Drs. Filip Ambrosio and Gregori M. Kurtzman illustrate their full arch treatment implant protocol with an implant that helps maintain the crestal bone.
Drs. Filip Ambrosio and Gregori M. Kurtzman discuss achieving osseocompression and improving bone density during implant procedures
Introduction
Full-arch implant prosthetics, referred to as “All-on-X,” have become a common option for treating either the edentulous arch or an arch that will be edentulous due to a failing remaining dentition. The goal typically is immediate provisionalization of the implants to provide a stable prosthesis during the integration phase and to not require the patient to wear a removal denture that may have minimal retention. With that in mind, selection of the implant would ideally utilize a design with deep aggressive threads. This will help to achieve osseocompression, thereby improving bone density around the implants when utilized in the less dense bone found in the maxilla. When employed in the more dense bone of the mandible, the aggressive threads of the implant create a self-tapping effect, making insertion into the osteotomy easier. It is commonly accepted and supported by the literature that when insertion torque of 35 Ncm or greater is achieved, implants can be immediately loaded with a provisional hybrid prosthesis during the initial healing and osseointegration phase of treatment.1
A systematic review and meta-analysis of clinical success when higher insertion torque can be achieved showed no deleterious effect on implant survival rate or marginal bone loss.2 Overall implant survival has been reported up to 98% when the critical minimum insertion torque is achieved when immediately loading the provisional prosthetics.3,4 When four to eight implants are immediately loaded in the arch, and the accepted minimum insertion torque is achievable, a very high-clinical success has been reported.5,6
Selection of the implant
Selection of the implant may have an effect on the overall clinical success, especially when immediate loading is required. As previously mentioned, thread design on the implant has an effect on initial stability and is correleated to bone density at time of placement. The Ditron Ultimate Precision Implant (ULT™) is designed with double stressless sharp threads (DSST), which generate gentle progressive vertical and horizontal bone compaction upon insertion into the osteotomy (Figure 1A). This enhances initial implant stability regardless of the quality of bone present while preserving the bone vascularity.7

The authors recommend in lower dentisty maxilla that the osteotomy diameter be underprepared so that the implant creates osseocompression, thereby densifying adjacent bone. For example, when the planned implant is 4.2 mm in diameter in Type III or IV bone (D3 or D4), the final drill diameter will be 3.2 mm drilled to the prescribed depth of the implant being placed. In Type I or II bone (D1 or D2), the final drill diameter utilized will be 3.8 mm In some instances, based on the bone type, the final drill may not go to depth. Additionally, the apical aspect of the implant plays a factor on how the subsequent threads interact with the bone as the implant is threaded into the osteotomy. Helical apico-coronal slots (HACS) are present along the length of the implant from below the micro-grooves to the apex. These slots help reduce resistance with the osseous walls of the osteotomy during insertion, allowing for collection of blood and bone chips from the osteotomy. These are drawn up, coating the surface of the implant, thereby creating a scaffold or matrix to accelerate osteoconduction during the initial phase of healing. The ULT implant has a cutting apex edge with progressive thread and sharp apical blades. Depending on the bone type and quality, this will act as a self-drilling, self-tapping feature to the implant design. The rounded apex itself improves ease of insertion, allowing mild directional refinement during the initial insertion of the implant into the osteotomy.
Maintenance of the crestal bone is important to the long-term success of the implant. Under function, the majority of loading occurs at the crestal portion of the implant.8 So, the thicker this bone is around the implant, the better the load handling and preservation of this critical bone over time. Frequently, the thin buccal crestal aspect of bone adjacent to the implant resorbs, which may contribute to soft tissue recession and resultant esthetic compromise. Given time, this may progress to peri-implantitis and compromise the health of the implant. So, the thicker the bone is at crest on the buccal/palatal dimension and between implants or the implant and adjacent natural teeth, the easier it is to preserve that critical crestal bone long-term.9
With this in mind, the ULT implant is designed with a slight platform switch at bone level or slightly subcrestal upon placement. But in addition, the reverse concave neck (RCN) provides what has been termed bone platform switching,10 a narrowed concave neck strategy to preserve additional marginal bone beyond the platform switch (Figure 1B). Enhanced bone volume at the cervical not only helps provide for greater resistance to bone resorption, but also reduces overall stress on the crestal cortex (Figure 2). Less titanium at the crest also helps to prevent removal of delicate marginal and subpapillary bone, providing the vascularity necessary for preservation of the peri-implant soft tissue.10
The combined strategy of platform switch and platform bone switch optimizes resistance to bone resorption, thereby stabilizing both hard and soft tissue elements.
Interestingly, the addition of microgrooves within the reverse concave neck provide a third bone preservation strategy, even as it serves a favorable biomechanical purpose to increase implant surface area to reduce stress and promote maintenance of crestal bone under functional loading.11
Case report
A 49-year-old female patient presented with the chief complaint of her inability to wear her current full maxillary and mandibular dentures due to a significant gagging reflex, indicating the dentures were delivered 2 years previously. She also expressed dissatisfaction with the current esthetics of the prosthesis and her smile. The patient’s general dentist had referred her for an implant consultation. Her medical history was reviewed, and no significant health issues were disclosed.
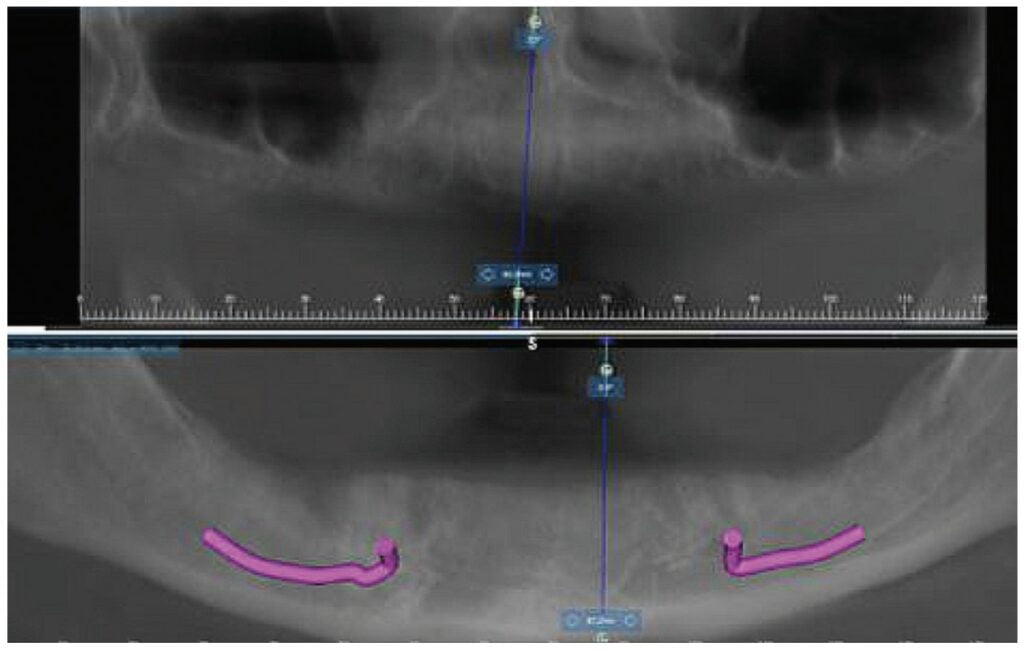
A CBCT scan was taken and panoramic views of the maxilla and mandible evaluated (Figure 3). Bilateral pneumatization of the maxillary sinus was noted, but adequate bone height was present between the premolars for implant placement to support an All-on-X hybrid prosthesis. In the mandibular arch, sufficient height was available between the mental foramen bilaterally and over the inferior alveolar nerve for implant placement to also support an All-on-X fixed hybrid prosthesis. A discussion was held with the patient that implants could be placed in both arches that would allow restoration with fixed prosthetics. Should sufficient insertion torque be achieved at the time of implant placement, a screw-retained hybrid provisional prosthesis would be placed and worn for several months during healing after which a final prosthesis would be fabricated. The patient would also be able to do a “trial-run” of the esthetics with the provisional prosthesis, with any requested modifications made when the final prosthesis was designed and fabricated. The treatment plan included six implants in each arch to support the planned hybrid prostheses. The patient was informed that reduction of the crestal bone would be required to achieve a flat ridge for adaptation of the prosthesis to the ridge as well as to provide adequate interarch space for the final prosthesis. The patient accepted the treatment plan. An intraoral scan of the arches was performed with Medit i500 (Medit Corp, Seoul, Korea) as well as the current complete arch maxillary and mandibular dentures (Figure 4). The patient was dismissed and scheduled for the surgical appointment.

The scans were imported into the planning software (RealGUIDE™, Allston, Massachusetts) and merged with the CBCT scan to allow implant planning. The maxillary arch was planned for implants at six sites, including tilted implants mesial to the maxillary sinus bilaterally to avoid the need for sinus augmentation and allow more distal placement of the implant platform for a better anterior/posterior (A-P) spread (Figure 5A). ULT implants were planned as follows: No. 3 (3.75 x 11.5 mm), No. 6 (3.75 x 11.5 mm), No. 8 (3.75 x 11.5 mm), No. 9 (3.75 x 11.5 mm), No. 11 (3.75 x 11.5 mm), and No. 14 (3.75 x 11.5 mm) (Figure 5B).

The mandibular arch was then planned for seven possible implants with the extra implant beyond what was initially planned should the short posterior implant on the patient’s left have less than ideal initial stability to provide better stability of the provisional prosthesis (Figure 6A). Ditron Dental ULT implants were planned as follows: No. 19 (3.75 x 11.5 mm), No. 20 (3.75 x 11.5 mm), No. 22 (3.75 x 11.5 mm), No. 24 (3.75 x 11.5 mm), No. 25 (3.75 x 11.5 mm), No. 27 (3.75 mm x 10 mm), and No. 30 (3.75 x 11.5 mm) (Figure 6B). A replica of the current dentures was fabricated to be used as a surgical guide, and the center of the replica was removed with a lab bur to create a zone for the implants to emerge to ensure they would be within the proper prosthetic zone (Figure 7).
The patient presented for surgery, and the consent form was reviewed and signed. IV sedation was initiated, and local anesthetic (2% Lidocaine with 1:100,000 epi) was administered in both arches. A crestal incision was made in the maxillary arch midcrest, and a full thickness flap was elevated to expose the buccal and palatal aspects of the ridge. Evaluation of the osseous ridge noted it was fairly flat, and reduction was deemed to be not necessary. The surgical guide was inserted and utilized to guide the location of the osteotomies. ULT implants were placed at the six planned sites: No. 3 (3.75 mm x 13 mm), No. 6 (3.75 mm x 10 mm), No. 8 (3.75 mm x 10 mm), No. 9 (3.75 mm x 11.5 mm), No. 11 (3.75 mm x 10 mm) and No. 14 (3.75 mm x 13 mm). Insertion torque of greater than 40 Ncm was achievable at five of the sites with site No. 10 being less than 30 Ncm and insufficient to support an immediate load. As sufficient A-P distance and adequate insertion torque was present utilizing the five other maxillary implants, it was decided to place an immediate provisional hybrid prosthesis. Multi-unit abutments (MUAs) with the following angulations were placed: (No. 3 = 30 degrees, No. 6= 17 degrees, No. 8= 0 degrees, 11 = 17 degrees, and No. 14 = 30 degrees). The soft tissue was repositioned around the MUAs, and primary closure was achieved utilizing a continuous polylactic acid (PLA) suture.
A scalpel was then utilized to create a crestal incision in the mandible from the approximate first molar on the right to the approximate first molar on the left, and a full thickness flap was elevated with identification of the mental nerve and its foramen bilaterally. As with the maxillary arch, the mandibular crestal bone was fairly flat, and ridge reduction was not needed. The surgical guide was inserted in the mandible and utilized to guide the location of the osteotomies. ULT implants were placed at six sites as: No. 20 (3.75 mm x 10mm), No. 22 (3.75 mm x 10m m), No. 24 (3.75 mm x 11.5 mm), No. 25 (3.75 mm x11.5 mm), No. 27 (3.75 mm x 10 mm) and No. 30 (3.75 mm x 10 mm). Insertion torque of greater than 40 Ncm was achievable at all of the sites. As sufficient adequate insertion torque was present, placement of an immediate provisional hybrid prosthesis was planned. MUAs with the following angulations were placed (No. 20 = 30 degrees, No. 22 = 0 degrees, No. 24 = 0 degrees, No. 25 = 0 degrees, No 27 = 0 degrees, and No. 30 = 0 degrees). The soft tissue was repositioned around the MUAs, and white protective caps were placed onto the MUAs. Primary closure was achieved, and a continuous PLA suture placed. The patients’ dentures were relieved to seat over the white caps, and a reline impression was taken with the two arches in occlusion to allow use of the current vertical dimension of occlusion (VDO) in the planned fabrication of the provisional hybrid restorations. The patient was dismissed and scheduled for postoperative check and suture removal in 2 weeks.
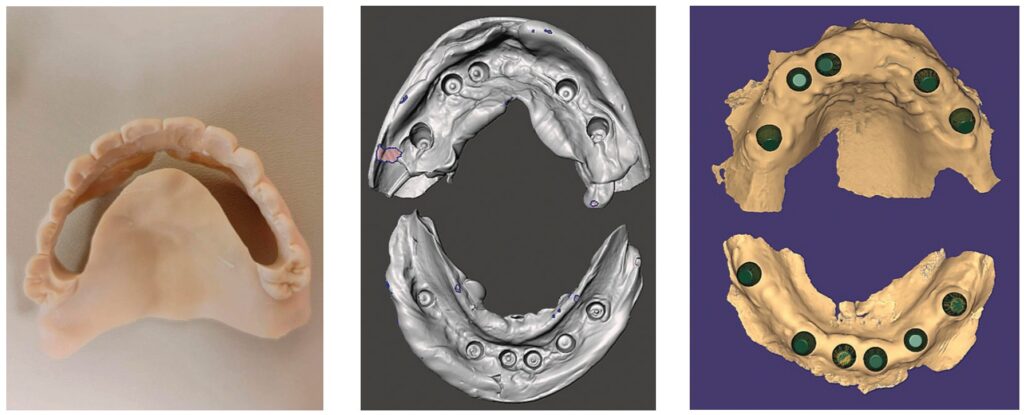
The tissue side of the impressions was scanned (Figure 8). The scan data was imported into the software (exocad), while the patient remained in the treatment operatory (Figure 9). Utilizing the planned implant positions, the information was merged, and analogs were added to the virtual models of the white protective cap scans. The scans of the current dentures with modifications to increase the VDO were added as well as projections for emergence of the screw access channels through the virtual prosthesis. The model was then removed virtually (Figure 10). The planned provisional hybrid prostheses were evaluated for esthetics and alignment of the midline in relation to the arches. The flange area was modified to convert the virtual prosthesis from a denture to a hybrid prosthesis (Figure 11). The virtual designed provisional hybrid prostheses were printed utilizing Flexcera™ Smile resin (Desktop Health™, Newport Beach, California) with the EnvisionOne 3D printer (Desktop Health™).


The patient returned 2 weeks later to evaluate healing and for suture removal. She indicated general comfort during the initial healing period. Sutures were removed with slight bleeding noted related to the sutures, and soft tissue did not present with any significant inflammation. The printed immediate provisional prostheses were placed onto each arch and secured with the prosthetic screws to fixate them to the MUAs, and a panoramic radiograph was taken to verify seating of the prostheses and document the implants in relation to the anatomy (Figure 12). The occlusion on the provisional prostheses was checked and minor adjustments made intraorally for a more even occlusion upon occluding the arches. The patient was shown her provisional smile and indicated that she was satisfied with the initial esthetics (Figure 13).

The patient presented after 12 months of integration to initiate fabrication of the final prostheses. A discussion occurred with the patient regarding the unloaded implant at site No. 10, where she expressed her anxiety regarding further surgery and asked if the case could be finalized on just the five implants in the arch as it “seemed” to be working with the provisional restoration. As the provisional was stable on the five implants and taking into account the patient’s desire not to have additional surgery to uncover the buried implant, the plan was modified to fabricate the prosthesis on the currently loaded implants in the maxilla. During further discussions with the patient regarding the esthetics of the provisional prostheses, she expressed that she wanted larger anterior teeth and that the current tooth shape was too rounded for her. She requested that a more square-shaped anterior tooth be used. That information was communicated with the lab to modify the final prostheses. The lab modified the design virturally in the software and then milled the final monolithic zirconia hybrid prostheses for both arches.

The patient returned for insertion of the final monolithic zirconia hybrid prostheses. The provisional restorations were removed, and minimal superfical inflammation was noted at the crestal top, which was felt to be due to the patient’s homecare (Figures 14 and 15). Additional instruction on homecare under the prostheses would be given the patient at the end of the appointment after the final prostheses were inserted. The final monolithis zirconia hybrid prostheses were inserted, and the MUA prosthetic screws were hand tightened. A piece of teflon tape was placed into each screw access hole, and the hole was sealed with flowable composite (Figures 16 and 17). Occlusion was checked, and no adjustments were noted to be needed. After the patient was shown her teeth in a mirror, she expressed that she was more satisified with the smile on the final prostheses. She said her smile appeared the way she remembered before the loss of her natural dentition (Figure 18). A panoramic radiograph was taken to document the final clinical results and verify complete seating of the prostheses on the implants in both arches (Figure 19).

Conclusion
Implant treatment of the edentulous arch has challenges. Ideally the plan is to immediately load the implant, which requires achieving implant insertion torque that is at or greater than the accepted value of 35 Ncm. Selection of the implant being utilized plays a factor in achieving that desired insertion torque. The selected implant needs to have an aggressive thread to better engage the bony walls of the osteotomy and create osseocompression in less dense bone to improve bone-to-implant contact (BIC) and initial implant stability.7 The platform switch and bone platform switching achieved with the reverse concave neck of the Ditron Dental Ultimate Precision Implant permits added bone volume at the crestal aspect which is critical to maintain marginal bone, vascularity, and support for the peri-implant soft tissue under functional loading.
Read more about full arch treatment and improving facial esthetics by Dr. Paul Lipton by clicking this link: https://implantpracticeus.com/full-arch-implant-restoration/
- Alfadda SA, Chvartszaid D, Tulbah HI, Finer Y. Immediate versus conventional loading of mandibular implant-supported fixed prostheses in edentulous patients: 10-year report of a randomised controlled trial. Int J Oral Implantol (Berl). 2019;12(4):431-446.
- Lemos CAA, Verri FR, de Oliveira Neto OB, et al. Clinical effect of the high insertion torque on dental implants: A systematic review and meta-analysis. J Prosthet Dent. 2021;126(4):490-496.
- Eckert SE, Hueler G, Sandler N, Elkattah R, McNeil DC. Immediately Loaded Fixed Full-Arch Implant-Retained Prosthesis: Clinical Analysis When Using a Moderate Insertion Torque. Int J Oral Maxillofac Implants. 2019;34(3):737-744.
- Caramês JMM, Marques DNDS, Caramês GB, Francisco HCO, Vieira FA. Implant Survival in Immediately Loaded Full-Arch Rehabilitations Following an Anatomical Classification System — A Retrospective Study in 1200 Edentulous Jaws. J Clin Med. 2021;10(21):5167.
- Meloni SM, Tallarico M, Pisano M, Xhanari E, Canullo L. Immediate Loading of Fixed Complete Denture Prosthesis Supported by 4-8 Implants Placed Using Guided Surgery: A 5-Year Prospective Study on 66 Patients with 356 Implants. Clin Implant Dent Relat Res. 2017;19(1):195-206.
- Slutzkey GS, Cohen O, Chaushu L, et al. Immediate Maxillary Full-Arch Rehabilitation of Periodontal Patients with Terminal Dentition Using Tilted Implants and Bone Augmentation: A 5-Year Retrospective Cohort Study. J Clin Med. 2022;11(10):2902.
- Greenberg A, Romanos GE. Effect of primary stability on short vs. conventional Ditron implants, of Perio Stony Brook University Poster Presentation AO; 2022
- Oliveira H, Brizuela Velasco A, Ríos-Santos JV, et al. Effect of Different Implant Designs on Strain and Stress Distribution under Non-Axial Loading: A Three-Dimensional Finite Element Analysis. Int J Environ Res Public Health. 2020;17(13):4738.
- Patil SM, Deshpande AS, Bhalerao RR, Metkari SB, Patil PM. A three-dimensional finite element analysis of the influence of varying implant crest module designs on the stress distribution to the bone. Dent Res J (Isfahan). 2019;16(3):145-152.
- Carinci F, Brunelli G, Danza M. Platform Switching and Bone Platform Switching. J Oral Implant. 2009;35(5):245-250.
- Yalçın M, Kaya B, Laçin N, Arı E. Three-Dimensional Finite Element Analysis of the Effect of Endosteal Implants with Different Macro Designs on Stress Distribution in Different Bone Qualities. Int J Oral Maxillofac Implants. 2019;34(3):e43–e50.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



