Educational aims and objectives
This self-instructional course for dentists aims to provide an overview of necessary practices to consider when prescribing and storing controlled substances.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Define key terms used when prescribing and storing controlled substances.
- List methods to minimize diversion and fraud of controlled substances.
- Outline federal requirements for storing controlled
- Identify specific records that must be readily retrievable should a dental practice be audited or investigated.
- List common violations of the Controlled Substance Act by dental practitioners.
Tyler Dougherty, PharmD; Michael O’Neil, PharmD; and Nikki Sowards, PharmD; offer important information regarding controlled substance record keeping in the dental practice.
 Tyler Dougherty, PharmD; Michael O’Neil, PharmD; and Nikki Sowards, PharmD; review key considerations when prescribing and storing controlled substances
Tyler Dougherty, PharmD; Michael O’Neil, PharmD; and Nikki Sowards, PharmD; review key considerations when prescribing and storing controlled substances
Introduction
Prescription medication misuse, substance use disorder (SUD), and diversion continue to remain problematic across the United States. Dental practitioners are often targeted by patients since they are a potential source of potent prescription opioids. Additionally, dental practitioners are subject to investigations by the Drug Enforcement Agency (DEA) as part of routine inspections or for potential violations of the Federal Controlled Substance Act (CSA).1 Dental practitioner prescribing and office management of controlled substances require vigilance, careful scrutiny of all records, and well-organized record keeping of both patient medical records and controlled substance records. This article will review key considerations when prescribing and storing controlled substances.
Definitions
Understanding of medical and legal terminology surrounding controlled substances is important when interpreting the medical/legal literature, and when trying to maintain compliance with state and federal statutes and regulations. The following terminologies provide guidance regarding safe and effective controlled substance management and prescribing practices.
Prescription Medication Misuse
Prescription medication misuse may be defined as taking a prescription medication outside of the boundaries of the initial prescription’s “intent for use” or directions. This may include a different diagnosis, taking the medication in larger doses or more often than prescribed, or to significantly alter/enhance one’s mental status.2
Substance Use Disorder (SUD)
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), no longer uses the terms substance abuse and substance dependence. Rather, it refers to substance use disorders, which are classified as mild, moderate, or severe. The level of severity is determined by the number of diagnostic criteria met by an individual.”3
Prescription Medication Diversion
The movement of a prescription medication in any direction other than how legally allowed to be transferred by law.4
Prescription Drug Monitoring Program (PDMP)
Prescription Drug Monitoring Programs are state-regulated electronic databases that store outpatient dispensing records for specific controlled substances.5
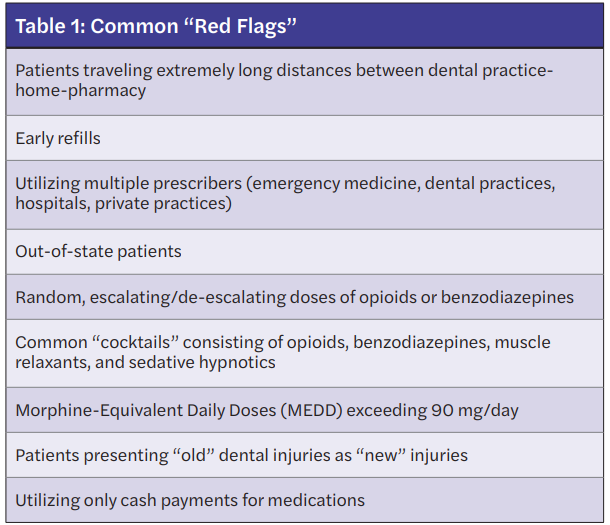
Red Flags
Red flags are observations that potentially may deter prescribing or dispensing of a medication. Red flags require further questioning of the patient or clarification prior to writing or dispensing a prescription medication.6
Due Diligence
“The practice of performing reasonable verification that the information presented is accurate and reliable in order to prevent deceptive or criminal practices. Reasonable implies that the practitioner is doing what any practitioner would and should do in the routine activities of the healthcare professional.”7
Readily Retrievable
“Readily retrievable means the record is kept or maintained in such a manner that it can be separated out from all other records in a reasonable time or that it is identified by an asterisk, redline, or some other identifiable manner such that it is easily distinguishable from all other records.”7
Dental practitioner prescribing and office management of controlled substances require vigilance, careful scrutiny of all records, and well-organized record keeping of both patient medical records and controlled substance records.
Prescribing controlled substances
Many dental practices prescribe controlled substance analgesics and anxiolytics prior to performing procedures and postoperatively. Recognition of attempts by patients to illegally obtain controlled substances is necessary to decrease risks to the dental practitioner and the dental practice. State and federal agencies require prescribers to practice “due diligence” when prescribing or dispensing prescription medications. The practice of performing “due diligence” for dental practitioners when prescribing controlled substances includes careful review of the patient’s medical history, review of previously prescribed controlled substances such as that found in the PDMP, evaluation of patient behaviors, patient interviewing, refusing to prescribe or dispense when diversion or fraud is suspected, and reporting these behaviors accordingly.
Currently, many states now require prescribers to evaluate a patient’s PDMP report prior to prescribing controlled substances. (For a more in-depth review of utilizing a state PDMP, see the continuing education article in Implant Practice US: “Practical Considerations for Utilizing Prescription Drug Monitoring Programs — A Primer.”) The PDMP provides controlled substances prescribed for patients that have been dispensed from a community pharmacy or outpatient clinic for a specific state. The PDMP is a helpful tool to optimize therapeutic decisions as well as to detect “red flags” that lead to further questioning prior to prescribing. Table 1 lists red flags commonly detected in a PDMP report.8 Dental practitioners should analyze this report for active controlled substances, recent controlled substance prescriptions from other prescribers, duplicate prescriptions, and early refills. It is important to recognize that any anomalies found should lead to further questioning of the patient since the information provided in the PDMP has not been validated by a secondary source and may have errors that occurred at the time of processing the prescription. Any verified abnormal findings should be thoroughly documented in the patient’s medical record.
Other methods to divert controlled substances from dental practices include altering written prescriptions or falsifying phone-in prescriptions. Tampering of prescriptions is limited by use of tamper-proof prescription pads, and copying of prescriptions is minimized by utilizing embedded watermarks or photocopying resistant paper. The use of preprinted prescriptions with the medication name, medication strength, dosage, and directions is highly discouraged. The use of presigned prescriptions by the prescriber is illegal. Controlled substance prescriptions should be signed the day the written prescription is provided to the patient. Additionally, utilization of ePrescribing can minimize these types of diversion and fraud.
ePrescribing
Electronic prescribing of prescription medications, also known as ePrescribing, began after the passing of the Medicare Modernization Act (MMA) of 2003. The MMA aimed to enhance the quality of patient care while also increasing the utilization of electronic medical records. It wasn’t until 2006, when the Institute of Medicine’s July report discussing the role ePrescribing can play on reducing medication errors, that ePrescribing began to be widely used.9
In 2018, Congress passed the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT Act), which aimed to address the opioid epidemic. In addition, this legislation required Schedule II-V controlled substances for Medicare Part D beneficiaries be ePrescribed beginning January 1, 2021.10 The Centers for Medicare and Medicaid Services (CMS) has since delayed the enforcement of the ePrescribing rule until January 1, 2022. Dental practices and other healthcare providers would clearly find it difficult to delineate Medicare and non-Medicare beneficiary prescriptions, meaning the prescribing of controlled substances must be electronic for all patients going forward. However, individual states are already implementing ePrescribing requirements for controlled substances. Currently, 25 states require ePrescribing with some provider exemptions. More states are expected to pass or implement legislation requiring ePrescribing starting in 2022 and beyond.11 The Centers for Medicare and Medicaid Services (CMS) policy does allow for prescribers to be exempt from ePrescribing controlled substances in the following situations: The prescriber and dispensing pharmacy are the same entity, the prescriber issues 100 or fewer controlled substance prescriptions per year for Medicare Part D patients, or circumstances surrounding natural disasters.12
Dental practices should begin to adopt ePrescribing for all prescriptions, controlled and non-controlled substances, for multiple reasons. Although the federal requirements center around Medicare beneficiaries, the combination of state specific regulations make it logistically difficult for practices to issue prescriptions in two different formats. Adopting ePrescribing can potentially improve medication safety while also preventing prescribing errors. For example, handwritten prescriptions can oftentimes be illegible or difficult to interpret, requiring pharmacists to make judgement calls or delay care for the patient in order to confirm the prescription information. Also, different state and federal requirements exist on the information that must be included on a prescription, including the address of the patient, phone number or address of the practice, and DEA number of the prescriber (for a controlled substance). This information would automatically be included with standardized ePrescribing systems. In addition, electronic prescribing can help with controlled substance diversion or patient selection of medications they want filled or not filled. For example, a patient who is prescribed two handwritten prescriptions for an antibiotic and a pain medication post-dental procedure could provide only the pain medication prescription to the pharmacy and not fill the antibiotic. Finally, ePrescribing enhances and further improves electronic health record information and exchanges of that information. The exchange of electronic health records is becoming more vital as healthcare providers, patients, and insurance companies look to increase communication to better patient care.
Record keeping
Laws and regulations for prescribing, storing, administering, and disposing of controlled substances are defined at the federal level in Title 21, Code of Federal Regulations (CFR), sections 1300-1316.13 The federal Drug Enforcement Agency (DEA) is mandated to ensure compliance to these laws and regulations. Compliance is usually under control of the state’s Boards of Pharmacy and Dentistry. Controlled substances laws and regulations frequently mirror federal laws and regulations. Required records for controlled substances — e.g., purchase receipts, invoices, DEA222 transfer forms, DEA106 theft loss forms, and records of detailed disposed controlled substances such as wastage or damaged product — must be maintained for 2 years and must be “readily retrievable” should a dental practitioner be audited or investigated. It is also important that providers remember to take a biennial inventory of all controlled substances. Individual states can have stricter requirements surrounding how often inventories must be taken.
Ordering and transferring controlled substances
21 CFR 1305.04 and 1305.05 require dental practitioners to be registered with the DEA if they intend to order Schedule II controlled substances (hydrocodone, oxycodone, etc.). They are referred to as a DEA registrant and are assigned a specific DEA registration number. The registrant may give authorization to other individuals to order Schedule II controlled substances through power of attorney. The ordering and transferring of Schedule II controlled substances requires the DEA222 form. The triplicate DEA222 form has been replaced with a single-sheet DEA222 form effective October 2021. The ordering of controlled substance medication Schedules III-V does not require transfer of the medications with the DEA222 form; however, the entities supplying and receiving the controlled substance must maintain records of the transactions.14,15
Storing and access of controlled substances
Title 21, CFR Section 1301.71(a) specifies considerations for storing controlled substances at a business or practice site. Some of these include the type of building, type/quantity of controlled substances to be stored, type of safe, vault or locked steel cabinet, and alarm systems. Controlled substances purchased for dental office practices must be kept in a “locked, well-constructed metal cabinet or safe.” Access to controlled substances should be limited. Equally important is determining who may have access to controlled substances within the dental practice. The DEA lists very specific individuals who may not have access. This list includes the following:
- Any person who has been convicted of a felony offense related to controlled substances
- Any person who has been denied a DEA registration
- Any person who has had a DEA registration revoked
- Any person who has surrendered a DEA registration for cause
Prior to hiring of personnel for the dental practice, it is prudent to complete thorough background investigations and screen for potential exclusions in this list.16
Disposal of controlled substances
How to appropriately dispose of controlled substances and document the disposals are critical considerations when handling these medications. Whenever controlled substances need to be destroyed due to being leftover following patient administration, are found broken, have become contaminated, or have expired, the risk for potential diversion is high. Ideally, these medications should be transferred to a designated “take-back” facility commonly known as reverse distributors. An alternative method involves having the DEA Special Agent in the practitioners’ area destroy the medications on-site. Other alternative methods for destruction may be found in the controlled Substance Act 21 CFR Part 1317. These records must be “readily retrievable” and maintained for 2 years.17
Reporting theft or loss of controlled substances
When dental practitioners suspect theft or loss of controlled substances, they should complete an inventory of controlled substances and immediately file a DEA 106 Theft/Loss form, which is available online or through a downloadable PDF. If theft is suspected by burglary or employee pilfering, local law enforcement should also be notified.
Common violations by dental practitioners
Dental practitioners may be investigated and ultimately prosecuted for a variety of reasons. Frequently, this may involve being nonadherent to federal regulations — e.g., failing to maintain up-to-date inventory records, failure to store controlled substances safely, failure to dispose of controlled substances appropriately, and failing to renew registrant license. Out of convenience, dental practitioners may prescribe medications for nondental-related issues. For example, prescribing oral contraceptives for pregnancy prevention or potent analgesics for migraines would be considered prescribing outside the scope-of-practice. Any prescription ordered by dental practitioners should be within their scope of practice and for a patient with records at the practice site.7
Summary
In summary, management of controlled-substance prescribing practices and record keeping require a comprehensive knowledge regarding methods to detect and deter attempts to divert medications from dental practices. Two important methods to optimize prescribing include use of the state’s PDMP and implementation of ePrescribing. Maintaining detailed records for storage, transfer, and disposal of controlled substances is also necessary to ensure adherence to federal, state, and dental board statutes and regulations. Dental practitioners should only prescribe medications to patients registered with their dental practice.
Before learning about controlled substance record keeping, check out the first part of this series, called “Practical considerations for utilizing Prescription Drug Monitoring Programs (PDMP) — a primer.” Subscribers can take the quiz to obtain 2 CE credits! https://implantpracticeus.com/ce-articles/practical-considerations-for-utilizing-prescription-drug-monitoring-programs-pdmp-a-primer/
References
- The controlled substances act. DEA. https://www.dea.gov/drug-information/csa. Accessed December 22, 2021.
- O’Neil M. Common Substances and Medications of Abuse. In: The ADA Practical Guide to Substance Use Disorders and Safe Prescribing. Wiley Blackwell; 2015.
- Key terms and definitions. SAMHSA. https://www.samhsa.gov/section-223/certification-resource-guides/key-terms-definitions. Accessed December 21, 2021. Accessed March 21, 2022.
- Melton S, Orr R. Detection and Deterrence of Substance Use Disorders and Drug Diversion in Dental Practice. In: The ADA Practical Guide to Substance Use Disorders and Safe Prescribing. Wiley Blackwell; 2015.
- Prescription Drug Monitoring Programs (pdmps). Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/pdmp/index.html. Published May 19, 2021. Accessed March 21, 2022.
- O’Neil M, Winbigler B, Sowards N. Prescription Medication Diversion: Detection and Deterrence. Journal California Dental Association. 2019;47(3):179-185.
- Aquinos C. Office Management of Controlled Substances. In: The ADA Practical Guide to Substance Use Disorders and Safe Prescribing. Wiley Blackwell; 2015.
- Melton S, Orr R. Detection and Deterrence of Substance Use Disorders and Drug Diversion in Dental Practice. In: The ADA Practical Guide to Substance Use Disorders and Safe Prescribing. Hoboken, NJ: Wiley Blackwell; 2015.146
- E-Prescribing. Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/E-Health/Eprescribing. Accessed March 21, 2022.
- R.6 – SUPPORT for Patients and Communities Act. Public Law 10/24/2018. https://www.congress.gov/bill/115th-congress/house-bill/6/text. Accessed March 21, 2022.
- Carter L. 2021 Survey of Pharmacy Law. National Association of Boards of Pharmacy. www.nabp.pharmacy. Accessed March 21, 2022.
- E-prescribing. Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/E-Health/Eprescribing. Accessed March 21, 2022.
- eCFR: 21 CFR Chapter II — Drug Enforcement … https://www.ecfr.gov/current/title-21/chapter-II. Accessed March 21, 2022.
- eCFR :: 21 CFR part 1305 — orders for schedule I and II … https://www.ecfr.gov/current/title-21/chapter-II/part-1305. https://www.ecfr.gov/current/title-21/chapter-II/part-1305/subpart-A/section-1305.04. Accessed March 21, 2022.
- eCFR :: 21 CFR part 1305 — orders for schedule I and II … https://www.ecfr.gov/current/title-21/chapter-II/part-1305. Accessed March 21, 2022.
- eCFR :: 21 CFR 1301.71 — security requirements generally. https://www.ecfr.gov/current/title-21/chapter-II/part-1301/subject-group-ECFRa7ff8142033a7a2/section-1301.71. Accessed March 21, 2022.
- eCFR :: 21 CFR Part 1317 — disposal. https://www.ecfr.gov/current/title-21/chapter-II/part-1317. Accessed March 21, 2022.
- Theft/Loss Reporting. Significant Theft or Loss Reporting of Controlled Substances. Diversion Control Division: https://www.deadiversion.usdoj.gov/21cfr_reports/theft/. Accessed March 21, 2022.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Tyler Dougherty, BA, PharmD, BCACP, received his Bachelor of Arts degree in Biochemistry from Maryville College in 2011 and his Doctor of Pharmacy degree from the University of Tennessee College of Pharmacy in 2015. He completed a postgraduate residency at South College School of Pharmacy in 2016. Dr. Dougherty is a Clinical Community Pharmacist and Assistant Professor of Pharmacy Practice where he specializes in community pharmacy practice and teaches ethics and pharmacy law. Dr. Dougherty is an invited speaker for healthcare professionals teaching ethics and law with emphasis on medication management.
Tyler Dougherty, BA, PharmD, BCACP, received his Bachelor of Arts degree in Biochemistry from Maryville College in 2011 and his Doctor of Pharmacy degree from the University of Tennessee College of Pharmacy in 2015. He completed a postgraduate residency at South College School of Pharmacy in 2016. Dr. Dougherty is a Clinical Community Pharmacist and Assistant Professor of Pharmacy Practice where he specializes in community pharmacy practice and teaches ethics and pharmacy law. Dr. Dougherty is an invited speaker for healthcare professionals teaching ethics and law with emphasis on medication management. Michael O’Neil, PharmD, received his Doctor of Pharmacy from the University of North Carolina at Chapel Hill, North Carolina. Dr. O’Neil has extensive experience in pain management, substance misuse, and medication diversion. Dr. O’Neil was editor and lead author for the American Dental Association’s book titled The ADA Practical Guide to Substance Use Disorders and Safe Prescribing, published in 2015. Dr. O’Neil has served as a consultant for prescription drug misuse and diversion for several entities including the Federal Drug Enforcement Agency. He is currently Professor and Chair of Pharmacy Practice at South College School of Pharmacy in Knoxville, Tennessee.
Michael O’Neil, PharmD, received his Doctor of Pharmacy from the University of North Carolina at Chapel Hill, North Carolina. Dr. O’Neil has extensive experience in pain management, substance misuse, and medication diversion. Dr. O’Neil was editor and lead author for the American Dental Association’s book titled The ADA Practical Guide to Substance Use Disorders and Safe Prescribing, published in 2015. Dr. O’Neil has served as a consultant for prescription drug misuse and diversion for several entities including the Federal Drug Enforcement Agency. He is currently Professor and Chair of Pharmacy Practice at South College School of Pharmacy in Knoxville, Tennessee. Nikki Sowards, PharmD, earned her Doctor of Pharmacy degree in 2012 from the University of Tennessee College of Pharmacy in Memphis, Tennessee. She completed a PGY-1 Pharmacy Practice residency in Knoxville, Tennessee. Dr. Sowards joined South College School of Pharmacy as an Assistant Professor in 2013. In 2015, Dr. Sowards worked as a Director of Hospital Pharmacy in Knoxville, Tennessee. Dr. Sowards is currently an Assistant Professor of Pharmacy Practice at South College School of Pharmacy. She practices at Blount Memorial Hospital where she focuses on pharmacy operations and pharmacy management.
Nikki Sowards, PharmD, earned her Doctor of Pharmacy degree in 2012 from the University of Tennessee College of Pharmacy in Memphis, Tennessee. She completed a PGY-1 Pharmacy Practice residency in Knoxville, Tennessee. Dr. Sowards joined South College School of Pharmacy as an Assistant Professor in 2013. In 2015, Dr. Sowards worked as a Director of Hospital Pharmacy in Knoxville, Tennessee. Dr. Sowards is currently an Assistant Professor of Pharmacy Practice at South College School of Pharmacy. She practices at Blount Memorial Hospital where she focuses on pharmacy operations and pharmacy management.

