Dr. Timothy Kosinski illustrates treatment of a patient affected by maxillary lateral incisor agenesis

Maxillary lateral incisor agenesis (MLIA) is a condition in which at least one of the maxillary lateral incisors is missing in the primary or permanent dentition. One of the most common congenital anomalies, MLIA occurs in the smile zone and affects both dental esthetics and function.
[userloggedin]
These problems can impact the self-esteem and social relationships of individuals with this condition.1,2
As innovations in dental implants and prosthetic materials have been made, esthetic restoration of dental function has become a straightforward, predictable process. With advanced designs and surface treatments, modern implants integrate exceptionally well, ensuring long-term stability and function. Implant dentistry is an excellent mode of treatment for improving the lives of patients with MLIA. Although tooth replacement at the maxillary lateral incisor site may present challenges due to limited anatomical space and its location in the esthetic zone, implant therapy has become one of the primary treatment options for addressing this anomaly.3 In addition to providing optimal, esthetic restorative results, this mode of treatment preserves the alveolar ridge.

For patients with MLIA, implant therapy is a conservative approach that avoids damage to the morphological features of neighboring dentition.1 Provided the available space is sufficient for implant placement, treatment is relatively noninvasive because adjacent teeth do not need to be prepared for a bridge. In the event that there is not enough room to receive an implant, it is possible to create the necessary space through orthodontics.4
The following case summary demonstrates implant placement in a 20-year-old female who presented with an acid-etch bridge that was used to restore her congenitally missing maxillary right lateral incisor. Following orthodontic therapy that had straightened the patient’s smile, the existing bridge was placed and maintained the mesial-distal space nicely during the patient’s formative years. Although esthetic, the patient’s bridge was unstable and fell off periodically. Due to problems with long-term retention, the acid-etch bridge is not considered a viable permanent solution.5
The young college student was interested in single-tooth replacement and had discussed dental implant treatment with her general dentist. The Hahn™ Tapered Implant System (Glidewell Direct, Irvine, California) was utilized to restore the missing tooth. The implant system includes implants with narrower diameters, a feature that is beneficial for cases in which space is limited. Additionally, the tapered body of the implant is ideal for use in anatomically constricted areas. The prominent thread design also allows the implant to be more easily positioned and controlled by the clinician during placement. Following integration of the implant, a cement-retained BruxZir® Anterior crown provided a strong, esthetic final result.
Case summary
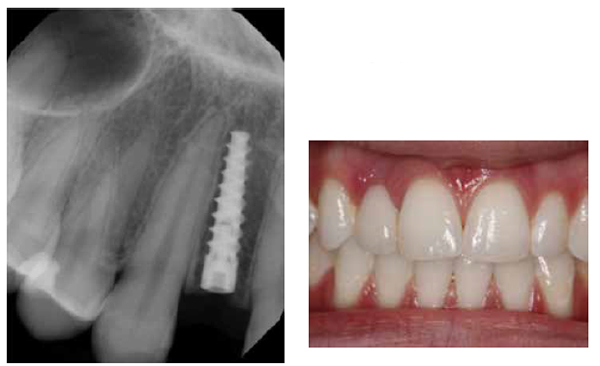
The patient presented with a cuspid and central incisor that were minimally prepared on the palatal aspect to support the wings of the acid-etch bridge (Figure 1). The acid-etch bridge was indeed nice and esthetic (Figure 2). However, the patient was mainly concerned about long-term function. There was no indication to prepare the adjacent teeth for a conventional 3-unit bridge.
Although there were no medical contraindications to implant therapy, the amount of space between the adjacent natural teeth was minimal. As mentioned earlier, the lateral incisor site can present some difficulties when surgically placing dental implants. The facial-palatal width is often compromised, especially for cases in which the edentulous condition is congenital. A digital periapical radiograph of the edentulous site indicated, however, that there was enough space to surgically position and accept a dental implant (Figure 3).


When placing an implant, the practitioner needs to be certain that the angulation, depth, and position of the implant are appropriate to allow for a natural emergence profile. For this case, scans were taken using the PaX-i3D Green imaging system (VATECH America Inc., Fort Lee, New Jersey) for CBCT image analysis. The sagittal view of the scan illustrates the amount of vertical and horizontal bone that was available (Figure 4). The amount and quality of bone was precisely determined with the imaging software. Virtual placement of the implant can also be performed, helping the practitioner select the appropriate implant size and visualize how the implant should be positioned in the edentulous space. Because the patient’s anatomy did not present any complications, the implant was placed without the use of a surgical guide.

After treatment planning, the acid-etch bridge was easily removed from the adjacent teeth (Figure 5). This revealed a defect on the facial contour of the edentulous space. Due to the lack of interseptal bone, no interdental papillae were present (Figures 6A-6B).
A pilot drill was centered between the teeth adjacent to the edentulous site. The osteotomy was positioned approximately 3-mm palatal to the facial aspect of the adjacent dentition to allow for the best esthetics and enough facial room for a custom abutment and implant-retained crown. The mesial-distal angulation of the drill was checked with a periapical radiograph. The diameter of the osteotomy was slightly smaller than that of the implant chosen for this case, and a depth of approximately 13 mm was established (Figure 7).
A 3.0-mm-diameter Hahn Tapered Implant was chosen for this case. The diameter size and tapered body of the implant was ideal for the limited space that was available. Additionally, the implant features prominent threads, which ease placement and allow the clinician to thread the implant into an undersized osteotomy (Figure 8). The ability to place an implant in a slightly smaller osteotomy can help ensure excellent primary stability.6 This is especially beneficial in cases where bone quality is not optimal.
Because her acid-etch bridge would function as a transitional appliance during the period of healing and osseointegration, a cover screw was hand-tightened into the implant (Figure 9). As illustrated in the radiograph, the implant was nicely positioned (Figure 10). A postoperative CBCT scan was used to verify the position of the implant and proper maintenance of the facial bone.



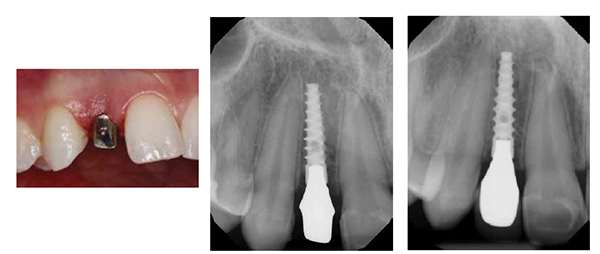
The patient’s acid-etch bridge was then cemented back onto the adjacent teeth (Figure 11). Four months following surgery, the patient returned to begin the restorative process (Figure 12). A tissue punch was utilized to access the healed implant site (Figures 13A-13B).
Because of the relatively noninvasive nature of the tissue punch, the final impression was taken during the same visit. The cover screw was removed, and an impression coping was hand-tightened into the conical internal hex connection of the Hahn Tapered Implant (Figures 14A-14B). Panasil® vinyl polysiloxane material (Kettenbach, Huntington Beach, California) was used to create a final impression so the dental lab could fabricate the restoration (Figure 15).
Based on the final impression, the lab produced an Inclusive® Titanium Custom Abutment and an esthetic BruxZir® Anterior crown. In order to achieve symmetrical esthetics and occlusion when the patient is missing only one maxillary lateral incisor, the dimensions of the restoration should be primarily dictated by those of the contra-lateral tooth.3 Thus, the lab aimed to mimic the shape and contours of the contra-
lateral incisor.
Because the patient could return to the dental office only during school breaks, the patient again used the acid-etch bridge as a transitional prosthesis. At the final delivery appointment, the soft tissue was once more removed using a simple tissue punch (Figures 16A-16B). The custom implant abutment was then placed, and the prosthetic screw was tightened. Note that the margins of the abutment were just slightly subgingival, making removal of the cement easy and predictable (Figures 17A-17B).
The final crown was cemented on the custom abutment. A final radiograph verified complete seating of the restoration (Figure 18). The patient was pleased to have a fixed restoration that exhibits high stability, strength, and esthetics (Figure 19).
Conclusion
Implant treatment is an excellent method of restoring dental function and esthetics. Understanding the complexity of the patient’s condition is imperative to the long-term success of the case. Choosing not only the right dental implant, but also considering the proper prosthetic components is important. In this case, implant treatment proved to be an outstanding treatment modality in a difficult situation, and the Hahn Tapered Implant allowed for surgical predictability and reliable osseointegration.
[/userloggedin]
[userloggedout][/userloggedout]
- Pini NI, De Marchi LM, Pascotto RC. Congenitally missing maxillary lateral incisors: update on the functional and esthetic parameters of patients treated with implants or space closure and teeth recontouring. Open Dent J. 2014;8:289-294.
- Willhite C, Bellerino M, Eubank J. Treatment of congenitally missing lateral incisors with resin-bonded fixed partial dentures. Quintessence Dent Technol. 2002:63-72.
- Richardson G, Russell KA. Congenitally missing maxillary lateral incisors and orthodontic treatment considerations for the single-tooth implant. J Can Dent Assoc. 2001;67(1):25-28.
- Nirola A, Bhardwaj SJ, Wangoo A, Chugh AS. Treating congenitally missing teeth with an interdisciplinary approach. J Indian Soc Periodontol. 2013;Nov;17(6):793-795.
- El-Mowafy OM. Posterior acid-etch bridge—a modified retentive design. J Can Dent Assoc. 1996;Nov;62 (11):862-865.
- Degidi M, Daprile G, Piattelli A. Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: an in vitro study. J Oral Maxillofac Surg. 2015;Jun;73(6):1084-1988.
Article published with permission from Inclusive magazine.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



