
 Dr. Ronald Delmanto required creative treatment planning for a patient after jaw resection
Dr. Ronald Delmanto required creative treatment planning for a patient after jaw resection
When a patient named Al visited his general dentist several years ago, a routine appointment turned into a life-changing event. After an FMX series, a review of the radiographs showed suspicious dark radiolucent areas below the teeth and in the bone.
[userloggedin]
The patient was referred to the University of Medicine and Dentistry in New Jersey, where it was ascertained that Al had multiple ameloblastomas, a rare, noncancerous (benign) tumor that develops most often in the jaw near the molars. If these extremely aggressive neoplasms are not excised completely, they can reoccur and result in bone destruction. The patient had no symptoms. After diagnosis and oral surgery, the road to both physical and esthetic recovery required creative planning, and 3D imaging played a significant role in the reconstruction process.
To remove these lesions, the surgeon resected the portion of the mandible that extended from the mesial of tooth No. 18 around to the mesial of tooth No. 27, quite an extensive area. After the resection, a metallic bar was screwed into the intact portions of his jaw for support. At a second surgery, the jaw was reconstructed utilizing a cadaver rib and bone marrow from the patient’s hip. After the jaw resection, the patient was dejected. He could not chew on left side at all, had no anterior teeth on the bottom, and he was very unhappy with his esthetic appearance. He was an active and robust man in his mid-50s, a retired New Jersey state police major, so this was crushing from both a functional and esthetic point of view.
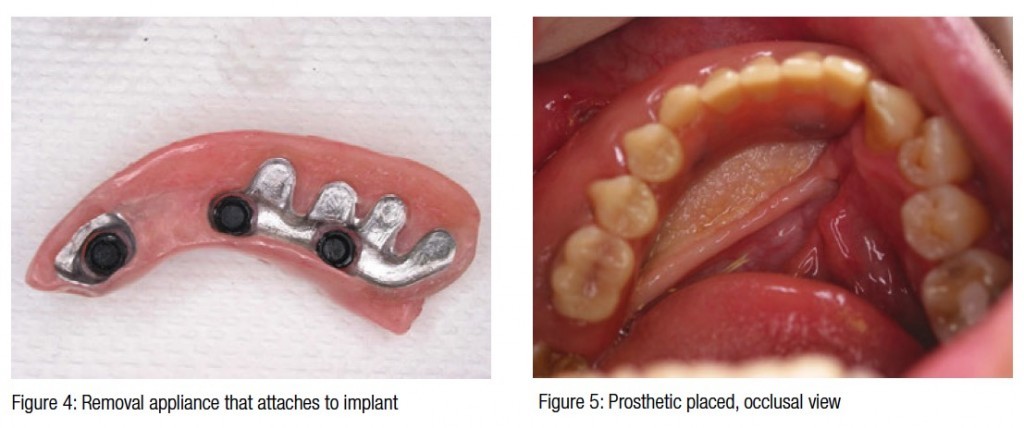
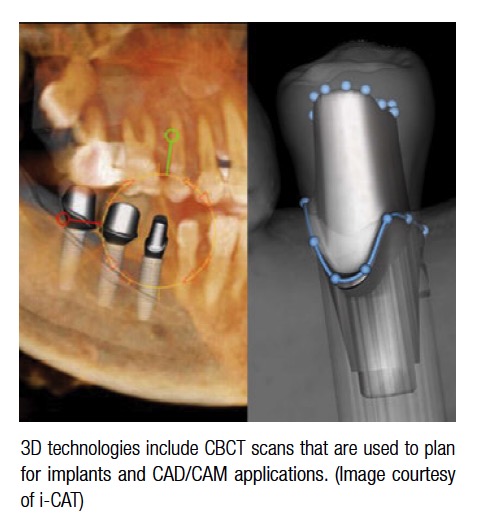
 After the graft was allowed to mature for 8 months, the patient came to me for a reconstruction treatment plan. An i-CAT™ 3D scan (i-CAT™) was taken, and treatment planning software was used to accumulate all of the data and measurements necessary to complete the reconstruction and devise a plan for this rather challenging anatomical issue. After the resection, the jaw had ended up too far buccally and labially for the type of treatment that I first had considered. I had originally intended to perform routine crown and bridge, but in that case, the buccal aspect of the teeth would have protruded too far into the cheek and the lip. I had surgical guides created and then (Figure 1) surgically placed the implants (Figure 2), and then conferred with the laboratory. Instead of crown and bridge, we created custom castings and a framework that attached to the implants (Figure 3). I planned the framework to protrude more lingually, and then placed LOCATOR® attachments (Zest Anchors) on the framework and reconstructed the jaw with a removable appliance (Figures 4-6).
After the graft was allowed to mature for 8 months, the patient came to me for a reconstruction treatment plan. An i-CAT™ 3D scan (i-CAT™) was taken, and treatment planning software was used to accumulate all of the data and measurements necessary to complete the reconstruction and devise a plan for this rather challenging anatomical issue. After the resection, the jaw had ended up too far buccally and labially for the type of treatment that I first had considered. I had originally intended to perform routine crown and bridge, but in that case, the buccal aspect of the teeth would have protruded too far into the cheek and the lip. I had surgical guides created and then (Figure 1) surgically placed the implants (Figure 2), and then conferred with the laboratory. Instead of crown and bridge, we created custom castings and a framework that attached to the implants (Figure 3). I planned the framework to protrude more lingually, and then placed LOCATOR® attachments (Zest Anchors) on the framework and reconstructed the jaw with a removable appliance (Figures 4-6).
 This treatment plan worked very favorably — it restored the dentition, and by utilizing a removable appliance, we reconstructed much of the tissue that he lost after the oral surgery. Before reconstruction, the left lower side of Al’s face appeared to be collapsed, as though his lip had no support. When his case was completed, we were able to reconstruct much of that lost tissue with acrylic and the teeth placement. As a result, he regained the ability to chew on that side, and esthetically, he had a fuller lip support and looked basically the same as he did prior to the surgery (Figure 7).
This treatment plan worked very favorably — it restored the dentition, and by utilizing a removable appliance, we reconstructed much of the tissue that he lost after the oral surgery. Before reconstruction, the left lower side of Al’s face appeared to be collapsed, as though his lip had no support. When his case was completed, we were able to reconstruct much of that lost tissue with acrylic and the teeth placement. As a result, he regained the ability to chew on that side, and esthetically, he had a fuller lip support and looked basically the same as he did prior to the surgery (Figure 7).
From the time the jaw was resected, the process took approximately 1½ years.
A CBCT imaging system was a very valuable asset to this case. Besides the extremely precise data that I gained from the 3D scans, I performed the surgery utilizing the CBCT scans in conjunction with surgical guides. I am proud to say that I presented this case to a clinic in Miami several years ago, and Dr. Carl Misch, whose implant course I have taken several times, complimented me about how straight and in-line the implants were. I would not have been able to plan and implement the case with such accuracy and precision without the information from the i-CAT scans and the surgical guide created from the scan data, both of which helped me to determine the precise spacing and parallelism. The spacing is so good that we have had no residual problems. In fact, normally, I have to change the male inserts for the LOCATOR attachments that wear out periodically, depending on the individual patient’s chewing habits. I have not changed Al’s LOCATORS since 2006 because he is biting so evenly.
The surgeon, patient, and I are all pleased about the outcome of this case. Professionally, I see Al every year, and he is still happy with the outcome. He has regained function and eats anything he wants. I am especially satisfied that I was able to build out some of the soft tissue that he had lost, which gave him his smile back.
As a result of what I have learned from doing the difficult cases, I don’t plan even a single unit now without using a CBCT system. As with this case, symptomless anatomical anomalies may catch us by surprise, but 3D imaging allows me to diagnose and treatment plan decisively with a phenomenal amount of data to help patients, like Al, regain their physical health, comfort, and self-esteem. Besides being my patient, Al is also my wife’s cousin, so I am happy to have the opportunity to see my handiwork and his smile at his daughters’ weddings and the recent christening of his grandchildren, as well as when we go fishing together.
[/userloggedin]
[userloggedout][/userloggedout]
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Ronald Delmanto, DDS, received his undergraduate degree at Seton Hall University, and dental degree at Fairleigh Dickinson University School of Dentistry. He also served in the Air Force for 3 years as a dentist. He has had extensive training on implant procedures and practices general dentistry in Toms River, New Jersey. Dr. Delmanto has no financial interest in i-CAT.
Ronald Delmanto, DDS, received his undergraduate degree at Seton Hall University, and dental degree at Fairleigh Dickinson University School of Dentistry. He also served in the Air Force for 3 years as a dentist. He has had extensive training on implant procedures and practices general dentistry in Toms River, New Jersey. Dr. Delmanto has no financial interest in i-CAT.

