Editor’s intro
Dr. Matthew Hallas discusses this non-invasive high frequency vibration device that increases bone volume and enhances implant integration. Read about this new adjunctive therapy in implant care.
Dr. Matthew Hallas illustrates a case that utilized a new adjunctive therapy in implant care
In dentistry, we routinely encounter patients requiring implants and restorations where the underlying causes such as disease and improper forces have impacted contributing factors to treatment success. This can often relate to the patients’ bone: loss of bone height, reduced bone density, defects, and tooth mobility. To restore these patients to the desired esthetics and function, we first need to gain control of the disease and improve overall oral health. However, bone quality and tooth mobility remain an on-going challenge.
Recently a new, noninvasive mode of therapy using high-frequency vibration (HFV) has been made available. In preclinical studies, HFV has demonstrated the following abilities:
- to increase bone volume and preserve alveolar bone width and height1
- to significantly increase osteoblasts and fibroblasts in the periodontal ligament (PDL)2
- to enhance the integration of implants3
- to increase naturally produced growth factors — for example, bone morphogenetic protein (BMP), platelet-derived growth factor (PDGF)4
This case study focuses on a patient using the VPro™ (Propel Orthodontics), a noninvasive, high-frequency vibration, oral device with a bite plane used for 5 minutes per day post-extraction to improve bone for future implants, while significantly reducing tooth mobility and improving overall oral health.


Initial presentation
A 60-year-old healthy nonsmoking female presented for surgical and restorative consultation regarding her failing maxillary left dentition. The patient’s chief complaint was fear that a removable dental appliance was her only restorative option due to the extensive breakdown of her teeth. Following an initial discussion, the dentist performed and completed a comprehensive dental examination of her hard and soft tissues that included an occlusal exam, periodontal charting, mobility analysis, and temporomandibular joint evaluation. The patient’s maxillary left quadrant examination revealed vertical root fractures on teeth Nos. 12 and 14 with periapical abscesses, resulting in non-restorability of No. 12-x-14 fixed bridge work (Figures 1 and 2). Additionally, tooth No. 15 presented with a large mesial-occlusal amalgam with distal-occlusal fracture, (+)2 mobility, and a periodontal probing depth range of 3 mm-7 mm. Generalized moderate plaque and calculus accumulations, posterior interproximal food impaction, and generalized bleeding on probing were also noted.
Treatment planning
The patient desired to phase her treatment plan with initial treatment of the maxillary left quadrant followed by completion of the maxillary right quadrant at a future date. The following treatment options were discussed with the patient.

Option 1: Removal of teeth Nos. 12 and 14 with hard tissue augmentation, implant placement at Nos. 12 and 14 sites, implant-supported fixed bridge work with abutments at Nos. 12 and 14, and core buildup tooth No. 15 with a crown.
Option 2: Removal of teeth Nos. 12, 14, and 15 with hard tissue augmentation, implant placement at No. 12 and 14 sites, and implant-supported fixed bridge work with abutments at Nos. 12 and 14.
The first option was chosen with the understanding that following removal of teeth Nos. 12 and 14 and an adequate amount of healing, that there would be a reduction in the amount of probing depths and mobility on tooth No. 15 to support a restoration with a favorable long-term prognosis.
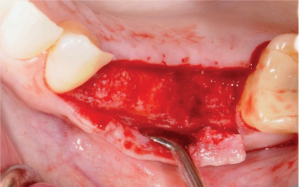
Surgical phase part 1
Extractions with hard tissue augmentation
The patient was premedicated with amoxicillin 500 mg (2 g presurgery followed by 875 mg BID for 7 days, an oral antibacterial rinse (CHG 0.12%), and an NSAID — all starting 1 hour prior to surgery. Local infiltration of the hard and soft tissue in the maxilla was completed at site Nos. 11 through 15 with 2% lidocaine with 1:100,000 epinephrine. Routine dental extractions of teeth Nos. 12 and 14 were completed, and thorough curettage and irrigation of the sites were completed. Maintenance of the buccal plates was accomplished using a minimally traumatic approach. Hard tissue augmentation was completed using a CollaPlug® Absorbable Collagen Wound Dressing (Integra LifeSciences Corp.) technique utilizing creos™ allo.gain corticocancellous 0.25-1.00 mm (Nobel Biocare) and Miltex by Integra HeliPLUG®. Following completion of the procedures, postoperative instructions were given, and a VPro device (Propel Orthodontics) was delivered with instructions to use 5 minutes per day for 8 weeks.
Surgical phase part 2
Implant placement treatment planning
Following 4 months of healing, the patient was re-evaluated for implant placement at site Nos. 12 and 14 (Figures 3 and 4). Clinical examination with cone beam CT was completed and revealed tooth No. 15 presented with 1 mm-4 mm probing depths and no clinical sign of mobility (Figures 5A and 5B). Potential future implant sites Nos. 12 and 14 have adequate soft and hard tissue volume for implant placement as originally treatment planned.

Conclusion
This case demonstrates the VPro high-frequency vibration device helped improve overall oral health by improving blood flow and circulation, while helping maintain quality bone for implants and normalizing mobility. At this phase of treatment, the patient had normalized mobility and normalized probing depths of 1 mm-4 mm.
Tooth mobility remains a challenge in restorative dentistry as well as periodontics. While antibiotics, scaling, planing, or laser treatments can decrease the progress of mobility, they do not usually improve the existing mobility.5 In studies, high-frequency vibration has demonstrated a significant increase in biological activity in growth factors4 and a substantial increase in fibroblast PDL.2 It is hypothesized that this stimulation of PDL fibroblasts, along with improved bone volume and density, leads to a stabilizing of mobile teeth.6
The effects of HFV on bone has been extensively studied in orthopedics and orthodontics.7 These data show the HFV has an anabolic effect through activation of osteoblasts to stimulate bone growth and improve bone density.2,8 High-frequency vibration has also been demonstrated to relieve oral pain and improve blood flow to tissues.4,9,10
The HFV VPro device is noninvasive, requires only 5 minutes of daily use at home, and provides a phone app for tracking usage, which can help overall patient compliance.
While only a case study and more studies are needed, high-frequency vibration may offer a new adjunctive therapy in implant care and a new primary treatment for mobile teeth.
Editor’s call to action
High frequency vibration is an innovative tool for implant therapy. Read Dr. Komal Suri’s article, “Managing the failing dentition” for more insights into dealing with an aged dentition with multiple restorations. It’s also a CE, so our subscribers can take the quiz and receive 2 credits!
https://implantpracticeus.com/ce-articles/managing-the-failing-dentition/.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Matthew Hallas, DMD, joined Bay Lakes Center for Complex Dentistry after several years working with University Associates in Dentistry in Chicago, Illinois. His extensive training in the specialty of prosthodontics gives him advanced skills and knowledge of the latest technologies and utilization of dental materials, including all ceramic restorations, CAD/CAM restorations, and computer-guided implant surgery. Additionally, Dr. Hallas is an active lecturer for dental study groups and continuing education programs, which keeps him on the leading edge of new developments in the field of prosthodontics.
Matthew Hallas, DMD, joined Bay Lakes Center for Complex Dentistry after several years working with University Associates in Dentistry in Chicago, Illinois. His extensive training in the specialty of prosthodontics gives him advanced skills and knowledge of the latest technologies and utilization of dental materials, including all ceramic restorations, CAD/CAM restorations, and computer-guided implant surgery. Additionally, Dr. Hallas is an active lecturer for dental study groups and continuing education programs, which keeps him on the leading edge of new developments in the field of prosthodontics.

