Drs. Lanka Mahesh, Gregori M. Kurtzman, and colleagues discuss the potential for a tooth-derived bone graft.
Drs. Lanka Mahesh, Gregori M. Kurtzman, Varun Raj Kumar, Anshi Jain, Saurabh Juneja, and Yuvika Raj Kumar discuss the efficacy of human extracted teeth as an alternative
Abstract
Objective
To test the efficacy of human extracted tooth for use as bone graft material as an alternate to other synthetic, allogenic, or xenogenic bone graft materials.
Study design
Freshly extracted teeth were cleaned of all debris and calculus and were placed in a “smart dentin grinder,” which is a device used to grind and sort extracted teeth into a specific-sized dentin particulate. Dentin particulate material was then placed in surgical sites to be used as graft material and were tested histologically.
Results
Histological analysis showed the presence of remaining graft material and forming dentin around graft material. Section further revealed the formation of lamellar bone around the dentin surface. Lamellar bone showed the presence of plump osteoblastic rimming, entrapped osteocytes in lacunae. Different stages of mineralization also were evident in our case where dentin was placed as a bone graft material.
Conclusion
Though there is still insufficient data regarding use of extracted teeth for bone grafting, it may be considered as a useful biomaterial and an alternative to synthetic, allogenic, or xenogenic bone grafts for socket preservation, and filling other bony defects. It is autogenous, clinically safe, shows no adverse reactions, and has good bone regeneration potential.
Introduction
A variety of materials have been commercialized for use in different treatment procedures in maxillofacial, periodontal, and dental implant surgery. In particular, bone grafts are used to stabilize blood clotting, increase alveolar bone volume, and restore its original volumetric structure, function, and appearance. A range of biomaterials have been developed for grafting and bone regeneration as alternatives to autogenous bone grafts. These offer good osteoinductive and osteoconductive capacities but suffer some risk of negative host response. Synthetic materials are an alternative graft material that offers osteoconductive capacities and can be supplied in unlimited quantities.1 Alternative graft materials, including allografts, xenografts, and alloplastic bone grafts, are clinically used, but they have disadvantages such as lacking osteoproliferation and having high-material cost and limited osteoinductivity.2 Therefore, development of an alternative graft material that surpasses all these limitations is desired.
Recently, bone graft materials using permanent teeth from the patient receiving the graft, which has been processed, have come to light. Clinical and histological outcomes of this autogenous tooth-derived graft material have been confirmed by some studies. Tooth components are very similar to alveolar bone components, which has led to consideration as a bone graft material using the organic and inorganic components of extracted teeth.3 Additionally, since they are derived from the patient, all potential for autoimmune-type reactions to the graft material are eliminated.
Extractions are one of the most widely performed procedures in dentistry, yielding teeth that are discarded as clinical waste. But teeth could be recycled to produce an effective graft material. Dentists have been transplanting teeth for many years, and tooth ankylosis is a well-studied principle.4 In recent years, several research teams have assessed the potential uses of extracted teeth.5,6
Autogenous dental bone graft material, a human demineralized dentin matrix derived from extracted human teeth, was first developed in 2008, and its osteoinductive, osteoconductive, and remodeling capacities in implant dentistry have been evaluated.7
Methodology
Freshly extracted teeth were taken and were processed into a bacteria-free particulate autogenous mineralized dentin for immediate grafting into that same patient who had just undergone the extraction. A Smart Dentin Grinder (KometaBio, Fort Lee, New Jersey) was devised, which is utilized to grind extracted teeth into a specific-sized dentin particulate. A chemical cleanser is then applied to process the dentin particulate into a bacteria-free graft during a 15-20 minute time frame. This novel procedure is indicated mainly in cases when teeth are extracted because of periodontal reasons or when impacted teeth require extraction. Teeth that have undergone root canal treatment should not be employed in this procedure because the obturation material present may lead to foreign material contamination of the resulting graft material. On the other hand, if teeth have crowns present, the restoration can be removed prior to processing, and direct filling materials such as amalgam or composite can be ground out of the tooth prior to processing.6 The teeth are extracted atraumatically to maintain integrity of the socket (Figure 1). Any restorative materials are removed from the extracted teeth with a handpiece and burs in preparation for processing the dentin (Figure 2).
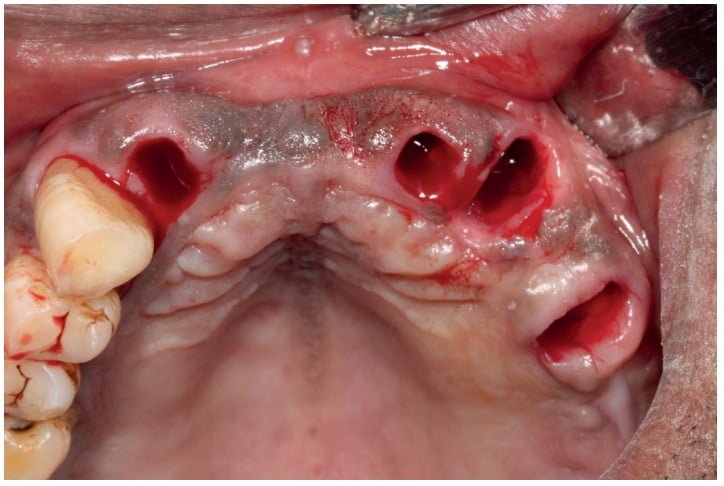
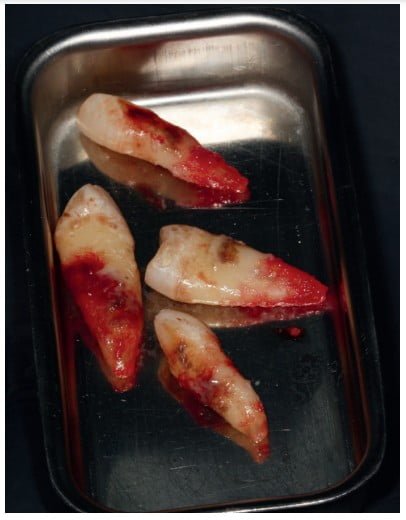

The teeth are then processed to create dentin particles and hydrated appropriately (Figure 3). The area at the sites to receive the dentin grafting is flapped to expose the sockets (Figure 4). Immediate implant placement was planned, and the osteotomies were created. Ground dentin particulate was placed into the osteotomies and extraction sockets that would not receive implants, and implants were placed into the planned sites (Figures 5 and 6). The flap was repositioned to cover the area with primary closure of the soft tissue, and sutures were placed (Figure 7). The patient was recalled after 3 months to check osteointegration of the implants, and the socket grafting was evaluated. The area was flapped and a core sample taken at the previously grafted sockets with a trephine for histological analysis of the dentin graft material.


Histological analysis
After the process of implant placement, histological analysis was done in which the specimens were fixed with 4% paraformaldehyde in 0.1M PBS (pH 7.4), and decalcified in 0.5M EDTA (pH7.8) for 10 days. After decalcification, each specimen was transversally divided into two blocks, exactly along the center of the original surgical defect, processed, and embedded in paraffin. Then transverse serial sections of 5 µm thickness were prepared. The sections were stained with hematoxylin and eosin (HE) and showed the presence of remaining graft material and forming dentin around graft material (Figure 8). The section further revealed the formation of lamellar bone around the dentin surface. Lamellar bone showed the presence of plump osteoblastic rimming, entrapped osteocytes in lacunae (Figure 9). Different stages of mineralization were also evident in the case where dentin was placed as a bone graft material. The stroma is fibrovascular in nature with very mild chronic inflammatory reaction in the background. Special stains, including eosin (HE) methylene blue and aldehyde fuchsin, were also performed, which showed the presence of resorbing graft material and forming dentin (Figures 10 and 11).


Discussion
Bone and dentin resemble each other in composition and mechanism of formation. In addition to major levels of Type I collagen, both tissues contain non-collagenous proteins (NCPs). The NCPs are believed to play key biological roles in osteogenesis and dentinogenesis. Among these NCPs, dentin phosphoprotein (DPP) and dentin sialo-protein (DSP) have been thought to be uniquely involved in dentinogenesis. In dentin extracellular matrix, Type I collagen is the most abundant organic constituent, while DPP is the second-most plentiful protein. The most unusual feature of DPP is the occurrence of large amounts of aspartic acid (Asp) and phosphoserine (Pse) largely present in repeating sequences of (Asp-Pse-Pse)n and (Asp-Pse)n. These repeating sequences assume extended backbone structures with relatively long ridges of carboxylate and phosphate groups on each side of the peptide backbone7 (dentin). Autogenous bone grafting is the gold standard for bone augmentation because of its excellent osteoinductivity and osteoconductivity, but it has some impediments such as limited availability, donor site morbidity, and also high-resorption rates of up to 50%.8
In particular, bone grafts are used to stabilize blood clotting, increase alveolar bone volume, and restore its original volumetric structure, function, and appearance.
The osteogenic capacity of a demineralized tooth was verified as early as 1967,9 and was first introduced by R&D Institute Korea Tooth Bank (Seoul, Korea). The tooth graft has satisfied many clinicians and patients for its osteoconduction as well as osteoinduction capacity. Nampo, et al.,5 reported that dentin, when used as a bone graft, promotes bone formation as it contains proteins such as osteopontin (OPN). On immunohistochemical staining with anti-DSP antibody, the positive reaction was localized to the dentin of the extracted tooth fragments incorporated into the new bone at 6 weeks, suggesting that dentin has a high affinity for and marked osteoconductive effect on jawbone. The structure and composition of dentin are similar to that of bone, consisting of collagen (20%), hydroxyapatite (70%), and body fluid (10%) in weight; and having a significant osteoconductivity. Furthermore, dentin matrix has some osteoinductivity because it contains BMPs. Thus, dentin or dentin matrix is expected to serve as a bone substitute. Some studies have shown that mineralized dentin matrix possesses excellent biocompatibility. However, it was also observed that the dentin matrix promoted the formation of a more homogenous and uniform trabecular bone in the three-thirds of the dental socket during the 15-day and 30-day periods of healing, characterizing its osteoconductive property in dental socket repair.8 Therefore, dentin tooth can be classified into three groups according to the degree of demineralization: undemineralized dentin (UDD), partially demineralized dentin matrix (PDDM) (70% decalcified), and demineralized dentin matrix (DDM). It has been shown that UDD is less effective in bone formation, whereas other studies have shown that DDM is biocompatible and also osteoinductive, similar to demineralized bone matrix.10
In tooth-based graft materials, there are higher mineralization and crystallinity when compared with bone. However, tooth demineralization is time-consuming (usually 2 to 6 days), thus limiting the use of fresh demineralized tooth (FDT) as a graft material. Nevertheless, FDT has shown great potential in alveolar bone regeneration. In an animal study performed by Al-Asfour, et al.,11 human dentin graft was compared with tibia bone graft. The authors reported that demineralized xenogenic dentin onlay grafts showed similar resorption characteristics as autogenous bone onlay grafts, being resorbed in a similar rate during 12 weeks. This is in contrast with Zitzmann, et al., who reported a remaining amount of Bio-Oss® (Geistlich Pharma North America Inc.) of 37% at 6 months after grafting Bio-Oss.12 Moreover, in the study done by Kim, et al., autogenous teeth (AutoBT) showed gradual resorption during the first three months. At 6 months, new bone was replaced with trabecular bone with resorption of most graft material.13 Osteoinduction and osteoconduction were observed, which were similar to the histologic analysis of other’s papers.14,15,16
Conclusion
Although there is still insufficient data regarding use of extracted teeth for bone grafting, it may be considered as a useful biomaterial and alternative to synthetic, allogenic, or xenogenic bone grafts for socket preservation and filling other bony defects. Being autogenous, it is clinically safe, shows no adverse reactions, and has a good bone regeneration potential.
Dr. Armin Nedjat discussed a tooth-derived bone graft as an effective grafting material in “Autologous bone grafting using extracted teeth.” Read it at: https://implantpracticeus.com/ce-articles/autologous-bone-grafting-using-extracted-teeth/
- Calvo-Guirado JL, Pino PC, Sapoznikov L, et al. A new procedure for processing extracted teeth for immediate grafting in post extraction sockets. An experimental study in American Fox Hound dogs. Ann Anat. 2018;217:14-23.
- Koga T, Minamizato T, Kawai Y, et al. Bone Regeneration Using Dentin Matrix Depends on the Degree of Demineralization and Particle Size. PLoS One. 2016;11(1):e0147235.
- Vaqués PG, Yanes CP, Devesa AE, et al. Autogenous teeth used for bone grafting: A systematic review. Med Oral Patol Oral Cir Bucal. 2018;23(1):e112-e119.
- Pape HD, Heiss R. Zur Geschichte der Zahntransplantation [History of tooth transplantation]. Fortschr Kiefer Gesichtschir. 1976;20:121-125.
- Nampo T, Watahiki J, Enomoto A, et al. A new method for alveolar bone repair using extracted teeth for the graft material. J Periodontol. 2010;81(19):1264-1272.
- Kuperschlag A, Keršyte G, Kurtzman GM, Horowitz RA. Autogenous Dentin Grafting of Osseous Defects Distal to Mandibular Second Molars After Extraction of Impacted Third Molars. Compend Contin Educ Dent. 2020;41(2):76-83.
- Yeomans JD, Urist MR. Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues. Arch Oral Biol. 1967;12(8):999-1008.
- Calvo-Guirado JL, Sánchez de Val JEM, Oltra MLR, Martínez CPA, Fernández MPR, Gosálvez MM. The Use of Tooth Particles as a Biomaterial in Post-Extraction Sockets. Experimental Study in Dogs. J. 2018;6:12-22.
- Urist MR. Bone: Formation by autoinduction. 1965;150(3698):893-899.
- Qin C, Brunn JC, Cadena E, et al. The expression of dentin sialophosphoprotein gene in bone. J Dent Res. 2002;81(6):392-394.
- Al-Asfour A, Farzad P, Al-Musawi A, Dahlin C, Andersson L. Demineralized Xenogenic Dentin and Autogenous Bone as Onlay Grafts to Rabbit Tibia. Implant Dentistry. 2017;26(2):232-237.
- Zitzmann NU, Sharer P, Marinello CP, Schupbach P, Berglundh T. Alveolar ridge augmentation with Bio-Oss: a histologic study in humans. Int J Periodontics Restorative Dent. 2001;21(3):288-295.
- Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, Kim SY. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(4):496-503.
- Gomes MF, de Abreu PP, Morosolli ARC, Araújo MM, Goulart MDGV. Densitometric analysis of the autogenous demineralized dentin matrix on the dental socket wound healing process in humans. Braz Oral Res. 2006;20(4):324-30.
- Binderman I, Hallel G, Nardy C, Yaffe A, Sapoznikov L. A Novel Procedure to Process Extracted Teeth for Immediate Grafting of Autogenous Dentin. J Interdiscipl Med Dent Sci. 2014;2:6.
- Reddy GV, Abhinav A, Malgikar S, et al. Clinical and Radiographic Evaluation of Autogenous Dentin Graft and Demineralized Freeze Dried Bone Allograft with Chorion Membrane in the Treatment of Grade II and III Furcation Defects‑: A Randomized Controlled Trial. Indian Journal of Dental Sciences. 2019;11(2):83-89.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



