Dr. Sarah Balaster talks about two products that can help dentists bring advanced techniques into their practices — lasers and dry mouth solutions.

Dr. Sarah Balaster discusses solutions that support patients’ oral health and quality of life
As the prevalence of dental implants continues to rise, so too does the occurrence of complications such as peri-implant mucositis and peri-implantitis. Addressing these challenges requires patient-focused, innovative solutions. Laser-assisted protocols, such as LANAP® (Laser-Assisted New Attachment Procedure) and LAPIP™ (Laser-Assisted Peri-Implantitis Protocol), provide minimally invasive, effective treatments to reverse peri-implant disease and periodontal conditions. By integrating these advanced techniques, dental professionals can not only treat ailing and failing implants but also differentiate their practices in a competitive market by offering high-quality care that supports long-term implant success.
Laser precision: elevating implantology with minimally invasive technology
More than 3 million Americans currently have dental implants, and that number is growing by approximately 500,000 each year.1 However, this growth is accompanied by a corresponding increase in complications, such as peri-implant mucositis and peri-implantitis. Notably, 80% of patients and 50% of implants will develop peri-implant mucositis, while up to 56% of patients and 43% of implants will experience peri-implantitis.2 This growing issue underscores the urgent need for patient-focused solutions and advanced protocols that not only address these complications but also establish a foundation for long-term success in dental implant cases.
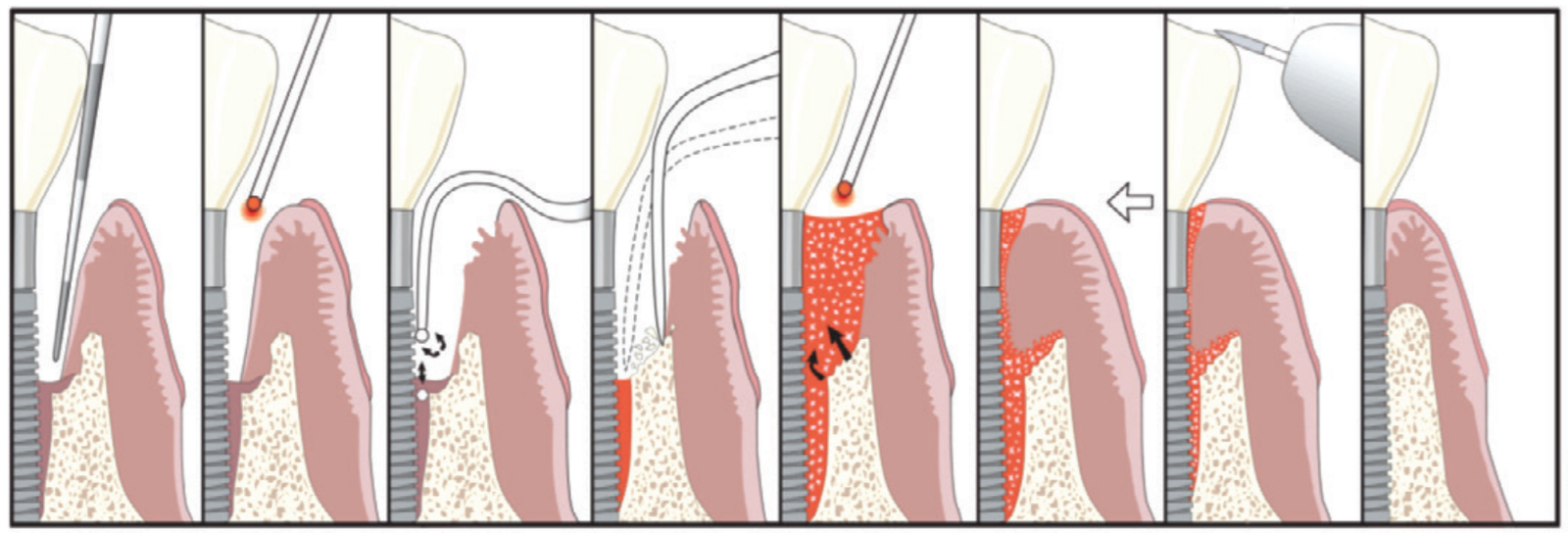
Advanced techniques such as laser-assisted protocols like LANAP®, a patented method for treating periodontal disease (Figure 1) and LAPIP™, which adapts LANAP techniques to address peri-implantitis (Figure 2), offer minimally invasive solutions to reverse these conditions and improve patient outcomes. By integrating these innovative protocols, dental professionals can effectively treat ailing and failing implants, reverse periodontal disease, and advance the standard of care with patient-friendly and minimally invasive surgery.

The power of protocols
The patented LANAP and LAPIP protocols were developed to provide effective treatment options for periodontal disease and peri-implant disease, respectively. To optimize these innovative techniques, the PerioLase® MVP-7™ laser (Millennium Dental Technologies, Inc., Cerritos, California) was specifically designed to execute these protocols. A 1064-nm Nd:YAG free-running pulse laser, the PerioLase MVP-7 incorporates unique parameters, features, and safety measures for dental professionals to take control over debilitating diseases in their practices.
The LANAP protocol is FDA-cleared for true regeneration of bone, cementum, and periodontal ligament (PDL) on previously diseased root surfaces. Human histology studies have demonstrated remarkable regeneration of these critical structures, showcasing the protocol’s effectiveness in restoring oral health,3,4 even around multi-rooted teeth.
While selectively targeting diseased tissue and preserving healthy structures, the LANAP protocol regenerates bone without the use of additional biologics such as bone grafts or membranes. It is also capable of significantly reducing bacterial load; one study demonstrated 85% of LANAP-treatment patients were culture-negative for orange and red complex bacterial species immediately posttreatment, compared with 83.3% positivity in patients subjected to traditional ultrasonic root debridement only.5
Much like how the LANAP procedure is tailored to treat periodontal disease, the LAPIP protocol is specifically designed for reversing peri-implantitis. Both protocols utilize the same advanced laser technology, allowing for effective decontamination of the implant surface and targeted treatment of infections while minimizing patient discomfort. In a retrospective study involving 249 implants in 138 patients diagnosed with peri-implantitis, the LAPIP protocol demonstrated an impressive 94% survival rate at a median follow-up time of 13.1 months, offering a minimally invasive solution for common complications associated with dental implants.6

Why address periodontal disease in implant patients?
Treating periodontal disease prior to implant placement is crucial for achieving comprehensive oral care. A healthy periodontal foundation is vital for successful implant outcomes,7 and laser technology plays a key role in addressing this often-overlooked aspect of treatment. By incorporating the concepts of LANAP and LAPIP into practice, we can enhance disease management, improve patient satisfaction, and foster better overall oral health. Additionally, LAPIP treatment provides a minimally invasive solution for reversing the ever growing number of ailing and failing implants.
The versatility of the PerioLase MVP-7 extends beyond periodontal treatment and peri-implantitis. With adjustable presets, this laser can address a variety of clinical needs, from extractions and hemostasis to implant surface decontamination and maintenance. For instance, laser pocket disinfection post-implant placement can reduce bacterial presence and be incorporated into implant maintenance routines. The BLAST™ protocol, another application of the PerioLase MVP-7, targets foreign body reactions and decontaminates implants and extraction sites, optimizing conditions for osseointegration. By utilizing laser technologies throughout the implant process — from extraction to maintenance — dental practices can reduce the need for biologics, control overhead costs, and improve clinical outcomes.

Leading the future of implantology
Integrating laser-assisted protocols like LANAP, LAPIP, and BLAST not only improves patient care but can also position a practice at the forefront of dental implantology. These innovative approaches lead to satisfactory clinical outcomes and can transform patient experiences, resulting in higher acceptance rates. A recent survey of LANAP clinicians revealed that 90.7% of patients are more willing to accept LANAP treatment than traditional osseous/GTR/GBR surgery.8 By embracing these minimally invasive, laser-assisted techniques, dental professionals have a unique opportunity to provide value-added dental care and deliver personalized treatment. In today’s competitive landscape, distinguishing one’s practice relies on providing advanced, patient-centered care, and laser-assisted protocols are essential for achieving implant success and overall oral health management.
Aquoral at the forefront: breaking the mold of dental commodification with value-based care
In the rapidly evolving landscape of dentistry, commodification presents a formidable challenge for dental implant practitioners. As we witness an increasing focus on affordability and transactional models, many providers find themselves caught in a race to the bottom. Patients are often led to view their care solely through the lens of cost — measuring services based on the price of an implant rather than recognizing the profound impact of regaining a healthy smile and the ability to chew. This mindset diminishes the quality of care, reducing complex treatments to mere transactions and neglecting the holistic aspects of patient health.
So, how do we rise above this trend as providers? By embracing value-based care. This approach prioritizes patient-centric care and health outcomes over the mere provision of services. It’s about addressing the whole patient — identifying unmet needs and enhancing outcomes that truly matter. By advocating for holistic care, we can transcend the commoditized nature of today’s dental marketplace and empower our patients to see the true value in their oral health journey.
Delivering long-lasting relief while transforming the dry mouth treatment landscape
Addressing dry mouth, or xerostomia, is crucial for enhancing patient care and outcomes. This often-overlooked condition profoundly affects overall health and can lead to significant complications if left untreated. Patients suffering from severe dry mouth are not merely uncomfortable; they face increased risks of choking, oral sores, and even life-threatening conditions in severe cases. Moderate xerostomia can escalate the likelihood of tooth decay, gum disease, cavities, and altered taste, while also contributing to tooth sensitivity and the demineralization of enamel.9 The implications go beyond oral health, as xerostomia can impact nutrition and lead to a reduced quality of life. Patients often report dissatisfaction with removable dentures, experience tissue friction and sticking with full-arch or large fixed implant-supported restorations, and suffer from increased soreness in denture-bearing tissues.10-12
Understanding the multifaceted nature of dry mouth is essential for dental professionals. It can arise from a range of factors, including medications, underlying health issues, and stress. As we strive to offer holistic care, addressing dry mouth is not just an add-on to our treatments; it’s a vital component of patient-centered care. By proactively identifying and managing xerostomia, we can improve patient satisfaction, enhance treatment outcomes, and ultimately restore the quality of life that our patients deserve. This commitment to comprehensive care underscores our role as advocates for our patients’ health and well-being, moving beyond the transactional model to a more integrated approach that truly values the patient experience.
While head and neck cancer patients and those with Sjögren’s syndrome are commonly recognized as affected demographics, they are not the only individuals struggling with dry mouth. Xerostomia is a widespread condition, impacting nearly one in four adults in the United States, yet it often goes undiagnosed or untreated in our practices.
Certain groups are particularly affected, including patients on polypharmacy and those using CPAP machines for sleep apnea. Common causes of dry mouth include medication side effects, autoimmune disorders, radiation therapy, recreational marijuana use, and CPAP usage. It is estimated that xerostomia affects approximately 22% of adults in the U.S., with higher rates among older populations and CPAP users.13 The prevalence of dry mouth increases significantly with the number of medications taken; only 17% of individuals not on medication report experiencing dry mouth, while this rises to 33.5% for those on three medications and reaches 67% for individuals taking seven or more.14 With about 60% of U.S. adults taking at least one prescription medication and roughly a quarter on four or more, the likelihood of xerostomia increases, particularly among those managing chronic conditions like hypertension and diabetes.15
Approximately 33 million adults in the U.S. use CPAP machines16, and studies found 45% of these users experience dry mouth17, often leading to appliance discontinuation due to discomfort. By recognizing the significant impact of xerostomia and addressing it with comprehensive care, we can provide immense value to our patients and differentiate ourselves as healthcare providers.
Despite the high prevalence of dry mouth, both patients and providers often believe that limited treatment options are available. Many practitioners rely on over-the-counter (OTC) water-based solutions, which provide only temporary relief and require frequent reapplication, especially after eating or drinking. Conversely, prescription medications like pilocarpine offer a more potent solution but come with systemic side effects, limiting their use for many patients. This gap in effective treatment options has left both providers and patients frustrated, with few solutions that can deliver long-lasting relief without complications.
Enter Aquoral, a groundbreaking lipid-based dry mouth solution that addresses the shortcomings of traditional treatments. Unlike water-based solutions that can wash away upon eating or drinking, Aquoral creates a protective lipid layer that provides sustained moisture for up to 6 hours (Figure 6). This innovative prescription-based lipid solution is designed to deliver lasting relief with its advanced Oxidized Glycerol Triester (OGT) technology, making it 4 times as effective in hydrating the tissues and 2 times as effective in maintaining the moisture as many over-the-counter alternatives. This compact and effective solution not only enhances patient comfort but also improves overall quality of life, particularly for CPAP users who suffer from dry mouth during sleep.
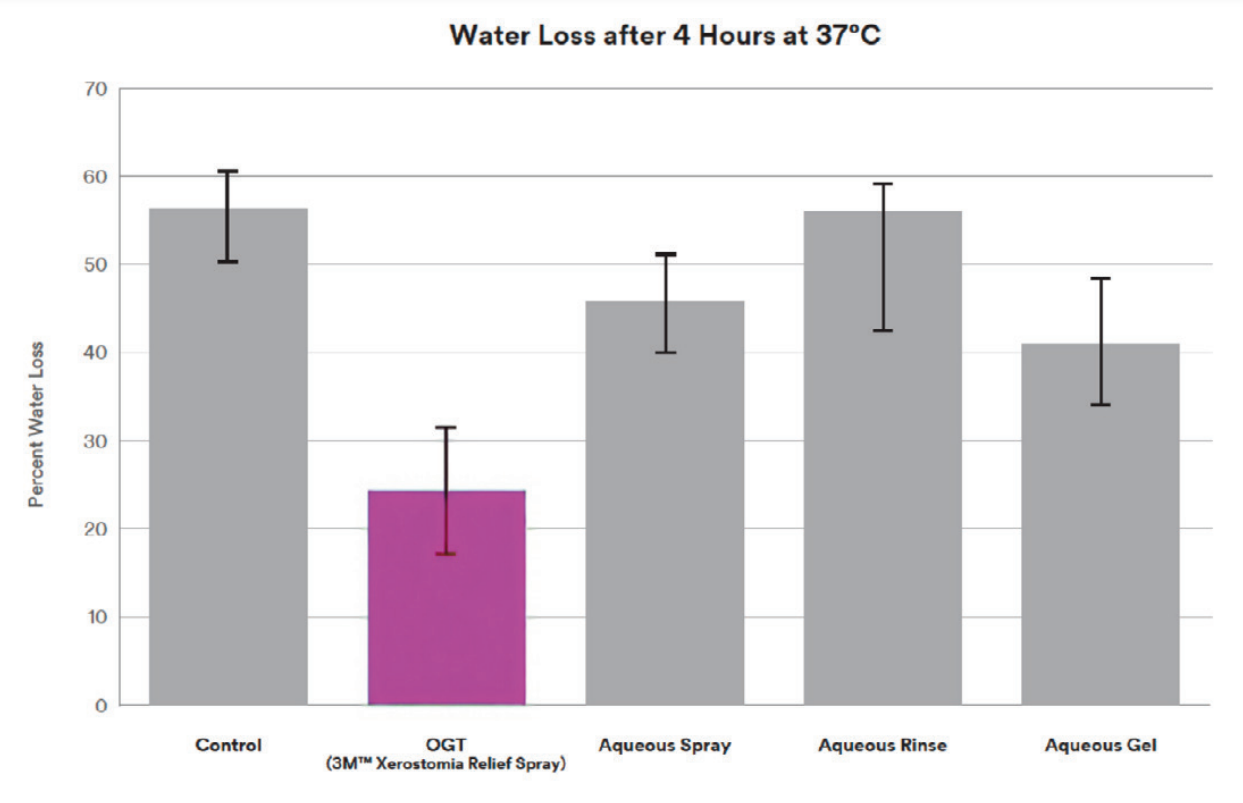
Integrating technologies like Aquoral into practice not only demonstrates a commitment to comprehensive patient care but also addresses a critical aspect of oral health that often goes unrecognized. For patients undergoing full-arch implant treatments, managing dry mouth is essential, as it directly impacts the comfort and success of their prostheses. Many mistakenly believe that discomfort from prosthetics sticking to dry tissues is just part of the experience; however, by screening for and bundling Aquoral with full-arch cases, we can enhance the overall patient experience, leading to greater comfort and fewer complaints — note Aquoral’s ability to reduce the coefficient of friction in Figure 7. Ultimately, Aquoral is more than a solution for dry mouth; it exemplifies how we, as dental professionals, can embrace value-based care. By recognizing and addressing hidden patient needs like xerostomia, we can transcend commoditization and provide meaningful, transformative care. Aquoral’s lipid-based technology elevates our treatment protocols, offering effective, long-lasting relief where traditional methods fall short.

Our primary goal in dental implantology has always been to restore function and esthetics with precision and care, but achieving excellence in patient outcomes requires us to consider the entire person and their overall well-being. By focusing on holistic care and addressing every facet of our patients’ needs, we enhance their quality of life. In conclusion, Aquoral presents an opportunity to elevate patient care and break free from the commoditized nature of dental services. By prioritizing value-based care, we can meet unmet needs like dry mouth, provide innovative solutions that truly improve patient outcomes, and distinguish ourselves in a crowded marketplace. The future of dental care is not just about delivering a service — it’s about enhancing lives, and by embracing this approach, we can ensure that our care is as impactful as it is effective.
- American Academy of Implant Dentistry. What are Dental Implants? https://aaid-implant.org/what-are-dental-implants/. Accessed October 16, 2014.
- Zitzmann NU, Berglundh T. Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008 Sep;35(8 Suppl):286-291.
- Nevins ML, Camelo M, Schupbach P, Kim SW, Kim DM, Nevins M. Human clinical and histologic evaluation of laser-assisted new attachment procedure. Int J Periodontics Restorative Dent. 2012 Oct;32(5):497-507.
- Yukna RA, Carr RL, Evans GH. Histologic evaluation of an Nd:YAG laser-assisted new attachment procedure in humans. Int J Periodontics Restorative Dent. 2007 Dec;27(6):577-587.
- McCawley TK, McCawley MN, Rams TE. Immediate Effects of Laser-Assisted New Attachment Procedure (LANAP) on Human Periodontitis Microbiota. J Int Acad Periodontol. 2018 Oct 1;20(4):163-171.
- Schwarz GM, Harris DM. Laser-assisted treatment of peri-implantitis: a retrospective cohort study. Gen Dent. 2020 May-Jun;68(3):18-25.
- Casado PL, Pereira MC, Duarte ME, Granjeiro JM. History of chronic periodontitis is a high risk indicator for peri-implant disease. Braz Dent J. 2013;24(2):136-141.
- Richman C, Levine RA, Sullivan A, Jiang S, Farber A, Zalewsky J. Perceptions of the LANAP protocol. Decis Dent. 2020 Nov;6(10):18:21-23.
- American Dental Association. Xerostomia (Dry Mouth. https://www.ada.org/resources/ada-library/oral-health-topics/xerostomia. Updated April 24, 2023.
- Chrcanovic, B. R., & Albrektsson, T. (2016). Patient-reported outcomes of implant-supported fixed prostheses: A systematic review. The International Journal of Oral & Maxillofacial Implants, 31(4), 1003-1014.
- Zitzmann NU, Marinello CP. Patientenzufriedenheit mit abnehmbaren Implantat- Rekonstruktionen im zahnlosen Unterkiefer [Patient satisfaction with removable implant-supported prostheses in the edentulous mandible]. Schweiz Monatsschr Zahnmed. 2006;116(3):237-244.
- Schimmel, M., et al. (2013). The impact of oral health on quality of life in edentulous older adults: a systematic review. Gerodontology, 30(1), 33-40.
- Fornari CB, Bergonci D, Stein CB, Agostini BA, Rigo L. Prevalence of xerostomia and its association with systemic diseases and medications in the elderly: a cross-sectional study. Sao Paulo Med J. 2021 Jul-Aug;139(4):380-387.
- Dental, Oral and Craniofacial Data Resource Center. Oral Health U.S., Bethesda, Maryland. 2002 September:115-117 http://drc.hhs.gov/report/pdfs/section14-xerostomia.pdf.
- Nederfors T, Isaksson R, Mörnstad H, Dahlöf C. Prevalence of perceived symptoms of dry mouth in an adult Swedish population–relation to age, sex and pharmacotherapy. Community Dent Oral Epidemiol. 1997 Jun;25(3):211-216.
- Liu Y, Carlson SA, Wheaton AG, Greenlund KJ, Croft JB. Sleep Disorder Symptoms Among Adults in 8 States and the District of Columbia, 2017. Preventing Chronic Disease. Published Dec. 30, 2021. Available at https://www.cdc.gov/pcd/issues/2021/21_0305.htm. Accessed October 23, 2024.
- Pico-Orozco J, Carrasco-Llatas M, Silvestre FJ, Silvestre-Rangil J. Xerostomia in patients with sleep apnea-hypopnea syndrome: A prospective case-control study. J Clin Exp Dent. 2020 Aug 1;12(8):e708-e712.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Sarah Balaster, DMD, received her Doctor of Dental Medicine from Rutgers School of Dental Medicine and earned her certificate in Periodontics from the New York University College of Dentistry. Prior to that, she attained a Bachelor’s of Arts with honors in Fine Arts from Wesleyan University in Connecticut. Her background in both the visual arts and sciences enables her to work with patients to achieve both an esthetic and healthy smile. She strives to treat patients with minimally invasive surgical therapies, such as LANAP (laser periodontal therapy), minimally invasive gum grafting, and laser-assisted dental implant placement. She has advanced training in and is an instructor of laser dentistry. She has also worked on the development and application of soft tissue (gum) grafting techniques to improve esthetics, function, and patient comfort. She is a member of the American Academy of Periodontics, Northeast Society of Periodontics, Southern Academy of Periodontics, American Dental Association, and the Institute for Advanced Laser Dentistry.
Sarah Balaster, DMD, received her Doctor of Dental Medicine from Rutgers School of Dental Medicine and earned her certificate in Periodontics from the New York University College of Dentistry. Prior to that, she attained a Bachelor’s of Arts with honors in Fine Arts from Wesleyan University in Connecticut. Her background in both the visual arts and sciences enables her to work with patients to achieve both an esthetic and healthy smile. She strives to treat patients with minimally invasive surgical therapies, such as LANAP (laser periodontal therapy), minimally invasive gum grafting, and laser-assisted dental implant placement. She has advanced training in and is an instructor of laser dentistry. She has also worked on the development and application of soft tissue (gum) grafting techniques to improve esthetics, function, and patient comfort. She is a member of the American Academy of Periodontics, Northeast Society of Periodontics, Southern Academy of Periodontics, American Dental Association, and the Institute for Advanced Laser Dentistry.

