Editor’s intro: Evolving techniques and trends for 2019, such as 3D technologies and guided surgery, discussed by Dr. Nichols, are expected to drive implant planning and placement next year and beyond.
Dr. Matthew Nichols discusses some trends that will change practice protocols in the future


As the end of each year approaches, it’s helpful to look back at the technology and techniques that have furthered the evolution of implantology — and it’s just as exciting to think about what the future holds for the oral surgery specialty. Below are just a few of the trends that I think will drive implant planning and placement in 2019.
Technology
Smart CBCT
I was trained to use cone beam computed tomography (CBCT) about halfway through my degree in the mid-2000s. Where we’ll see advancements in 2019 is in “smart” CBCT. Much like the smart technology we think of that makes our daily lives easier (devices that intuitively adapt to their environment; respond to our voices; or predict our desires based on previous interactions), we’ll see similar advancements in our practices. Touchscreens will be incorporated with the system so a computer screen and mouse will become optional. Built-in video cameras will aid with patient positioning as well as facial scanning. Quality control features will either autocorrect mistakes or alert users before the scan is taken. Most important, advancements in technology will keep radiation dose at a minimum for patients, and scan times will be faster than ever. We’ve seen a trend toward all-in-one systems, and future CBCT systems will continue in this direction, with multiple fields of view and upgradable options for cephalometric imaging to appeal to all specialists.
Implant planning software
With new research confirming that virtually planning implants increases their angular accuracy during surgery,1 we’ll see further advancements in software that help doctors virtually plan and place implants. The rise of the “crown-down” approach to implant planning is also driving demand for intuitive planning software that leads to greater predictability in the success of the implant and final restoration. Additionally, software that can automatically merge STL files from an intraoral scanner with the DICOM files of a CBCT system, such as the Prosthetic-Driven Implant Planning (PDIP) Module, will give an added layer of confidence in planning — not to mention a powerful communication tool for patients.
3D printing
Three-dimensional printing has exploded in popularity across all industries, and oral surgery is no exception. Aiding in the spread of this technology is a significant decrease in the cost of buying a printer — as low as $3,000 instead of $25,000 as in years past. For example, since bringing 3D printing in-house a year and a half ago, I have printed all my own surgical guides. I’m able to do so for approximately $30 a guide, rather than $400-$500; it’s more cost-effective for my practice and also protects my patients from any surprise lab fees that may be passed down to them. By cutting out the middleman, I can also collaborate directly with the referring GP. Based on the number of phone calls I receive from colleagues asking about my 3D-printing workflow, we’ll see more doctors of all specialties bring 3D printing in-house.
Techniques
Guided surgery
Many of the technological advancements above make new techniques possible. As such, we’ll see more doctors take advantage of guided implant surgery. If virtual implant planning increases the accuracy of implant planning and placement, as previously mentioned, then using a restrictive drill guide increases the angular and depth accuracy even more. Surgical guides also allow doctors to take a flapless approach, with means less healing time for patients. The predictability of guided surgery will even help doctors save on supplies. In the past, I would have to order five to six implants to ensure I’d be covered during surgery. In 2019, an implant will be virtually placed from a digital implant library, and the necessary implant will be ordered for the day of surgery. In addition to the advanced software and 3D printing that will make guided surgery prevalent in the coming year, surgical navigation systems will also aid with accuracy and safer surgeries.
Trends
Greater collaboration among specialties

Open communication among doctors will lead to more efficient treatment and faster turnaround times (in healing, having implants restored, receiving appliances, etc.) for patients. Again, it’s all possible thanks to advancements in technology. I’m able to share the full version of my CS 3D Imaging software with referrals, so they can see exactly what I see when discussing a patient’s case. Open systems, in general, also make it easier to export and share files. Since I serve a small rural community, many doctors send their patients to me for CBCT imaging, especially orthodontists, rather than sending them to a hospital.
We’ll also see more multispecialty practices as referral relationships evolve into business partnerships. With more equipment being designed to handle several workflows — such as intraoral scanners that can be used for restorations, orthodontics, and implant-borne restorations, and CBCT systems that are ceph-ready — several different specialists can benefit from technology used in one multidiscipline practice. In 2019, there will be no reason to work in a silo since working across specialties will benefit doctors and patients so much more.
“2019” comes early
As previously mentioned, I was trained on CBCT in school and have never practiced without it. However, I recognize that the technology behind 3D imaging systems and software keeps evolving, which can be daunting to some. Fortunately, I recently had the opportunity to implement one of the newest CBCT systems on the market: Carestream Dental’s CS 9600 system. This new system features smart technology to aid oral surgeons and their teams in providing exceptional care. For example, a built-in SmartPad guides my team in positioning patients and previewing images. Smart-automated technology incorporates much of what we know about medical imaging — photographic scout, radiographic scout, etc. — so the team can capture a smaller area more effectively, or a larger area more easily, with fewer retakes. The system can also detect and visually indicate if the wrong accessory is inserted for the selected procedure and recommends the appropriate one.
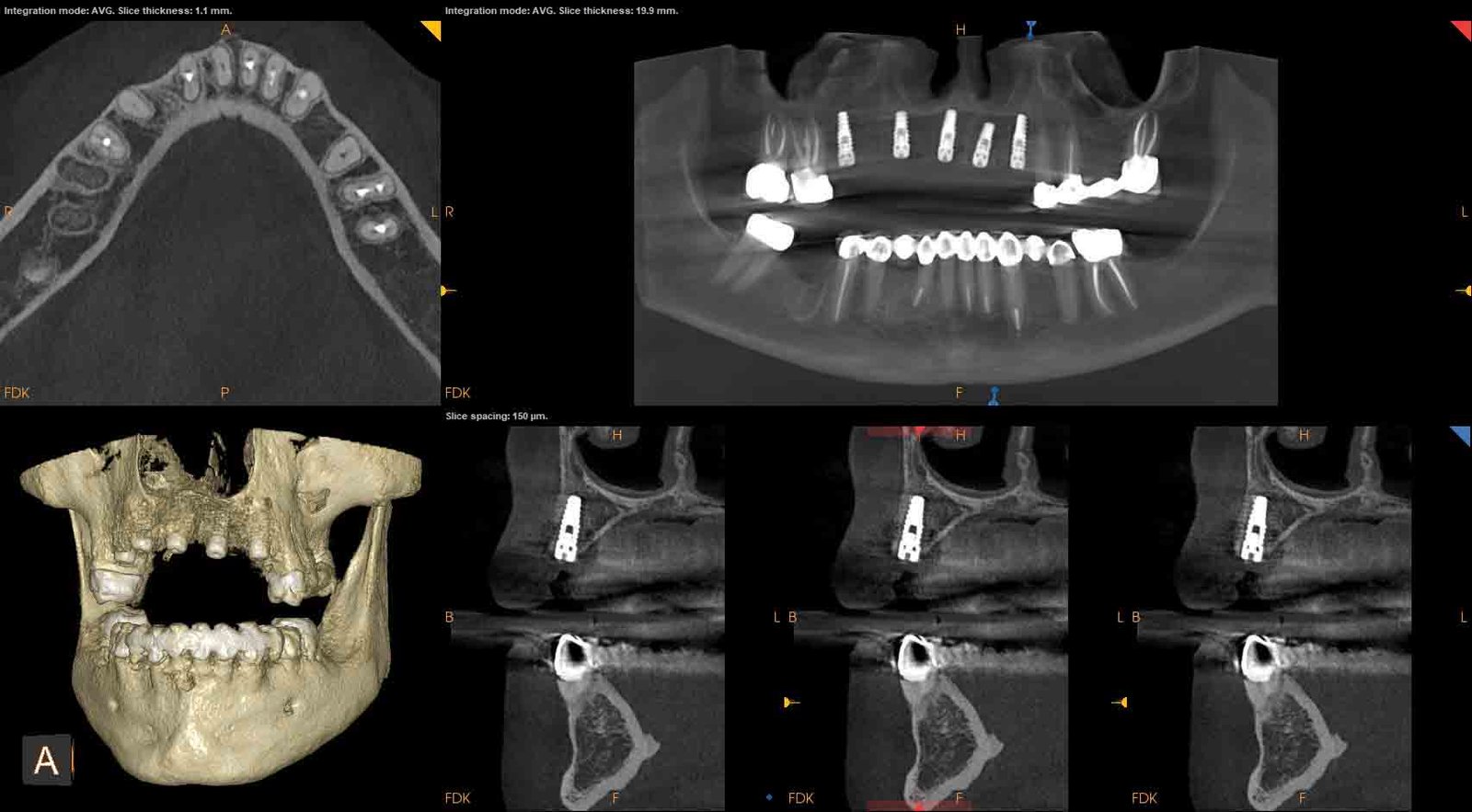
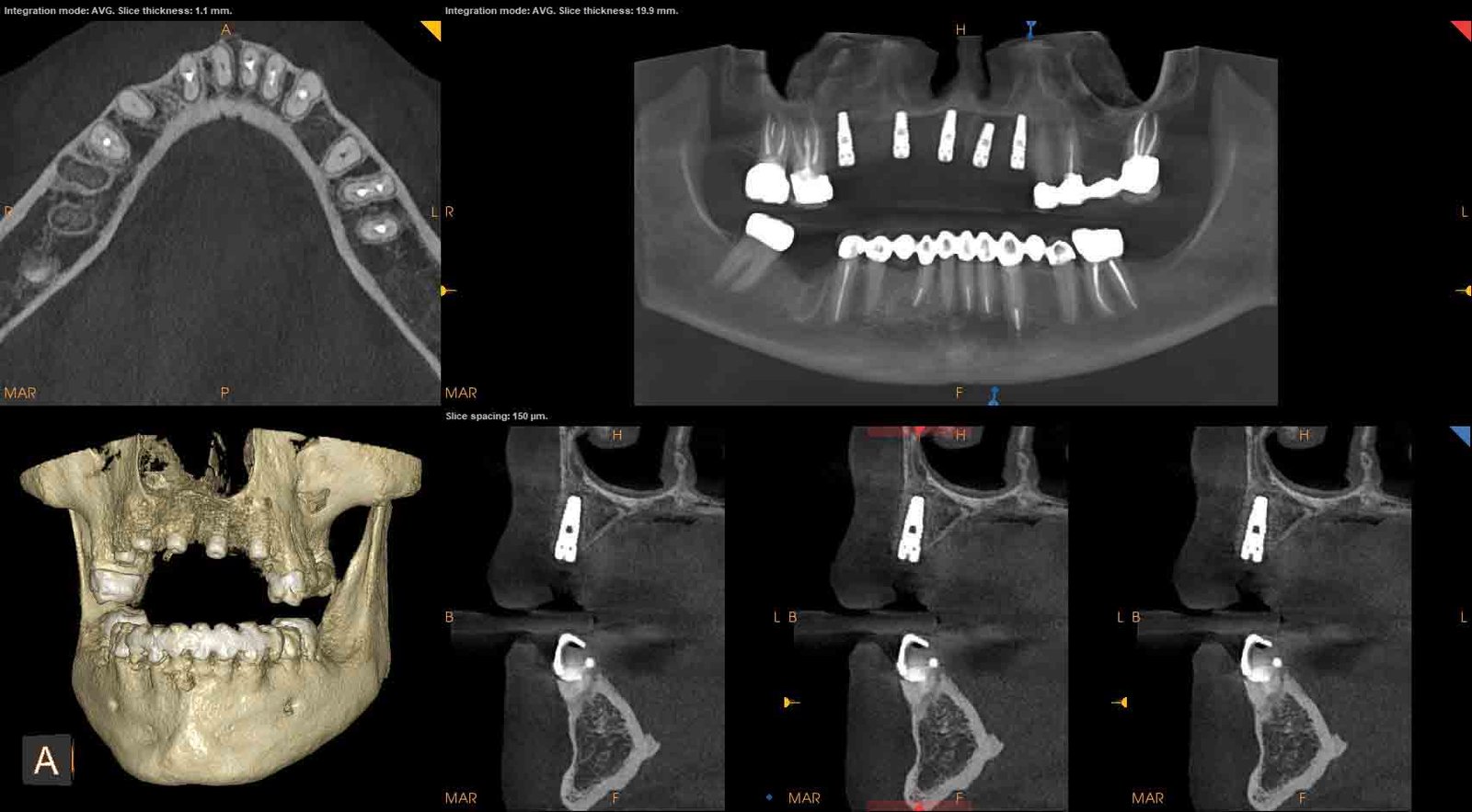
Multiple fields of view give me more options to handle any clinical situation, even capturing the frontal sinus (16 cm x 17 cm). At the same time, I can capture a post-op image using the 4 cm x 4 cm FOV at just slightly more dose than a PA. The metal artifact reduction (MAR) algorithm also significantly reduces metal artifacts to help confirm diagnosis and reduces risk of misinterpretation. As we enter 2019, my team and I are eager to discover even more ways this innovative system can benefits our patients.
No one can say for certain what the future holds for oral surgery, but there’s no doubt the right technology has given me more certainty about the future of my patients’ oral health. As that technology aids with new techniques for better surgery and fuels industry trends, we’re sure to see even more advancements in 2019 that will change the way we practice and, ultimately, change our patients’ lives.
There are always more advancements and trends for 2019 will change the way clinicians practice and, ultimately, change patients’ lives. Dr. Ara Nazarian also shares his insights in his article “Implants and the Spirit of Inventiveness.” Read it here.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



