up. Ann Maxillofac Surg. 2016 Jul-Dec;6(2):190-194.
- Pai UY, Rodrigues SJ, Talreja KS, Mundathaje M. Osseodensification – A novel approach in implant dentistry. J Indian Prosthodont Soc. 2018 Jul-Sep;18(3):196-200.
- Hattingh A, De Bruyn H, Vandeweghe S. A retrospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin Implant Dent Relat Res. 2019 Oct;21(5):879-887.
- Wychowański P, Woliński J, Kacprzak M, Tomkiewicz W, Bartłomiej I, Szubińska-Lelonkiewicz D, Wojtowicz A, Nevins M. Immediate Palatal Molar Implants: A Simple, Safe, Minimally Invasive Technique. Int J Periodontics Restorative Dent. 2017 Nov/Dec;37(37):e297-e301.
- Araujo RZ, Santiago Júnior JF, Cardoso CL, Benites Condezo AF, Moreira Júnior R, Curi MM. Clinical outcomes of pterygoid implants: Systematic review and meta-analysis. J Craniomaxillofac Surg. 2019 Apr;47(4):651-660.
- Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2-9.
- Maló P, Araújo Nobre MD, Lopes A, Rodrigues R. Double Full-Arch Versus Single Full-Arch, Four Implant-Supported Rehabilitations: A Retrospective, 5-Year Cohort Study. J Prosthodont. 2015 Jun;24(4):263-270.
- Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000 May-Jun;15(3):405-414.
- Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. A retrospective analysis of 800 Brånemark System implants following the All-on-Four™ protocol. J Prosthodont. 2014 Feb;23(2):83-88.
- Holtzclaw D. Pterygoid Fixated Arch Stabilization Technique (PFAST): A Retrospective Study of Pterygoid Dental Implants used for Immediately Loaded Full Arch Prosthetics. J Implant Adv Clin Dent. 2018;10(7):6-15.
- Linkow LI. The pterygoid extension implant. J Miss Dent Assoc. 1972 Nov;28(4):10-19.
- Linkow LI. The pterygoid extension implant for the totally and partially edentulous maxillae. Int J Orthod. 1974 Sep;12(3):9-19.
- Linkow LI, Mahler MS. 3-Jahresbericht über Pterygoid-Extensions-implantate für den total und teilweise unbezahnten Oberkiefer [3-year report on pterygoid-extension-implants for totally and partially edentulous upper jaws]. Orale Implantol. 1975 Jul;2(3):19-29. German.
- Linkow LI, Mahler MS. Three year progress report on the pterygoid extension implant for the totally and partially, edentulous maxillae. Quintessence Int Dent Dig. 1976 Jan;7(1):9-17.
- Linkow LI. Bericht über die Weiterentwicklung der Pterygoidextensions-implantate für den ganz und teilweise unbezahnten Oberkiefer [Further development of the implant pterygoid-extension for the totally and partially edentulous upper jaw]. Orale Implantol. 1976 Jun;3(4):125-146. German.
- Butura CC, Galindo DF, Jensen OT. Mandibular all-on-four therapy using angled implants: a three-year clinical study of 857 implants in 219 jaws. Dent Clin North Am. 2011 Oct;55(4):795-811.
- Malo P, de Araújo Nobre M, Lopes A, Moss SM, Molina GJ. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011 Mar;142(3):310-320.
- Maló P, de Araújo Nobre M, Lopes A, Francischone C, Rigolizzo M. “All-on-4” immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin Implant Dent Relat Res. 2012 May;14 Suppl 1:e139-150
- Maló P, de Araújo Nobre M. Partial rehabilitation of the posterior edentulous maxilla using axial and tilted implants in immediate function to avoid bone grafting. Compend Contin Educ Dent. 2011 Nov-Dec;32(9):E136-145.
- Maló P, Nobre Md, Lopes A. The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5-year retrospective study and a new classification. Eur J Oral Implantol. 2011 Autumn;4(3):227-243.
- Malo P, Nobre Mde A, Lopes A. Immediate rehabilitation of completely edentulous arches with a four-implant prosthesis concept in difficult conditions: an open cohort study with a mean follow-up of 2 years. Int J Oral Maxillofac Implants. 2012 Sep-Oct;27(5):1177-1190.
- Nag PVR, Dhara V, Puppala S, Bhagwatkar T. Treatment of the Complete Edentulous Atrophic Maxilla: The Tall Tilted Pin Hole Placement Immediate Loading (TTPHIL)-ALL TILT™ Implant Option. J Contemp Dent Pract. 2019 Jun 1;20(6):754-763.
- Tulasne JF. Implant treatment of missing posterior dentition. In: Albrektson T, Zarb G, Editors. The Branemark Osseointegrated Implant. Chicago: Quintessence;1989:103-115.
- Tulasne JF. Osseointegrated fixtures in the pterygoid region. In: Worthington P, Branemark P, Editors. Advanced Osseointegration Surgery. Applications in the Maxillofacial Region, Chicago: Quintessence; 1992:182-188.
- Graves SL. The pterygoid plate implant: a solution for restoring the posterior maxilla. Int J Periodontics Restorative Dent. 1994 Dec;14(6):512-523.
- Balshi TJ, Wolfinger GJ, Balshi SF 2nd. Analysis of 356 pterygomaxillary implants in edentulous arches for fixed prosthesis anchorage. Int J Oral Maxillofac Implants. 1999 May-Jun;14(3):398-406.
- Balshi TJ, Lee HY, Hernandez RE. The use of pterygomaxillary implants in the partially edentulous patient: a preliminary report. Int J Oral Maxillofac Implants. 1995 Jan-Feb;10(1):89-98.
- Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. Brånemark system implant lengths in the pterygomaxillary region: a retrospective comparison. Implant Dent. 2013 Dec;22(6):610-612.
- Cucchi A, Vignudelli E, Franco S, Corinaldesi G. Minimally Invasive Approach Based on Pterygoid and Short Implants for Rehabilitation of an Extremely Atrophic Maxilla: Case Report. Implant Dent. 2017 Aug;26(4):639-644.
- Rodríguez X, Méndez V, Vela X, Segalà M. Modified surgical protocol for placing implants in the pterygomaxillary region: clinical and radiologic study of 454 implants. Int J Oral Maxillofac Implants. 2012 Nov-Dec;27(6):1547-1553.
- Peñarrocha M, Carrillo C, Boronat A, Peñarrocha M. Retrospective study of 68 implants placed in the pterygomaxillary region using drills and osteotomes. Int J Oral Maxillofac Implants. 2009 Jul-Aug;24(4):720-6.
- Valerón JF, Valerón PF. Long-term results in placement of screw-type implants in the pterygomaxillary-pyramidal region. Int J Oral Maxillofac Implants. 2007 Mar-Apr;22(2):195-200.
- Curi MM, Cardoso CL, Ribeiro Kde C. Retrospective study of pterygoid implants in the atrophic posterior maxilla: implant and prosthesis survival rates up to 3 years. Int J Oral Maxillofac Implants. 2015 Mar-Apr;30(2):378-383.
- Bidra AS, Huynh-Ba G. Implants in the pterygoid region: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011 Aug;40(8):773-781.
- Candel E, Peñarrocha D, Peñarrocha M. Rehabilitation of the atrophic posterior maxilla with pterygoid implants: a review. J Oral Implantol. 2012 Sep;38 Spec No:461-466
- Vrielinck L, Politis C, Schepers S, Pauwels M, Naert I. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int J Oral Maxillofac Surg. 2003 Feb;32(1):7-14.
- Uchida Y, Yamashita Y, Danjo A, Shibata K, Kuraoka A. Computed tomography and anatomical measurements of critical sites for endosseous implants in the pterygomaxillary region: a cadaveric study. Int J Oral Maxillofac Surg. 2017 Jun;46(6):798-804.
- Rodríguez X, Lucas-Taulé E, Elnayef B, Altuna P, Gargallo-Albiol J, Peñarrocha Diago M, Hernandez-Alfaro F. Anatomical and radiological approach to pterygoid implants: a cross-sectional study of 202 cone beam computed tomography examinations. Int J Oral Maxillofac Surg. 2016 May;45(5):636-640.
- Rodríguez X, Rambla F, De Marcos Lopez L, Méndez V, Vela X, Jiménez Garcia J. Anatomical study of the pterygomaxillary area for implant placement: cone beam computed tomographic scanning in 100 patients. Int J Oral Maxillofac Implants. 2014 Sep-Oct;29(5):1049-1052.
- Nocini PF, De Santis D, Morandini B, Procacci P. A dental implant in the infratemporal fossa: case report. Int J Oral Maxillofac Implants. 2013 Jul-Aug;28(4):e195-197.
- Reiser GM. Implant use in the tuberosity, pterygoid, and palatine region: Anatomic and surgical considerations. In: Nevins M, Mellonig JT, eds. Implant Therapy: Clinical Approaches and Evidence of Success. Chicago, IL:Quintessence;1998:197-207.
- Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD003878.
- Esposito M, Grusovin MG, Coulthard P, Worthington HV. Different loading strategies of dental implants: a Cochrane systematic review of randomised controlled clinical trials. Eur J Oral Implantol. 2008 Winter;1(4):259-276.
- Trisi P, Berardi D, Paolantonio M, Spoto G, D’Addona A, Perfetti G. Primary stability, insertion torque, and bone density of conical implants with internal hexagon: is there a relationship? J Craniofac Surg. 2013 May;24(3):841-844.
- Schnitman PA, Hwang JW. To immediately load, expose, or submerge in partial edentulism: a study of primary stability and treatment outcome. Int J Oral Maxillofac Implants. 2011 Jul-Aug;26(4):850-859.
- Lee SP, Paik KS, Kim MK. Anatomical study of the pyramidal process of the palatine bone in relation to implant placement in the posterior maxilla. J Oral Rehabil. 2001 Feb;28(2):125-132.
- Rodríguez X, Méndez V, Vela X, Segalà M. Modified surgical protocol for placing implants in the pterygomaxillary region: clinical and radiologic study of 454 implants. Int J Oral Maxillofac Implants. 2012 Nov-Dec;27(6):1547-1553.
- Khojastepour L, Movahhedian N, Zolghadrpour M, Mahjoori-Ghasrodashti M. Assessment of the relationship between the maxillary sinus and the canine root tip using cone beam computed tomography. BMC Oral Health. 2021 Jul 10;21(1):338.
- Zhang YQ, Yan XB, Meng Y, Zhao YN, Liu DG. Morphologic Analysis of Maxillary Sinus Floor and its Correlation to Molar Roots using Cone Beam Computed Tomography. Chin J Dent Res. 2019;22(1):29-36.
- Holtzclaw D. Pterygoid Fixated Arch Stabilization Technique (PFAST): A Retrospective Study of Pterygoid Dental Implants used for Immediately Loaded Full Arch Prosthetics. J Implant Adv Clin Dent 2018;10(7):6-17.
- Graves SL. The pterygoid plate implant: a solution for restoring the posterior maxilla. Int J Periodontics Restorative Dent. 1994 Dec;14(6):512-523.
- Bidra A, Balshi T, Wolfinger G. Use of Implants in the Pterygoid Region for Prosthodontic Treatment: American College of Prosthodontists Position Statement. Amer College Prosth 2017;1:1-4. https://www.prosthodontics.org/about-acp/position-statement-use-of-implants-in-the-pterygoid-region-for-prosthodontic-treatment-/. Accessed April 25, 2023.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores


