Drs. Young-Jun Ko, Jeong-Ho Yun, Hong-Cheol Yoon, Baek-Il Kim, and Dong-Won Lee present case studies where measuring biofilm with a biofluorescence device was integral in detecting and treating peri-implantitis.
Drs. Young-Jun Ko, Jeong-Ho Yun, Hong-Cheol Yoon, Baek-Il Kim, and Dong-Won Lee illustrate the use of a new device to measure biofilm on implants
Introduction
As the prevalence of dental implant treatments continues to rise, the incidence of peri-implantitis has also increased, posing a significant threat to the long-term success of implants.1 Peri-implantitis is characterized by inflammation and bone loss caused by the accumulation of biofilm on the implant surface, where metabolic byproducts produced by pathogenic bacteria trigger inflammatory responses and accelerate disease progression.2
However, conventional biofilm removal methods have shown limited efficacy, and clinical examinations combined with radiographic imaging are often insufficient for accurately assessing early-stage lesions.3 In particular, small lesions or subtle biofilm accumulations are difficult to detect visually, highlighting the need for more precise diagnostic and therapeutic technologies.4
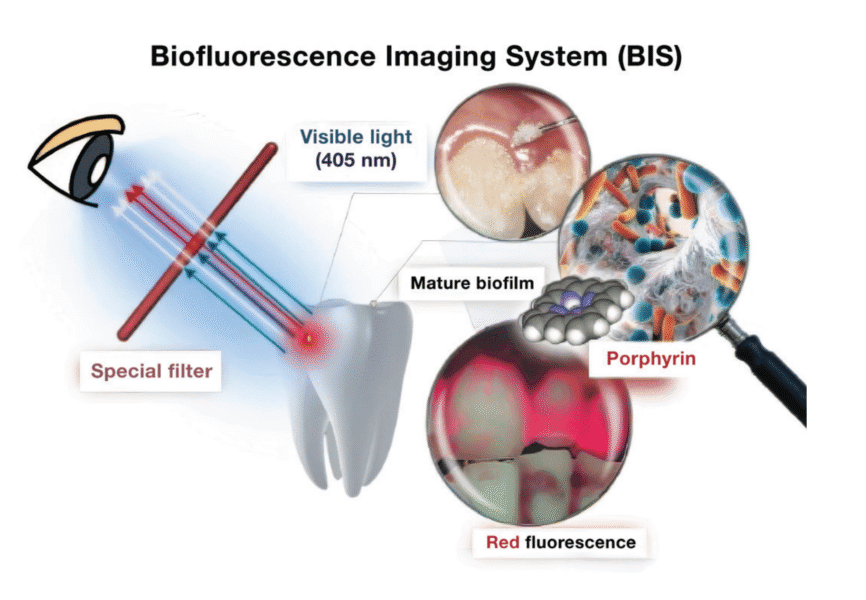
To overcome these limitations, biofluorescence imaging systems (BIS), such as quantitative light-induced fluorescence (QLF), have recently gained attention as innovative alternatives.5 QLF utilizes blue visible light at a specific wavelength (405 nm) to detect red fluorescence emitted by porphyrins produced by mature bacterial colonies, allowing for the quantitative assessment of biofilm location and maturity (Figure 1).6 This real-time visualization enables immediate evaluation of biofilm removal from the implant surface, ultimately enhancing treatment precision.6,7
In these case reports, we present a clinical cases in which QLF (Qraypen C, AIOBIO, Seoul, South Korea; Figure 2) was used to assess biofilm accumulation on the implant surface of a patient with peri-implantitis and to confirm biofilm removal during surgical/non-surgical therapy. Additionally, clinical parameters such as probing depth, bleeding on probing, and radiographic bone loss were evaluated to assess treatment outcomes. Furthermore, we discuss the limitations of this technology and its potential for future advancements. This case highlights the utility of biofluorescence technology as an effective and precise tool for biofilm detection and removal in the treatment of peri-implantitis.
Case presentations
Patients diagnosed with peri-implantitis reported experiencing persistent discomfort and irritation around the implant site over an extended period. Clinical examination revealed moderate gingival inflammation, bleeding on probing, and pus discharge. Radiographic assessment confirmed the diagnosis by demonstrating significant bone loss around the affected implant.
A biofluorescence imaging system (BIS) was used to identify sites of biofilm accumulation on the implant surfaces prior to the initial mechanical debridement. The effectiveness of biofilm removal was evaluated by re-examining the implant surfaces using BIS, and the disappearance of fluorescence was confirmed.
Clinical parameters including probing depth, bleeding on probing, and radiographic bone loss were recorded at baseline and post-treatment to evaluate the overall treatment outcome.
Results
Case 1
An 80-year-old female patient visited the Department of Periodontology at Gangnam Severance Dental Hospital, complaining of an odor emanating from the upper right implant site. Due to the long distance from her residence, she had been unable to attend regular check-ups consistently. The patient had a medical history of osteoporosis and had been receiving Denosumab (Prolia®) injections every 6 months for the past 6 years.
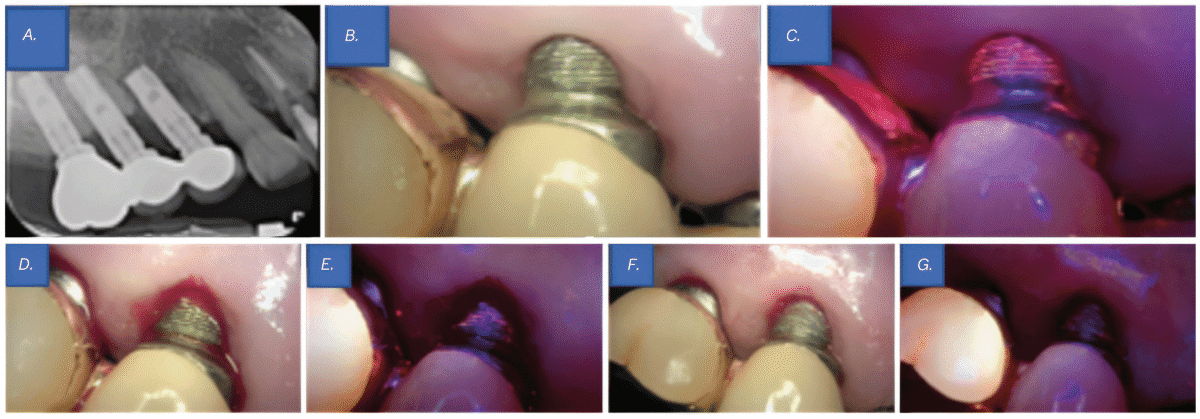
Clinical examination revealed probing depths of 5–6 mm around implant Nos. 4 and 5, with thread exposure at implant No. 5 above the gingival margin. Radiographic examination revealed bone loss around implant Nos. 4 and 5, leading to a diagnosis of peri-implantitis (Figure 3A). Although no significant biofilm accumulation was visible to the naked eye (Figure 3B), evaluation using QLF clearly detected biofilm that was not observable under conventional visual inspection (Figure 3C). Considering the patient’s osteoporosis and the fact that only 4 months had passed since her last denosumab (Prolia®) injection, flap surgery was not performed. Instead, curettage was selected as the treatment approach.
For biofilm removal, cleansing was performed using an ultrasonic scaler (Megagen, Seoul, South Korea), a curette, and a microbrush. After mechanical debridement, QLF imaging was conducted again to compare pre- and post-treatment findings. While no biofilm was visible to the naked eye (Figure 3D), QLF revealed residual biofilm on the implant threads (Figure 3E). Additional debridement was carried out, followed by another round of clinical and QLF imaging for confirmation (Figures 3F-3G). This process enabled a more thorough evaluation of biofilm removal and served as a visual aid for patient education on oral hygiene. Targeted brushing instruction (TBI) was also provided.
The area was then rinsed with 0.2% chlorhexidine, and 2% minocycline ointment (Periocline®, Sunstar, Osaka, Japan) was topically applied to the peri-implant lesion for inflammation control.
At the 2-week follow-up, peri-implant inflammation had significantly decreased, and the patient reported relief from discomfort. At the 6-month follow-up, only mild inflammation was observed in the surrounding area, but the patient remained symptom-free, and the peri-implant tissues were well maintained.
Case 2
A 70-year-old female patient visited the Department of Periodontology at Gangnam Severance Dental Hospital, reporting bleeding from the lower left implant site during brushing. The patient had been regularly attending follow-up appointments at our department but had only received non-surgical treatments due to her dental phobia. Medical history revealed no significant underlying medical conditions.
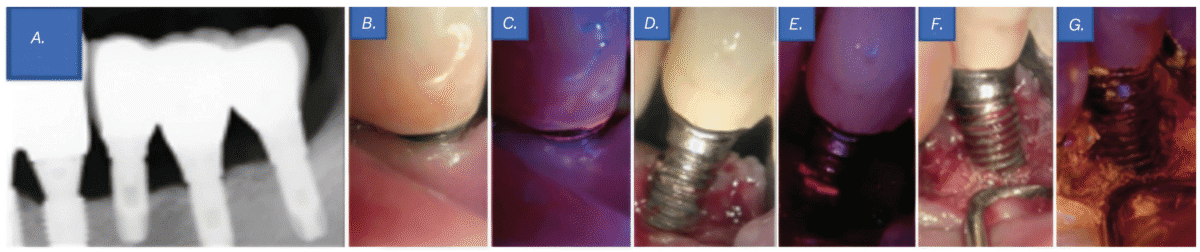
Clinical examination revealed a probing depth of 5–6 mm around implant No. 20, with the implant threads exposed above the gingiva. Although no significant biofilm attachment was observed with the naked eye (Figure 4B), QLF revealed the presence of biofilms (Figure 4C). In addition, periapical radiography revealed bone loss around implant No. 20, leading to a diagnosis of peri-implantitis (Figure 4A). Despite her dental phobia, the patient consented to undergo flap surgery after a thorough explanation of the necessity of actively removing factors contributing to infection from the implant surface.
A sulcular incision was made from the mesial line angle of No. 21 to the distal line angle of implant No. 19 using #15T and #12 blades. Upon flap elevation, visible biofilm was observed (Figure 4D), and its presence was confirmed with QLF imaging (Figure 4E). Biofilm removal was performed using an ultrasonic scaler (Megagen, Seoul, South Korea), a curette, and a microbrush. Tetracycline was additionally applied for implant surface decontamination. Subsequent clinical and QLF imaging confirmed the successful removal of residual biofilm and infectious material (Figure 4F-4G). The surgical site was then closed using 4-0 absorbable synthetic sutures (Coated Vicryl™, Ethicon, Johnson & Johnson, Somerville, New Jersey) with an interrupted suture technique.
One week after the flap surgery, the patient returned for suture removal. The healing process was satisfactory, with no abnormal findings. At 6-month and 1-year follow-ups, the patient reported no discomfort, implant surface hygiene had improved compared to the pre-treatment condition, and the overall oral health remained stable.
Case 3
An 86-year-old female patient initially visited a local dental clinic, where she was advised to seek evaluation and treatment at a university hospital due to severe bone loss around the lower left implant. She subsequently presented for her first visit to the Department of Periodontology at Gangnam Severance Dental Hospital. The patient had no significant underlying medical conditions aside from hyperlipidemia.
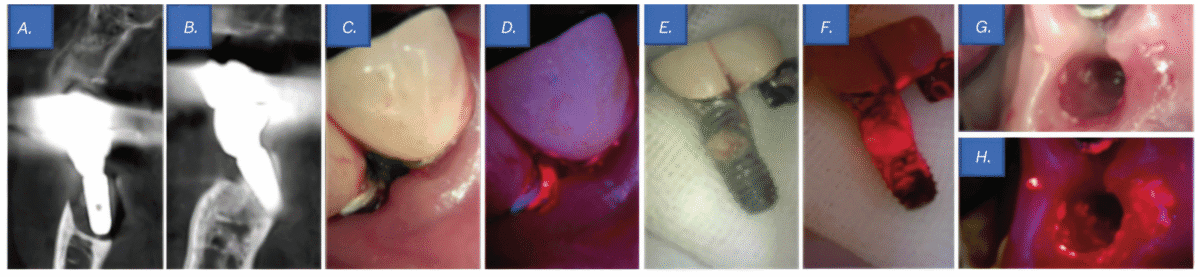
Clinical examination revealed a probing depth of 12 mm around implant No. 19, accompanied by active pus discharge above the gingival margin (Figure 5C). Furthermore, QLF imaging detected red fluorescence from porphyrins, indicating a mature biofilm (Figure 5D). Cone-beam computed tomography revealed bone loss around implant Nos. 18 and 19, leading to a diagnosis of peri-implantitis (Figures 5A-5B). Notably, implant No. 19 exhibited bone loss extending to the apex, and during prosthesis removal, it was spontaneously exfoliated (Figure 5E). Although no significant biofilm was observed macroscopically on the tissue and fixture surfaces (Figure 5G), QLF evaluation detected porphyrin fluorescence, confirming the presence of a biofilm (Figures 5F-5H).
Subsequently, a sulcular incision was made using #15T and #12 blades, followed by socket curettage with tetracycline. The wound was then closed using a figure-eight suture technique with 4-0 absorbable synthetic sutures (Coated Vicryl™, Ethicon, Johnson & Johnson, Somerville, New Jersey).
One week after the implant removal procedure, the patient returned for suture removal. Healing was satisfactory, with no notable complications. At the 6-month follow-up, the patient reported no significant discomfort, and overall oral health was stable compared to the preoperative condition.
Case 4
A 56-year-old male patient presented for his first visit to the Department of Periodontics at Gangnam Severance Dental Hospital, complaining of frequent food impaction around the upper left implant area and mobility posterior teeth. Medical history revealed no significant underlying medical conditions.
Clinical examination revealed a subgingival calculus at site tooth No. 11 and a probing depth of 6 mm at site implant No. 12. Furthermore, based on the panoramic radiography findings, the prognosis of tooth No. 14 was hopeless (Figure 6A); therefore, extraction of tooth No. 14 and flap surgery for implant No. 12 were planned. An intrasulcular incision was made from the mesial line angle of tooth No. 10 to the distal aspect of implant No. 12 using #15T and #12 blades. After flap elevation, subgingival calculus and bone loss were confirmed around tooth No. 11 and implant No. 12, respectively (Figure 6B).
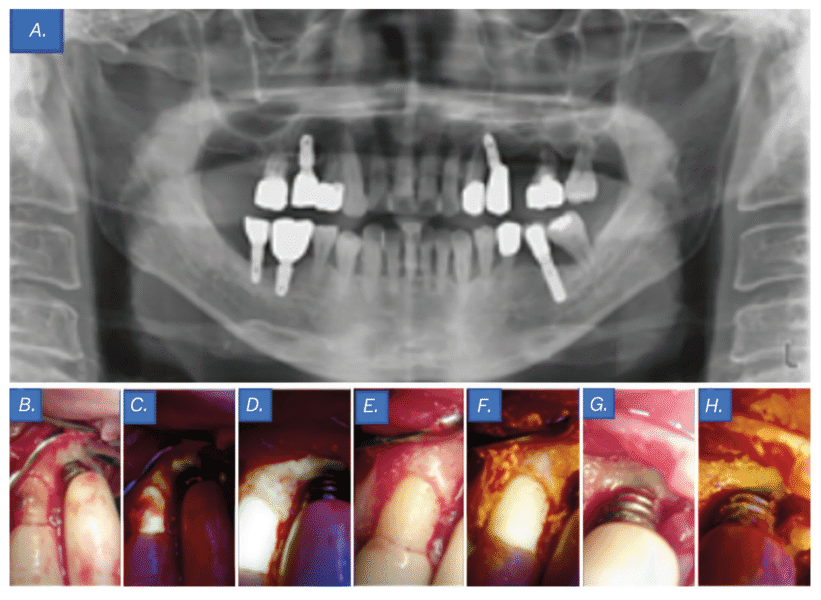
Although no biofilm was visible to the naked eye on the implant No. 12 threads, QLF imaging revealed its presence (Figure 6C). Biofilm removal was performed using an ultrasonic scaler (Megagen, Seoul, South Korea), curette, and microbrush. Follow-up QLF imaging was conducted to evaluate the pre- and post-treatment difference, confirming successful biofilm removal (Figure 6D). The area was irrigated with tetracycline, and additional clinical photographs and QLF images were taken to verify the elimination of biofilm and infection at tooth No. 11 and implant No. 12 (Figures 6E-6H). Interrupted sutures were placed using 4-0 absorbable synthetic sutures (Coated Vicryl™, Ethicon, Johnson & Johnson, Somerville, USA). The importance of oral hygiene management was emphasized using visual aids, and tooth brushing instruction (TBI) was provided.
One week after the flap surgery and implant surface decontamination, the patient returned for suture removal and reported significant relief from discomfort. Healing was uneventful, with no notable complications.
At the 6-month follow-up visit, the patient’s clinical symptoms had resolved. Through regular TBI, implant surface hygiene had improved compared to the pre-treatment condition, and the overall oral health remained stable.
Follow-up summary (Cases 1–4)
At the 1-week and 6-month follow-up after treatment in Cases 1 through 4, clinical reassessments demonstrated significant improvements in gingival inflammation, bleeding on probing, and pus discharge. Radiographic examinations showed that peri-implant conditions remained stable.
This case series highlights the potential of BIS technology in the clinical management of peri-implantitis. Its non-invasive nature and absence of adverse effects further support its value as a precise and patient-friendly diagnostic and therapeutic adjunct in implant dentistry.
Discussion
In this case series, QLF was used as a supplementary diagnostic tool for real-time visualization of the lesion status before and after treatment. This enabled clinicians to identify residual biofilms following the initial debridement, allowing for more thorough implant-surface cleaning.
The use of the BIS contributed to the development of more systematic and individualized treatment plans, ultimately enhancing the precision and success rate of peri-implantitis management.
However, biofluorescence imaging has some limitations. First, the biofilm we aim to detect is primarily located in the apical region rather than in the coronal region. However, currently available QLF devices have large heads, making access to the apical area difficult. Second, in addition to the surgeon retracting the cheek and gingiva, an assistant is required to aid in capturing images. Furthermore, effective control of bleeding is necessary during imaging. Third, areas actively exuding pus should be detected as red on QLF imaging; however, this was not observed in few cases. Further studies are required to investigate this phenomenon. Additionally, studies establishing the long-term clinical efficacy of peri-implantitis treatment with adjunctive biofluorescence imaging and verifying the effectiveness of biofluorescence imaging through comparative studies with existing diagnostic methods are required.
Conclusion
This case series highlights the usefulness of biofluorescence imaging in the clinical management of peri-implantitis. Biofluorescence imaging is a noninvasive, safe, precise, and patient-friendly diagnostic and therapeutic adjunct in implant dentistry.
Editor’s Note: The Lead Author was responsible for the data collection, performing the data analysis, and the composition of the abstract.
For more information on how biofilm can be detrimental to patients with implants, read this CE by Dr. Gregori M. Kurtzman and Debbie Zafiropoulos, titled, “Oral hygiene and dental implant maintenance: part 2,” here: https://implantpracticeus.com/ce-articles/oral-hygiene-and-dental-implant-maintenance-part-2/
- Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015 Apr;42 Suppl 16:S158-171. doi: 10.1111/jcpe.12334.
- Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E, Hämmerle CHF, Heitz-Mayfield LJA, Huynh-Ba G, Iacono V, Koo KT, Lambert F, McCauley L, Quirynen M, Renvert S, Salvi GE, Schwarz F, Tarnow D, Tomasi C, Wang HL, Zitzmann N. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018 Jun;45 Suppl 20:S286-S291. doi: 10.1111/jcpe.12957.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Clin Periodontol. 2018 Jun;45 Suppl 20:S246-S266. doi: 10.1111/jcpe.12954.
- Lee JW, Lee ES, Kim BI. Can red fluorescence be useful in diagnostic decision making of residual dentin caries? Photodiagnosis Photodyn Ther. 2019 Jun;26:43-44. doi: 10.1016/j.pdpdt.2019.02.016. Epub 2019 Feb 20.
- Han SY, Kim BR, Ko HY, Kwon HK, Kim BI. Assessing the use of Quantitative Light-induced Fluorescence-Digital as a clinical plaque assessment. Photodiagnosis Photodyn Ther. 2016 Mar;13:34-39. doi: 10.1016/j.pdpdt.2015.12.002. Epub 2015 Dec 9.
- Kim YS, Lee ES, Kwon HK, Kim BI. Monitoring the maturation process of a dental microcosm biofilm using the Quantitative Light-induced Fluorescence-Digital (QLF-D). J Dent. 2014 Jun;42(6):691-696. doi: 10.1016/j.jdent.2014.03.006. Epub 2014 Mar 19. Erratum in: J Dent. 2014 Dec;42(12):1626.
- Khudanov B, Jung HI, Kahharova D, Lee JW, Hamidov I, Lee ES, Kim BI. Effect of an oral health education program based on the use of quantitative light-induced fluorescence technology in Uzbekistan adolescents. Photodiagnosis Photodyn Ther. 2018 Mar;21:379-384. doi: 10.1016/j.pdpdt.2018.01.012. Epub 2018 Jan 31.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



