Educational aims and objectives
This self-instructional course for dentists aims to discuss 3D printing, how it works, and its benefits and drawbacks and applications for the implant dentist.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the differences between subtractive and additive manufacturing techniques.
- Recognize multiple applications for additive manufacturing in dentistry.
- Realize some oral surgery applications for 3D printing.
- Identify the clinical workflow for chairside 3D printing.
- Define bioprinting and realize its potential for dental applications.
Dr. Aaron Glick, Zain Moin, and Dr. Elham Abbassi offer a comprehensive overview of 3D printing and its applications
Introduction to 3D Printing
3D printing is a relatively new field starting in the 1980s with the understanding of sequentially polymerizing materials with a beam of UV light or laser.1 Since its inception, there has been significant interest and adoption of 3D printing in multiple fields. For example, a 400-square-foot 3D-printed house in Russia was made in 24 hours and at a cost of $10,000.2 Other fields use 3D printing for making automotive parts, fabricating tools in space, concocting custom edible foods, creating educational displays, and executing rapid prototyping for engineering projects. In the health field, bioprinting is being used to build bioactive scaffolds, create human cells, and synthesize implantable tissues.3
Subtractive versus additive manufacturing
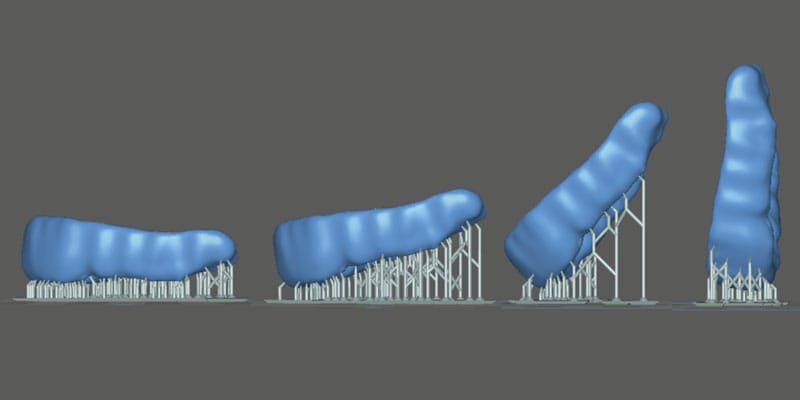
Generally, manufacturing techniques are either subtractive or additive. In subtractive manufacturing (i.e., CNC milling), the material is removed through carving or grinding away at the substructure. In additive manufacturing (i.e., 3D printing), the finished product is built through successive layers of material. Subtractive manufacturing involves a number of axes around which the block of material is rotated so the drill can remove the material, compared with additive manufacturing that will build layers of material in one plane as shown in Figure 1.

The additive nature of 3D printing holds a deep advantage in ease, cost, and flexibility. Due to the rotational axes required, there are some complex parts and internal geometries that are more difficult to manufacture through subtractive manufacturing (Figure 2). For instance, GE changed their manufacturing of some jet fuel nozzles since they could print one piece instead of assembling 20 separate parts.4 The decision to change their manufacturing method resulted in reducing manufacturing costs by 75%. Additive manufacturing allows for flexibility since the setup is minimal compared with retooling that is required for most high scale production facilities. In dentistry, the flexibility is underscored by multiple types of materials that can be used to build specific appliances.

Additive manufacturing technologies
The major categories of 3D printers are fused deposition modeling (FDM), stereolithography (SLA)/digital light projection (DLP), selective laser sintering (SLS), powder binder jetting (BJ), and photopolymer jetting (PJ) (Table 1). FDM printing is the most widely used type of printing that melts a thermoplastic filament. SLA/DLP use UV to cure a liquid photopolymer resting in a vat. This modality is most commonly used for dental applications due to its ability to accurately create small complex parts with resin materials. SLS printers are utilized more commonly in industrial settings and can be found in dental labs as opposed to offices. These printers can output nylon and metal components that have high mechanical properties. BJ printing uses a bed of binder where the printhead deposits a binding agent. PJ jets and cures droplets of liquid photopolymer materials and can build structures that are composed of multiple types of material.5

3D printing in dentistry
3D printing is most cited in manufacturing (automotive and avionics) and consumer good fields followed by the health field.6 In the dental field, the current usage of 3D printers is low according to an American Dental Association (ADA) survey conducted in late 2023 with 17% of dentists owning a 3D printer.7 Yet, the adoption rate is high with those who noted they own a printer, 67% of the dentists have owned the printer for 2 years or less. Additionally, there is interest in this field since 56% of those surveyed noted that they are considering buying a 3D printer or completing training in 3D printing. Manufacturers have been recently rapidly developing new techniques for faster post processing, material sciences, and development of low-cost printers due to the expiration of multiple key patents of additive processes.8
Multiple applications for additive manufacturing in dentistry
There are many applications of 3D printing in the field of dentistry. For instance, 3D printing can be used to create patient models, dentures, occlusal guards, temporary crowns, transitional RPDs, indirect orthodontic bonding trays, direct print aligners, retainers, surgical guides, implants, mandibular advancement devices, and educational devices (Figure 3). The patient models can be static or articulated and flexibly designed or altered digitally depending on the intended use. 3D printed dentures can offer reduced number of clinical appointments and higher intaglio accuracy, however have reduced esthetics compared with conventional dentures.9 The material properties of occlusal guards are similar to conventional and milled methods. Furthermore, wear resistance is not appreciably different between methods.10 Surgical guides can be used in implant placement, complicated root canal morphology, and complex craniofacial surgeries. Static dental implant surgical guides are accurate when 3D printed, however additional factors such as image acquisition with cone beam computed tomography (CBCT), computer aided design (CAD), and slicer software can add errors that affect overall clinical accuracies.11,12

Oral surgery applications
Alongside restorative dentistry applications, 3D printing has revolutionized surgical aspects of the field by enhancing preoperative planning, patient-specific implant fabrication, and surgical simulation. Specifically, patient-specific anatomical models derived from CT or MRI scans enable surgeons to visualize complex structures, which facilitates precise surgical planning and reduces intraoperative errors.13 These advancements allow for improved accuracy in complex reconstructions and better overall surgical outcomes.
The most notable developments in oral surgery involve the creation of custom implants and prosthetics. Advances in material science have allowed for implantable materials that are compatible with 3D printing. For instance, when using the inert material polyetheretherketone (PEEK), osseointegration can be increased using FDM with tunable porosity for diffusion of cells within the microstructure.14 Additionally, 3D-printed surgical guides allow for precise bone cutting and implant placement, further improving surgical efficiency and accuracy.15
Nevertheless, 3D-printed implants have raised concerns among clinicians regarding stress shielding for ceramic materials, long-term remodeling of the bone, and causing a potential immune response.16 Addressing these issues, novel bioprinting techniques are emerging with potential applications in tissue engineering for cartilage and bone regeneration in reconstructive head and neck surgeries.17 These bioprinted constructs aim to better replicate the mechanical properties of native bone while promoting host-derived healing and reducing the risk of immune rejection.18
As 3D printing technology continues to evolve, its applications in surgery are expanding, offering significant promise for future surgical innovations. With the ongoing development of bioprinting and improvements in material science, the integration of 3D printing in dental surgery is expected to further enhance surgical precision, reduce complications, and improve patient outcomes.

Clinical workflow for chairside 3D printing
The integration of these applications in a dental office might vary based on the device that is printed. Generally, the teeth are digitized and altered within a digital design software program and subsequently sent to a 3D printer. Given the cost of SLA/DLP printers, it is more practical to complete all steps chairside instead of sending impressions to a traditional lab. The decision of how to complete these steps also depends on the materials required. Chairside 3D printing has been shown to be less time consuming, more cost efficient, and display similar trueness compared with lab-fabricated single unit crowns using subtractive methods.19
After slicing the stl, the automatically generated G-code can be used to operate the 3D printer. Within the context of a SLA/DLP printer, there is a range of resins that can be used. The manufacturers are required to seek Food and Drug Administration (FDA) clearance for each indication of use.23 Therefore, there will be a set of materials that have been tested for the specific indication and are specifically formulated to have the appropriate mechanical properties.
Once printed, the device will have uncured resin surrounding the printed structure. The process of removing the uncured resin and attaining the structure’s final mechanical properties for a finished, functional product is called post-processing. This is completed in two steps: 1) Submerging the structure in isopropyl wash, 2) Curing the structure. The specifics of post-processing depends on the resin material manufacturer and the resin specifications. It is recommended to closely follow these instructions for use because deviations can result in underperforming mechanical properties and biocompatibility.24-26

After removing the printed solid from the build plate (Figure 6), the supports (if any) can be removed and excess resin washed off. The most widely used solvent washes are isopropyl alcohol and ethanol. Distributing the solvent evenly over the device is an important step to remove uncured liquid resin that has cytotoxic effects on the body. The exposure and permeation time of these solvents reduces the physical properties of the final product. Therefore, there is a fine balance of washing the structure long enough to reduce cytotoxicity but not too long to decrease its flexural strength.27-28
After the solvent has been completely evaporated, the final cure (post-polymerization) is initiated to complete the polymerization reaction. The product is placed in a UV chamber where the temperature, method, and duration will influence the mechanical properties of the end-product. The oxygen-inhibited layer will prevent full polymerization in subsequent steps. For instance, glycerin immersion, nitrogen chamber, and low-pressure vacuum have been methods to reduce the oxygen-inhibited layer. Reducing the oxygen-inhibited layer and reducing viscosity of the resin with higher temperatures has been shown to improve the mechanical properties of the resin.29-30 Generally, an increase of duration and intensity of the UV post-polymerization improves end-product strength.31
The rapid evolution of 3D printing technology is expanding the indications of use, reshaping clinical workflows, and reducing patient case limitations. Ongoing advancements, such as enhanced material properties and increased print speeds, allow for chairside integration. As of 2022, there were approximately 100 rigid and 30 flexible biocompatible resin materials on the market.32 Multiple advanced formulations continue to become FDA cleared, therefore increasing the selections and indications for printing. Additionally, the many types of 3D printing technology allow dental labs to reduce cost and increase throughput.
Future of 3D printing
Bioprinting
Bioprinting, a specialized subset of 3D printing, has gained significant traction in regenerative medicine by enabling the fabrication of functional tissues through layer-by-layer deposition of bioinks containing living cells and biomaterials. This technology has been explored for applications in tissue engineering, drug development, and personalized medicine. Bioprinting has been used to vascularize tissues, skin grafts, and organ models for transplantation and disease modeling.33 The field is rapidly expanding, with research focusing on enhancing cell viability, structural integrity, and biomimetic properties of printed tissues to bridge the gap between laboratory models and clinical applications.34
In dentistry, bioprinting has shown potential for regeneration of soft and hard tissues including bone, cartilage, and mucosa. The development of bioengineered scaffolds infused with stem cells and growth factors has facilitated tooth, periodontal ligament, and alveolar bone regeneration.35-36 In vivo assessments in animal models have been investigated in bone, periodontal ligament, and dentin regeneration with generally positive results.37 As bioprinting technology matures, its integration into clinical practice could revolutionize regenerative treatments in dental surgery by offering patient-specific, bioengineered tissues that improve functional and esthetic outcomes. These tools show promise in maintaining the structural integrity of patient anatomy and in reducing the immune response seen with conventional bone grafts.
Regulation in point-of-care printing
The ability to print custom devices for patients chairside disrupts the traditional workflow of dental offices. Traditionally, dental labs have fabricated all indirect prostheses. However, to maintain patient safety and effectiveness of the devices, the Food and Drug Administration (FDA) has identified software, material, and post-processing controls.38 Because the FDA regulates finished products, it also regulates dental devices at the point of care. Manufacturers will test their material with specific software along the workflow, and any modifications that a dentist makes to the lawfully marketed device could potentially have safety consequences.39 Due to increased controls by the FDA, free market competition is reduced, thus incentivizing manufacturers to build proprietary systems with higher upfront costs to the dentist. Despite commonly used controls, like quality management systems (i.e., ISO 13485), that are common in the industrial manufacturing sector, the specific guidelines for regulatory requirements for chairside 3D printing are sparce.32
Prototypes and innovation
The benefits of 3D printing for small scale, custom products are a notable reason that this technology fits well in dentistry because the majority of extraorally fabricated devices are patient-specific. As more dentists adopt this technology, the path toward fabricating dental-specific prototypes will increase early stages of innovation. Sites similar to thingiverse (thingiverse.com) or makerworld (makerworld.com) have accelerated user-based innovation and pose a possibility for democratizing supply chains — particularly for spare parts manufacturing.40 A recent example showing the importance of supply chain diversification was demonstrated during the COVID-19 pandemic when many dental offices began printing face shields, masks, and other medical devices as demand exceeded supply inventories.41
Re-thinking the application of current innovations in dental material science allows for boundless iterations of traditional designs. For instance, custom implants that do not require surgery (placement at time of extraction), hollow implants that allow for time-based release of anti-inflammatory mediators, and reductions of thickness or chairside implant printing through SLA compatible zirconium dioxide.42
3D printing technology can also be used in tandem with AI (artificial intelligence) in novel ways.43 For instance, AI frameworks have been used to reduce human error and automate critical steps in 3D-printing processing.44 Additionally, both tools can be used in the full digital workflow to create a dental prosthesis: a generative AI computer-aided design can be automatically created, then 3D printed and fitted to the patient.45-46
Summary
Additive manufacturing has multiple applications that are currently used in dental offices. There are still barriers for wide adoption, however the application of a personalized manufacturing approach combined with 3D technologies fits well into a digital clinical workflow. In order to adopt 3D printing in dentistry, an understanding of the different additive technologies and available materials is important. Each type of 3D printing technology has different upfront costs that can preclude its use in a dental clinic. Additionally, the post-processing criteria will vary on the type of print technology selected. Based on current research, 3D printing technology has the potential to reduce time spent and incurred costs for a semi-automated solution of custom dental prostheses.
References
- Pei E, Kabir IR, Leutenecker-Twelsiek B. History of AM. In: Springer Handbook of Additive Manufacturing. 2023 Oct 18 (pp. 3-29). Cham: Springer International Publishing.
- Sakin M, Kiroglu YC. 3D Printing of Buildings: Construction of the Sustainable Houses of the Future by BIM. Energy Procedia. 2017 Oct 1;134:702-711.
- Gu Q, Hao J, Lu Y, Wang L, Wallace GG, Zhou Q. Three-dimensional bio-printing. Sci China Life Sci. 2015 May;58(5):411-9. doi: 10.1007/s11427-015-4850-3. Epub 2015 Apr 29.
- D’Aveni R. The 3-D printing revolution. Harvard Business Review. 2015 May;93(5):40-48.
- Jakus AE. An introduction to 3D printing—past, present, and future promise. In: 3D printing in Orthopaedic Surgery. Elsevier;Jan 2019:1-15. doi:10.1016/B978-0-323-58118-9.00001-4.
- Ukobitz DV. Organizational adoption of 3D printing technology: a semisystematic literature review. Journal of Manufacturing Technology Management. 2021 Dec 17;32(9):48-74.
- Revilla-León M, Frazier K, da Costa J, Haraszthy V, Ioannidou E, MacDonnell W, Park J, Tenuta LM, Eldridge L, Vinh R, Kumar P. Prevalence and applications of 3-dimensional printers in dental practice. J Am Dent Assoc. 2023 Apr 1;154(4):355-356. doi: 10.1016/j.adaj.2023.02.004.
- Kessler A, Hickel R, Reymus M. 3D Printing in Dentistry-State of the Art. Oper Dent. 2020 Jan/Feb;45(1):30-40. doi: 10.2341/18-229-L. Epub 2019 Jun 7.
- Alhallak K, Hagi-Pavli E, Nankali A. A review on clinical use of CAD/CAM and 3D printed dentures. Br Dent J. 2023 Jan 9. doi: 10.1038/s41415-022-5401-5. Epub ahead of print.
- Valenti C, Federici MI, Coniglio M, Betti P, Pancrazi GP, Tulli O, Masciotti F, Nanussi A, Pagano S. Mechanical and biological properties of polymer materials for oral appliances produced with additive 3D printing and subtractive CAD-CAM techniques compared to conventional methods: a systematic review and meta-analysis. Clin Oral Investig. 2024 Jun 25;28(7):396. doi: 10.1007/s00784-024-05772-6.
- Ashtiani RE, Ghasemi Z, Nami M, Mighani F, Namdari M. Accuracy of static digital surgical guides for dental implants based on the guide system: A systematic review. J Stomatol Oral Maxillofac Surg. 2021 Dec 1;122(6):600-6077. doi: 10.1016/j.jormas.2020.10.010.
- Juneja M, Thakur N, Kumar D, Gupta A, Bajwa B, Jindal P. Accuracy in dental surgical guide fabrication using different 3-D printing techniques. Additive Manufacturing. 2018 Aug 1;22:243-255. doi: 10.1016/j.addma.2018.05.012.
- Javaid M, Haleem A, Singh RP, Suman R. 3D printing applications for healthcare research and development. Glob Health J [Internet]. 2022;6(4):217–226. http://dx.doi.org/10.1016/j.glohj.2022.11.001.
- Rendas P, Figueiredo L, Machado C, Mourão A, Vidal C, Soares B. Mechanical performance and bioactivation of 3D-printed PEEK for high-performance implant manufacture: a review. Prog Biomater [Internet]. 2022;12(2):89–111. Available from: http://dx.doi.org/10.1007/s40204-022-00214-6.
- Wu P, Hu L, Li H, Feng L, Liu Y, Zhang S, Li XC, Zhang ML, Yang SY, Lu RJ. Clinical application and accuracy analysis of 3D printing guide plate based on polylactic acid in mandible reconstruction with fibula flap. Ann Transl Med [Internet]. 2021;9(6):460. Available from: http://dx.doi.org/10.21037/atm-20-6781.
- Zhao M, Xiong G, Fang Q, Dong X, Wang F, Han Y, Shen Z, Wang FY. Enlarge the Error Prediction Dataset in 3-D Printing: An Unsupervised Dental Crown Mesh Generator. IEEE Transactions on Computational Social Systems. Dec 2024;PP99:1-12. doi:10.1109/TCSS.2024.3417388.
- Chia HN, Wu BM. Recent advances in 3D printing of biomaterials. J Biol Eng [Internet]. 2015;9(1):4. Available from: http://dx.doi.org/10.1186/s13036-015-0001-4.
- Hollister SJ. Porous scaffold design for tissue engineering. Nat Mater [Internet]. 2005;4:518–524. Available from: https://www.nature.com/articles/nmat1421.
- Mangano FG, Cianci D, Pranno N, Lerner H, Zarone F, Admakin O. Trueness, precision, time-efficiency and cost analysis of chairside additive and subtractive versus lab-based workflows for manufacturing single crowns: An in vitro study. J Dent. 2024 Feb;141:104792. doi: 10.1016/j.jdent.2023.104792. Epub 2023 Nov 25.
- Glick A and Flamenco D. Clinical application and implementation of 3D Printing. J Greater Houston Dent Soc. 2023; 94(4):16-19.
- Shim JS, Kim JE, Jeong SH, Choi YJ, Ryu JJ. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J Prosthet Dent. 2020 Oct;124(4):468-475. doi: 10.1016/j.prosdent.2019.05.034. Epub 2019 Dec 4.
- Alghauli MA, Almuzaini SA, Aljohani R, Alqutaibi AY. Impact of 3D printing orientation on accuracy, properties, cost, and time efficiency of additively manufactured dental models: a systematic review. BMC Oral Health. 2024 Dec 26;24(1):1550. doi: 10.1186/s12903-024-05365-5.
- Da Silva TM, Immich F, De Araujo TS, Lund RG, Da Silva AF, Piva E, Da Rosa WLO. Photosensitive resins used in additive manufacturing for oral application in dentistry: A scoping review from lab to clinic. J Mech Behav Biomed Mater. 2023 May;141:105732. doi:10.1016/j.jmbbm.2023.105732. Epub 2023 Mar 1.
- Cao J, Liu X, Cameron A, Aarts J, Choi JJE. Influence of different post-processing methods on the dimensional accuracy of 3D-printed photopolymers for dental crown applications – A systematic review. J Mech Behav Biomed Mater. 2024 Feb;150:106314. doi: 10.1016/j.jmbbm.2023.106314. Epub 2023 Dec 12.
- Vasques MT, Mulder JN, Machado DS, Lagana DC. The influence of the post-processing method on knoop hardness of photosensitive resins for 3D SLA printer used in Dentistry. Clinical and Laboratorial Research in Dentistry. 2019 Dec 31. Available at: https://www.revistas.usp.br/clrd/article/view/161294.
- Cabrol A, Chuy V, Fron-Chabouis H, Naveau A. Effectiveness of postprocessing on 3D printed resin biocompatibility in prosthodontics: A systematic review. J Prosthet Dent. 2024 Sep 19:S0022-3913(24)00588-2. doi: 10.1016/j.prosdent.2024.08.014. Epub ahead of print.
- Xu Y, Xepapadeas AB, Koos B, Geis-Gerstorfer J, Li P, Spintzyk S. Effect of post-rinsing time on the mechanical strength and cytotoxicity of a 3D printed orthodontic splint material. Dent Mater. 2021 May;37(5):e314-e327. doi: 10.1016/j.dental.2021.01.016. Epub 2021 Feb 18.
- Hwangbo NK, Nam NE, Choi JH, Kim JE. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers (Basel). 2021 Dec 16;13(24):4410. doi: 10.3390/polym13244410.
- Kim YJ, Kim HN, Kim DY. A study on effects of curing and machining conditions in post-processing of SLA additive manufactured polymer. Journal of Manufacturing Processes. 2024 Jun 15;119:511-519. doi:10.1016/j.jmapro.2024.03.112.
- Lim JH, Lee SY, Gu H, Jin G, Kim JE. Evaluating oxygen shielding effect using glycerin or vacuum with varying temperature on 3D printed photopolymer in post-polymerization. J Mech Behav Biomed Mater. 2022 Jun;130:105170. doi: 10.1016/j.jmbbm.2022.105170. Epub 2022 Mar 13.
- Lin YC, Tarrazzi D, Schoenbaum T, Knoernschild K. Effect of postprocessing parameters on the flexural strength of vat-polymerized additively manufactured interim fixed dental prostheses: A systematic review with postprocessing guidelines. J Prosthet Dent. 2024 Aug 13:S0022-3913(24)00497-9. doi: 10.1016/j.prosdent.2024.07.016. Epub ahead of print.
- Guttridge C, Shannon A, O’Sullivan A, O’Sullivan KJ, O’Sullivan LW. Biocompatible 3D printing resins for medical applications: A review of marketed intended use, biocompatibility certification, and post-processing guidance. Annals of 3D Printed Medicine. 2022 Mar 1;5:100044. https://doi.org/10.1016/j.stlm.2021.100044.
- Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol [Internet]. 2014;32:773–785. Available from: https://www.nature.com/articles/nbt.2958.
- Groll J, Burdick JA, Cho D-W, Derby B, Gelinsky M, Heilshorn SC, Jüngst T, Malda J, Mironov VA, Nakayama K, Ovsianikov A, Sun W, Takeuchi S, Yoo JJ, Woodfield TBF. A definition of bioinks and their distinction from biomaterial inks. Biofabrication [Internet]. 2018;11(1):013001. doi: 10.1088/1758-5090/aaec52Available from: http://dx.doi.org/10.1088/1758-5090/aaec52.
- Morrison DG, Tomlinson RE. Leveraging Advancements in Tissue Engineering for Bioprinting Dental Tissues. 2021 Aug;23:e00153. doi: 10.1016/j.bprint.2021.e00153. Epub 2021 Jun 13.
- Ostrovidov S, Ramalingam M, Bae H, Orive G, Fujie T, Shi X, Kaji H. Bioprinting and biomaterials for dental alveolar tissue regeneration. Front Bioeng Biotechnol. 2023 Apr 14;11:991821. doi: 10.3389/fbioe.2023.991821.
- Mohd N, Razali M, Fauzi MB, Abu Kasim NH. In Vitro and In Vivo Biological Assessments of 3D-Bioprinted Scaffolds for Dental Applications. Int J Mol Sci. 2023 Aug 17;24(16):12881. doi: 10.3390/ijms241612881.
- Food and Drug Administration. Technical considerations for additive manufactured medical devices: guidance for industry and food and drug administration staff. Accessed 3/19/2025 at: https://www.fda.gov/media/97633/download
- Kuo RF, Lin YS, Yang TH, Nguyen AT. 3D printing: limitations, safety, and regulatory considerations for oral health science. In: 3D Printing in Oral Health Science: Applications and Future Directions 2022 Sep 27: 269-291. Cham: Springer International Publishing. 10.1007/978-3-031-07369-4_13.
- Euchner J. Democratizing innovation. Research-Technology Management. 2023 Jul 4;66(4):9-10. doi:10.1080/08956308.2023.2212584.
- Longhitano GA, Nunes GB, Candido G, da Silva JVL. The role of 3D printing during COVID-19 pandemic: a review. Prog Addit Manuf. 2021;6(1):19-37. doi: 10.1007/s40964-020-00159-x. Epub 2020 Nov 24.
- Joda T, Yeung AWK, Hung K, Zitzmann NU, Bornstein MM. Disruptive Innovation in Dentistry: What It Is and What Could Be Next. J Dent Res. 2021 May;100(5):448-453. doi: 10.1177/0022034520978774. Epub 2020 Dec 16.
- Glick A, Tipton N, Manila N, Chang J. AI in implant dentistry: clinical implementation and considerations for use. Implant Practice US. 2024;17(1):20-24, Quiz 25.
- Martinez G, Huang K, Lou Y, Bai Y. Innovative Applications of AI and 3D Printing in Digital Dentistry: Enhancing Accuracy and Efficiency in Dental Care. In: 2024 International Conference on Identification, Information and Knowledge in the Internet of Things (IIKI). 2024 Dec 6:237-242. 10.1109/IIKI65561.2024.00048.
- Chau RCW, Chong M, Thu KM, Chu NSP, Koohi-Moghadam M, Hsung RT, McGrath C, Lam WYH. Artificial intelligence-designed single molar dental prostheses: A protocol of prospective experimental study. PLoS One. 2022 Jun 2;17(6):e0268535. doi: 10.1371/journal.pone.0268535.
- Zhao X, Li N, Zhang Z, Hong J, Zhang X, Hao Y, Wang J, Xie O, Zhang Y, Li H, Liu M, Zhang P, Ren X, Wang X. Beyond hype: unveiling the Real challenges in clinical translation of 3D printed bone scaffolds and the fresh prospects of bioprinted organoids. J Nanobiotechnology [Internet]. 2024;22(1):500. Available from: http://dx.doi.org/10.1186/s12951-024-02759-z.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



