Dr. Mark Ludlow shows how digital tools can facilitate a complex anterior implant restoration and streamline the entire implant therapy process.
Dr. Mark Ludlow discusses how adding efficiencies to this implant procedure led to a satisfying result
Implant therapy in the maxillary anterior region is always challenging from both a functional and an esthetic perspective. Tooth proportions, smile line, occlusion, soft tissue contour, and bone volume can all affect the degree of difficulty. However, with careful planning and a robust implant system, it is possible to achieve predictable success in these cases. The case presented demonstrates how digital technologies facilitate a complex anterior implant restoration.
Introduction
By establishing a standardized digital workflow — from diagnosis, to planning, to the creation of customized prosthetics — we can significantly improve outcomes and offer more efficient treatment strategies. In my own practice, I routinely use a combination of CBCT radiography, digital impressions (Primescan intraoral scanner, Dentsply Sirona), and implant planning software (Simplant, Dentsply Sirona) to diagnose and plan each case. I also use various in-house CAD/CAM fabrication technologies to create either temporary and/or final restorations. However, in more complex cases, it is necessary to use more refined or specialized components, such as custom abutments, surgical guides, or edentulous superstructures (Atlantis, Dentsply Sirona).
The following case outlines the care of a patient whose failing maxillary central incisors were replaced with single dental implants, custom abutments, and zirconia restorations.

Case history
A 64-year-old female presented to the clinic as a referral from her general dentist for evaluation of teeth Nos. 8 and 9. Many years ago the patient sustained trauma to her upper anterior teeth, which required both central incisors to be treated with root canal therapy and single crowns. However, her general dentist recently diagnosed both central incisors with internal root resorption during a recall examination. Additionally, the patient reported dissatisfaction with the color of her existing crowns, stating that they do not match the adjacent teeth.
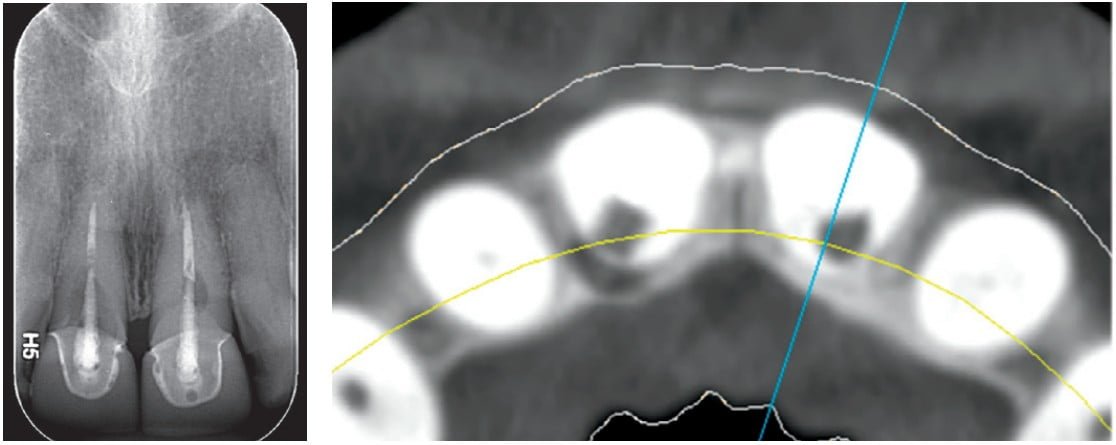
On clinical and radiographic examination, I noted the previously discussed endodontic findings, along with the patient’s esthetic complaint. I also observed several potential challenges in this case, which include a high-smile line, blunted gingival papilla, thin buccal plates, and a bony defect at site No. 8. However, the patient’s thick gingival biotype, shallow anterior occlusion, and square tooth form were identified as more favorable factors. Given the severity, I recommended extraction and implant replacement of teeth Nos. 8 and 9.
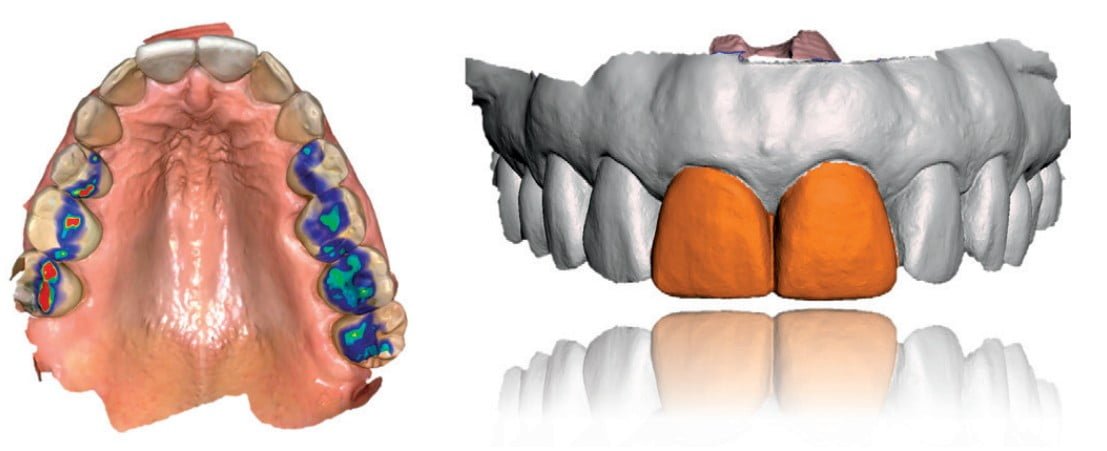
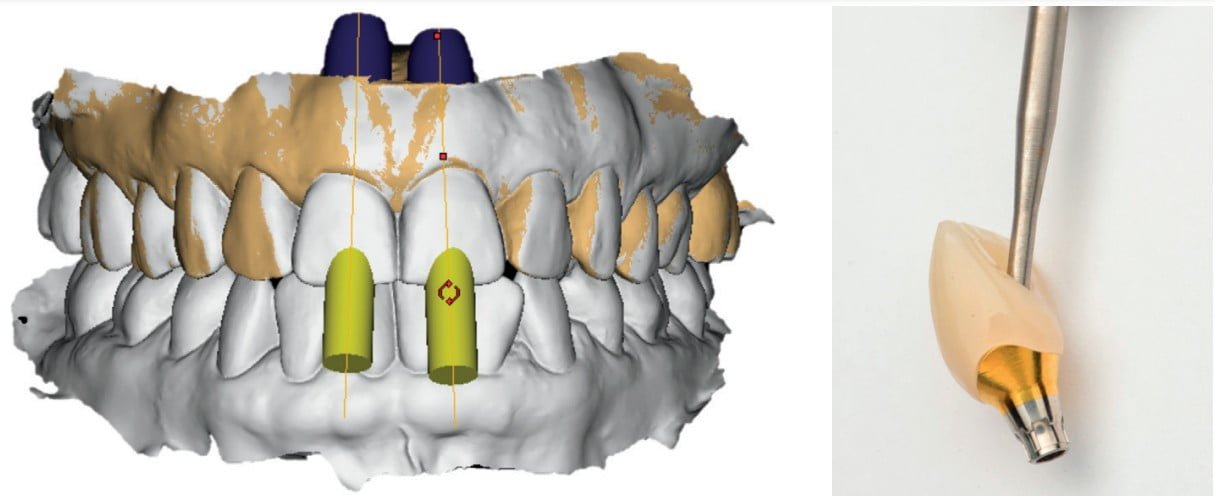
The DCM files from the CBCT scan and the STL files from the intraoral scan were exported and combined in Simplant planning software to confirm our diagnoses, to generate a prosthetically driven treatment strategy, and to order a surgical guide/ template. The patient’s bone volume and gingival biotype were well suited for immediate implant placement, assuming an intact buccal plate following extraction. Further, assuming adequate primary stability can be achieved at implant placement, the plan is to immediately provisionalize both sites. Following finalization of the treatment plan, I ordered and received the surgical guide, the custom abutments, and a core file to design and fabricate PMMA provisional crowns prior to the surgery.

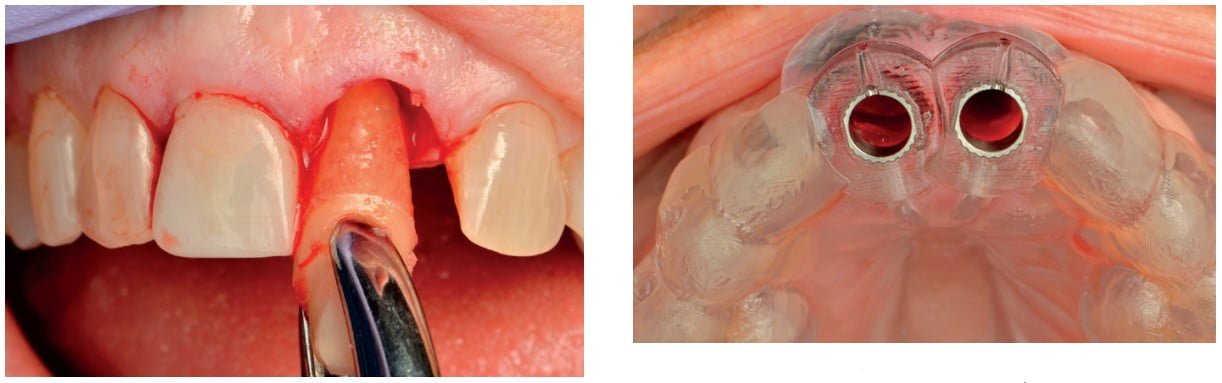
On the day of surgery, I carefully extracted teeth Nos. 8 and 9 to preserve the buccal plate, and curetted and irrigated each socket. Next, the surgical guide was seated, and the osteotomies prepared with each drill passing through the guide. Implants 8 and 9 (4.2 Astra Tech Implant System EV, Dentsply Sirona) were then placed through the guide. However, the primary stability was not sufficient for immediate loading. Therefore, cover screws were placed in each implant, and the sites were grafted with demineralized allograft and collagen membranes. A bonded temporary restoration was fabricated with multilayered PMMA directly in the practice using the inLab software and the inLab MC X5. The custom abutment and PMMA provisional will be saved for use in the second-stage procedure.
After 4 months of healing, the sites were uncovered, and osseointegration was confirmed. The previously fabricated Atlantis custom abutments were inserted along with the PMMA provisional crowns to facilitate tissue shaping over the next 6 to 8 weeks. Once the soft tissue contours were acceptable, the temporary crowns were removed, and an abutment level scan was made with Primescan. This final intraoral scan was merged with the design files of the original abutments to allow fabrication of the final restorations. The advantage of this technique is that the original abutments are not needed to be removed, and no additional effort is needed to expose/capture the margin line. The temporary crowns were also scanned and were used as a guide for the contours of the final restorations. Two zirconia screw-retained crowns were designed and fabricated to match the shade of the adjacent teeth. However, when attempting to insert the final restorations, I noticed the shade was slightly off. As a trained dental technician, I took this as a challenge. I then milled multiple sets of zirconia crowns and customized them differently for the patient to get the perfect shade and fit. Once the case was completed, the patient was very satisfied with the outcome.

Discussion
This case highlighted many of the challenges commonly found in anterior implant therapy. However, with careful planning, the right tools, and precise execution, optimal results were achieved. Further, the technologies and materials utilized in this case allowed us to react to the clinical situation and to make the correct intraoperative decisions for optimal outcome.
Intraoral scanning is an essential part of this workflow. The accuracy of Primescan is reflected in the precise fit of both the surgical guide and the final restorations. Primescan is an invaluable tool in both the diagnosis and monitoring of dental disease as well as in patient education and communication. Scan data can easily be exported to planning software, laboratories, or CAD/CAM devices.

Simplant gives the clinician the ability to view 3D data from any CBCT scanner, create virtual wax-ups, and plan cases using its extensive implant library. For those situations requiring guided surgery, Simplant makes it easy to order precise surgical guides for practically any implant system available today. Further, the link between Simplant and Atlantis allows the design and fabrication of custom abutments, based directly off the surgical planning.

This digital workflow streamlines the entire process of implant therapy. All steps are coordinated to avoid compatibility issues. Even if primary stability cannot be achieved initially during implant insertion, and closed healing is advisable, the fabricated abutments can be used as intended in the restorative restoration.

Patients also appreciate the difference of a digital workflow. The ability to illustrate problems, discuss treatment options, and actively involve patients in the decision-making process are vital to patient education and provider trust. Further, the reduction in chair time has an extremely positive effect on patient perception. Taken together, these differences contribute to better case acceptance and ultimately case success.
Conclusion
The patient was very satisfied with both the process and the result. She was particularly impressed by the appearance of the provisional restorations, and at first, she thought they were the definitive restorations. Her husband stated that he “couldn’t imagine how we could do better,” but through the leveraging of digital tools, we were able to achieve even better results, and now the patient can smile confidently again.
Dr. Bernard Touati also has written about anterior implant restoration and soft tissue management in the anterior region. Read his article, “Anterior implant esthetics,” here: https://implantpracticeus.com/anterior-implant-esthetics/
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



