Editor’s intro: Implant complications can occur in even the best of conditions, but how clinicians handle the setbacks is key to moving forward with the best solution. Read Dr. Moody’s article to see his insights on achieving resolution to those challenges.
Dr. Justin D. Moody discusses how to handle inevitable setbacks

Implant dentistry works very well most of the time, thank goodness. But when we have issues or complications, it often means lost chair time, materials, and lab fees. To me, those things are just a part of dentistry. It happens to all of us, but what defines us is how we handle these setbacks. Before charging forward to fix the problem, clinicians must take a step back and investigate — start with the “Why did this happen?” It’s only after you discover this that you truly can move forward with the solution.
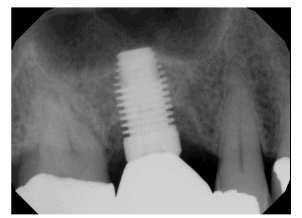
When talking with other dentists who place and/or restore dental implants, it seems the number one complication is bone loss around the dental implant. For some, this happens immediately after implant placement, and for others, it takes months and in many cases years before we see these effects on the radiographs or in a clinical manifestation.
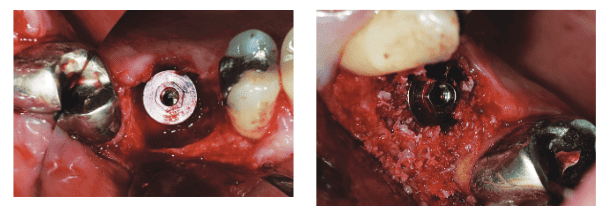
I want to share the story of a patient who recently came in after treatment over 10 years ago. Unfortunately, he was never good about coming in for re-care. The hygienist found a deep probing and took a periapical radiograph that was less than flattering to the eye — the tooth had bone loss and purulence around what was until recently a very solid and longtime functional restoration. I discussed my findings with the patient and told him that I would like to remove the crown/abutment to get a better look, maybe even grafting the case.
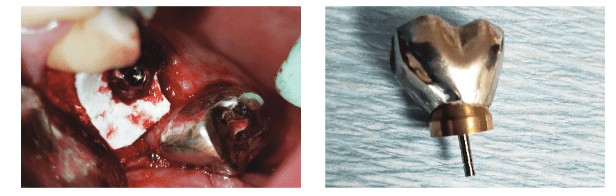
I accessed the crown/abutment and removed it only to find residual cement and granulation tissue all around the implant. There was my why! I removed the granulation tissue, cleaned the implant with an iBrush (NeoBiotech), rinsed with citric acid, placed some MinerOss® Cancellous graft material (BioHorizons®) around it and a sheet of Mem-Lok® (BioHorizons) over the graft, seated the cleaned-up crown/abutment, and sutured the tissue with some 4-0 PGA. I will follow the case at 1-week, 1-month, and 6-month intervals in hopes of achieving some resolution.
You may be wondering if I charged him for that day’s treatment. In this case, I elected to treat the patient for free, understanding that he was not the most loyal re-care patient, but when you stop to look at it, I was the one who left the residual cement behind, me and only me. Just do the right thing; it always works out best and lets you sleep well at night.
Read more of Dr. Moody’s insights on implant complications in “So you have a complication. …”
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Justin D. Moody DDS, DABOI, DICOI, is a Diplomate in the American Board of Oral Implantology, Diplomate in the International Congress of Oral Implantologists, Honored Fellow, Fellow, and Associate Fellow in the American Academy of Implant Dentistry, and Adjunct Faculty at the University of Nebraska Medical Center. He is an internationally known speaker, founder of the New Horizons Institute Non-Profit Clinic, and Director of Implant Education for Implant Pathway. You can reach him at
Justin D. Moody DDS, DABOI, DICOI, is a Diplomate in the American Board of Oral Implantology, Diplomate in the International Congress of Oral Implantologists, Honored Fellow, Fellow, and Associate Fellow in the American Academy of Implant Dentistry, and Adjunct Faculty at the University of Nebraska Medical Center. He is an internationally known speaker, founder of the New Horizons Institute Non-Profit Clinic, and Director of Implant Education for Implant Pathway. You can reach him at 

