Educational aims and objectives
This self-instructional course for dentists discusses a novel new treatment technique for failed zygomatic implant cases.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize some evolutionary history of zygomatic implants.
- Identify some challenges associated with zygomatic
- Identify various changes to zygomatic protocols over time.
- Recognize the indications for HESIAn zygomatic implant technique.
- Observe the technique for using the HESIAn zygomatic
- Recognize some benefits of using the HESIAn zygomatic implant technique.
- Recognize some risks of using the HESIAn technique.
Dr. Dan Holtzclaw introduces our readers to the HESIAn technique for treatment and rescue of failed zygomatic implants.
Dr. Dan Holtzclaw delves into a technique for salvaging failed zygomatic implants
Background
To afford patients with severe maxillary atrophy the opportunity for dental implant treatment without major bone grafting procedures, anchorage into the malar process was proposed as early as the mid-1980s.1 The original Brånemark protocol called for bilateral zygomatic implants anchored into the mid-body of the zygoma via an intrasinus approach.2,3 This approach, however, was not without problems, including:
- palatal positioning of zygomatic fixture platforms which caused discomfort and speech issues for some patients
- high rates of maxillary sinusitis in certain patients which some clinicians felt was related to the 100% perforation rate of the Schneiderian membrane with the intrasinus path of the zygomatic implant
- decreased visualization of the osteotomy drills with the intrasinus path
- oroantal fistula formation secondary to degradation of thin palatal bone at the platform position when using intrasinus paths
- unusual prosthetic configurations with extensive palatal extensions.4-9
To address these concerns, Stella and Warner proposed a modification to the original Brånemark intrasinus protocol whereby a “slot” was made in the external wall of the maxillary sinus allowing for more lateral “extrasinus” positioning of the zygomatic implant.10 This lateral positioning resulted in a more favorable prosthetic position of zygomatic implant platforms, thus reducing many of the palatal emergence issues associated with the original Brånemark protocol. Additionally, the authors noted that substitution of the lateral slot for the window needed with the intrasinus protocol allowed for better surgical visualization and improved the speed of the procedure.
While some clinicians in the early 2000s focused on better positioning of zygomatic implant platforms, others questioned the need for the additional bone grafting procedures which were required for many patients treated with the original Brånemark zygomaticus protocol. As these additional bone grafting procedures often produced higher failure rates for conventional dental implants in addition to increased treatment time, cost, and morbidity for patients, the concept of using multiple fixtures per zygoma in lieu of bone augmentation was considered. As an alternative to Brånemark’s original zygomatic implant protocol, in 2003, Bothur, et al., proposed a graftless procedure utilizing at least two zygomatic implants anchored into each zygoma.11 This protocol eliminated the need for additional bone grafting procedures to provide an enhanced patient experience and improve overall survivability of prostheses supported in this manner.
In 2011, Aparicio, et al., proposed a refinement of the zygomatic implant process with the “ZAGA” (Zygoma Anatomy Guided Approach) protocol.12 Rather than simply being a new technique, as was the case with previous movements from from intrasinus to extrasinus methods, The ZAGA concept considered patient specific anatomy to use a variety of zygomatic implant positions and/or specific implant fixtures for treatment. A decade later, Holtzclaw and Gonzalez introduced another full arch protocol that incorporated zygomatic implants for improved prosthetic outcomes.13 Like ZAGA, the PATZi (Pterygoid, Anterior, Tilted, Zygomatic, implants) protocol utilized a combination of implant styles to treat atrophic maxillae based upon patient-specific anatomy. The PATZi protocol, however, allowed clinicians to rapidly alter their treatment approach in real-time based on instrasurgical conditions that may arise during treatment.
As the fourth decade of treatment with zygomatic implants quickly approaches, the evolution of this treatment modality continues to advance, expanding the scope of treatment for those afflicted with severely atrophied maxillae. In this article, the author introduces the HESIAn zygomatic implant protocol: (H)oltzclaw (E)xtra (S)inus (I)nfratemporal (An)chorage.

Technique description
The HESIAn technique was born out of necessity for the treatment and rescue of previously failed zygomatic implant cases. Survival/success means the implants are osseointegrated with no mobility, infection, radiolucency, and are able to support their intended function for prosthetic support. Failure of a zygomatic implant can often lead to large defects of the malar process that can complicate the placement of additional implants (Figures 1-3).13 In many of these cases, adequate bone remains in the dorsal zygoma as it approaches the temporal process since zygomatic implant fixtures are not often placed here with initial treatment (Figure 4). Depending on the resultant defect from a failed zygomatic implant, preparation and approach to reach this area can be complicated. Often, previously placed zygomatic fixtures may have significantly altered lateral sinus wall anatomy or destroyed it completely (Figure 5). Additionally, failing zygomatic fixtures frequently produce sinusitis and create situations where placement of another implant through the sinus is discouraged.14-17 With this in mind, the HESIAn technique avoids the lateral sinus wall and the sinus in most cases.

The HESIAn zygomatic implant technique requires modifications compared to existing zygomatic implant protocols. While the standard zygomatic implant traverses the zygomatic buttress or just anterior to this anatomic feature, the HESIAn zygomatic implant is located dorsal to the buttress and crosses the anterior third of the infratemporal fossa (Figure 6). As such, incision design must be modified with posterior vertical releasing incisions moved to a more dorsal position closer to the pterygoid implant. Additionally, the more posterior location of the HESIAn zygomatic implant requires more extensive tissue dissection to achieve unimpeded clearance in the infratemporal fossa (Figure 7). This is critical for both effectiveness and safety with anatomic structures such as the buccal fat pad and ptergygoid venous plexus being propinquitious (near) to this area.13 Furthermore, the ventral portion of the masseteric tendon must be dissected and stripped to expose additional malar real estate for engagement of the HESIAn zygomatic implant fixture (Figure 8).
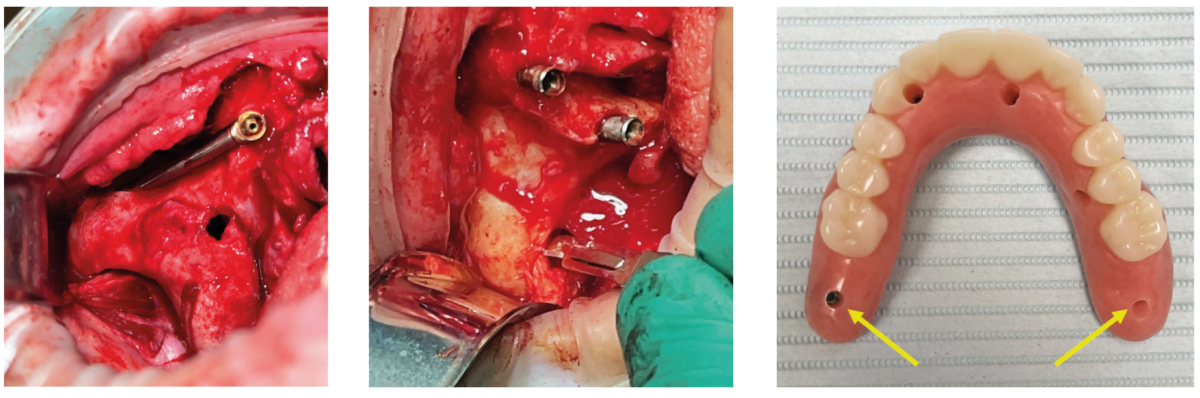
Once adequate exposure of the surgical site has been achieved with the aforementioned preparatory modifications, osteotomy creation commences. While zygomatic implant platform positioning typically occurs at the second premolar or first molar with traditional techniques,1,18,19 HESIAn protocol produces platform positions at either the second or third molar position (Figure 9). Osteotomy preparation begins by selecting platform position on the residual alveolar ridge according to the patient’s specific condition. The extrasinus barrel bur is then positioned at this point and crosses the infratemporal fossa in a position dorsal to the zygomatic buttress (Figure 10). The tip of the barrel bur should touch the medial aspect of the malar process in line with the desired apical exit point of the HESIAn zygomatic implant. Depending on the depth of the residual alveolar ridge, the barrel bur is advanced to a point whereby the bur is either level to the adjacent bone or not fully into the maxillary sinus.
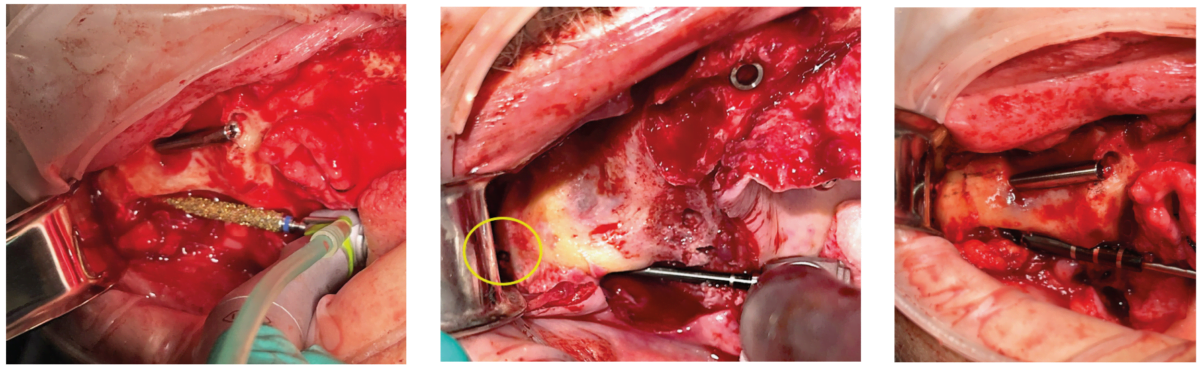
Once the channel is created into the residual alveolar ridge, a sharp marking drill is laid into the channel and advanced until it touches the medial aspect of the malar process. It is very important to note that this is done without the drill running. The curvature of the medial zygoma creates the potential for the drill to slip, and using a sharp marking drill reduces the risk of this happening. With the sharp marking drill firmly embedded into the channel created in the alveolar ridge, it is advanced through the medial aspect of the bone until it penetrates the lateral aspect (Figure 11). It is important to achieve full drill penetration for the following reasons:
- visualization of implant exit point which prevents collision with preexisting anterosuperior zygomatic implants, avoidance of preexisting defects from failed implants, and confirmation that the implant apex will not end up in the infratemporal fossa
- bicortical anchorage for maximum implant stability
- ability to adjust the timing of final multi-unit abutment positioning without bottoming out of the implant.
During the drilling process, it is important to protect the tissues of the dissected infratemporal fossa from being tangled up with the advancing drill. Failure to do so may result in premature exposure of the buccal fat pad and/or violation of the pterygoid venous plexus.
Once the initial marking drill has safely penetrated the lateral zygomatic cortex, subsequent drills are used to widen the osteotomy (Figure 12). It is important to note that due to the posterior positioning of the zygomatic implant fixture with the HESIAn technique, implant systems with longer drills will not work. The dense nature of the posterior malar process precludes underdrilling the osteotomy to less than adequate diameter.
With typical extrasinus zygomatic implant osteotomy preparation, measurement for fixture length is recommended to be performed at the most inferior aspect of the oblique exit point minus 2.5 mm to account for the multi-unit abutment. With the HESIAn protocol, however, the author has found that this measurement protocol often results in shorter than desired platform positions. As such, the author recommends not to subtract 2.5 mm from the apical exit measurement when using HESIAn.
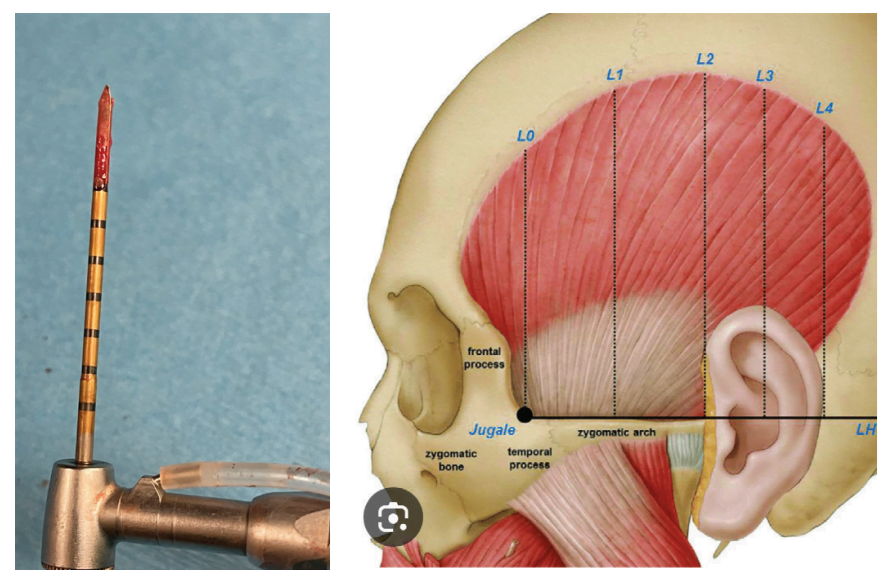
After osteotomy preparation, it is important to thoroughly irrigate the medial and lateral aspects of the posterior malar process. In most instances, the HESIAn protocol does not typically penetrate the maxillary sinus so intrasinus irrigation is not required. The appropriately sized zygomatic implant is then placed into the slot preparation of the alveolar ridge and advanced through the anterior third of the infratemporal fossa until it reaches the HESIAn osteotomy at the medial aspect of the malar process. With firm palatal pressure to ensure intimate contact with the residual alveolar ridge, the zygomatic implant is advanced to engage the bone of the posterior zygoma. Due to the oblique nature of the osteotomy preparation, the author has found that up to 10 mm of bone to implant engagement is achieved (Figure 13) with extremely high insertion torque.
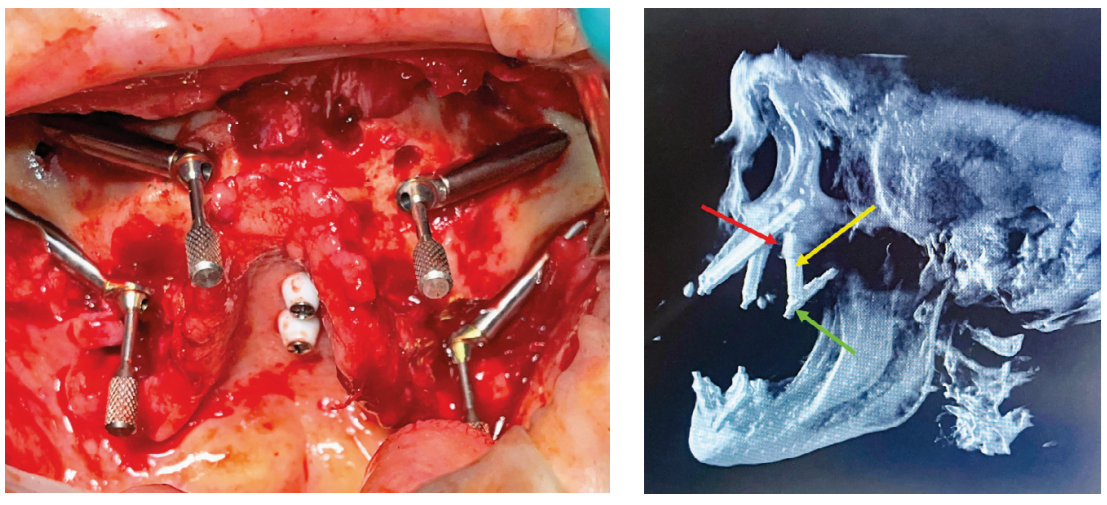
The unique position of HESIAn zygomatic implants often results in shorter fixture lengths ranging from 30 mm to 45 mm. The oblique angulation of these implants often requires multi-unit abutments ranging from 45 degrees to 60 degrees when a zero degree fixture is utilized (Figure 14).
Results
To date, the author has used the HESIAn protocol for 20 immediately loaded zygomatic implant fixtures with zero failures. Mean follow-up time for these procedures is 8.4 months (range 2 to 24 months). With every HESIAn zygomatic fixture placed, insertion torque exceeded 45 Ncm, which is the maximum measurement for the manufacturer’s wrench used in these procedures. To date, there have been zero instances of gingival recession with HESIAn fixtures. Because these implants do not enter the maxillary sinus, there have been zero cases of maxillary sinusitis associated with HESIAn zygomatic implants of this paper.
Discussion
Zygomatic implants have nearly 40 years of documented use in rehabilitation of atrophic maxillae.1-3 Systematic reviews and meta-analyses indicate that zygomatic implants have high long-term survival rates comparable to conventional fixtures. A recent publication by Moraschini, et al., evaluated 18 studies encompassing 5,434 dental implants (2,972 zygomatic and 2,462 conventional fixtures).20 With a mean follow-up of 91.5 months, zygomatic implants had a 96.5% survival rate. Roper, et al., found similar results in their systematic review and meta-analysis where 1,349 zygomatic implants had a 96.2% survival rate at 6 years.21 In both studies, maxillary sinusitis was the most commonly documented compliation with a prevalence of 14.2% at 5 years.21 Although zygomatic implants have a high survival rate, their failure can be catastrophic for severely atrophic maxillae. For many cases such as those treated with quad zygomatic fixtures, the loss of even one fixture may render the prosthetic unusable.22 When this occurs, resultant defects often limit bone available for replacement fixtures.
The HESIAn protocol is a technique that has been used by the author to salvage a number of failing zygomatic implant cases (Figure 15). To avoid defects from these failed fixtures, the HESIAn zygomatic implant typically engages zones B3 or C3 according to the classifications of Wang and Hung.23,24 While these zones have lesser thickness than other areas of the zygoma, they are still typically thick enough to achieve high insertion torque as evidenced in the findings of this study. This is aided by the oblique dorsosuperior insertion plane of the HESIAn zygomatic implant which increases bone to implant contact over the horizontal measurements that were used in determining bone thickness of the aforementioned anatomic studies. In most cases, HESIAn zygomatic implants will engage up to 10 mm of bone. In situations of anatomic defects secondary to failing zygomatic implants, the dorsal engagement of HESIAn zygomatic implants affords the clinician additional bone to engage as zones L2, L3, Lb, and Lc are the longest parts of the malar process according to the anatomic studies.23,24 Furthermore, these dorsal locations near the jugale have been found to be 16.6% denser than areas such as the mid-body of the zygoma.25
In addition to securing alternative anchorage sites for failed zygomatic implants, the HESIAn protocol produces prosthetic results that eliminate cantilevers. Most zygomatic implant treatments that do not employ PATZi or pterygoid implants have posterior platform positions at either the second premolar or first molar and subsequent prosthetic cantilevers.1,18,19 Davo’s 2024 study evaluating patients treated with quad zygomatic implants, for example, reported that cantilevers were present in 75% of prostheses.22 In the 14 patients treated with HESIAn zygomatic implants for this retrospective study, there were zero prosthetic cantilevers.
Cantilever elimination can be benficial for zygomatic implants as noted by the Ishak series of finite element analysis studies for malar fixtures.26-28 In this trio of studies, Ishak, et al., note that longer cantilevers produced higher stresses within the body of zygomatic implants. Additionally, these authors note that distal zygomatic implant platform positions further away from points of maximum occlusal load, which typically occur in the posterior maxilla, result in a near 2-fold increase of stress within loaded prostheses. As HESIAn zygomatic implants have platforms that typically exit at the second or third molar, they address these concerns of the Ishak studies by both eliminating cantilevers and having posterior platform exit points in the area of maximum occlusal force generation. The posterior exit point of HESIAn zygomatic implants does generate possible interference with positioning of pterygoid implants and this should be taken into consideration when planning cases.
Conclusion
The (H)oltzclaw (E)xtra (S)inus (I)nfratemporal (An)chorage (HESIAn) zygomatic implant protocol continues the near 40-year evolution of malar fixture treatment for atrophic maxillae. This technique is intended for either the rescue of failed zygomatic implant cases or maximizing anterior-posterior (AP) prosthetic spread in patients where pterygoid implants are not an option. The HESIAn protocol for zygomatic implants is highly advanced and should only be attempted by clinicians with significant experience placing malar fixtures. Long term follow-up and additional controlled studies further evaluating use of HESIAn zygomatic implants are warranted by the promising findings of this retrospective study.
References
- Brånemark PI, Gröndahl K, Ohrnell LO, Nilsson P, Petruson B, Svensson B, Engstrand P, Nannmark U. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70-85.
- Parel SM, Brånemark PI, Ohrnell LO, Svensson B. Remote implant anchorage for the rehabilitation of maxillary defects. J Prosthet Dent. 2001 Oct;86(4):377-81.
- Aparicio C. Brånemark P, Keller EE, Olivé J. Reconstruction of the premaxilla with autogenous iliac bone in combination with osseointegrated implants. Int J Oral Maxillofac Implants.1993;8:61-67.
- Lopes A, de Araújo Nobre M, Ferro A, Moura Guedes C, Almeida R, Nunes M. Zygomatic Implants Placed in Immediate Function through Extra-Maxillary Surgical Technique and 45 to 60 Degrees Angulated Abutments for Full-Arch Rehabilitation of Extremely Atrophic Maxillae: Short-Term Outcome of a Retrospective Cohort. J Clin Med. 2021 Aug 16;10(16):3600.
- Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000 Nov-Dec;15(6):889-893.
- Aleksandrowicz P, Kusa-Podkańska M, Grabowska K, Kotuła L, Szkatuła-Łupina A, Wysokińska-Miszczuk J. Extra-Sinus Zygomatic Implants to Avoid Chronic Sinusitis and Prosthetic Arch Malposition: 12 Years of Experience. J Oral Implantol. 2019 Feb;45(1):73-78.
- Aparicio C, Polido WD, Zarrinkelk HM. The Zygoma Anatomy-Guided Approach for Placement of Zygomatic Implants. Atlas Oral Maxillofac Surg Clin North Am. 2021 Sep;29(2):203-231.
- Aparicio C, Manresa C, Francisco K, Aparicio A, Nunes J, Claros P, Potau JM. Zygomatic implants placed using the zygomatic anatomy-guided approach versus the classical technique: a proposed system to report rhinosinusitis diagnosis. Clin Implant Dent Relat Res. 2014 Oct;16(5):627-642.
- Aparicio C, Ouazzani W, Hatano N. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontol 2000. 2008;47:162-171.
- Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000 Nov-Dec;15(6):889-893.
- Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants. 2003 Nov-Dec;18(6):902-904.
- Aparicio C. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey. Eur J Oral Implantol. 2011 Autumn;4(3):269-275.
- Holtzclaw D. Remote Anchorage Solutions for Severe Maxillary Atrophy: Zygomatic, Pterygoid, Transnasal, Nasal Rim, Piriform Rim, Nasopalatine, and Trans-Sinus Dental Implants. Austin, Texas: Zygoma Partners; 2023.
- Lan K, Wang F, Huang W, Davó R, Wu Y. Quad Zygomatic Implants: A Systematic Review and Meta-analysis on Survival and Complications. Int J Oral Maxillofac Implants. 2021 Jan-Feb;36(1):21-29.
- Chrcanovic BR, Abreu MH. Survival and complications of zygomatic implants: a systematic review. Oral Maxillofac Surg. 2013 Jun;17(2):81-93. Chrcanovic BR, Abreu MH. Survival and complications of zygomatic implants: a systematic review. Oral Maxillofac Surg. 2013 Jun;17(2):81-93.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J Oral Maxillofac Surg. 2016 Oct;74(10):1949-1964.
- Fiamoncini, E. S., Guimarães, G. M. M. M. de F., Alcalde, L. F. A., Mello, M. Of A. B., Ferreira Júnior, O., de Carvalho, P. S.S. P. Complications in the use of zygomatic implants for the treatment of atrophic maxillary rehabilitation: literature review. Journal of Multidisciplinary Dentistry. 2020;10(1), 41–45.
- Tuminelli F, Balshi T. Zygomatic implants: Position statement of the American College of Prosthodontists 2016. https://www.prosthodontics.org/about-acp/position-statement-zygomatic-implants/ (Accessed May 16, 2024).
- Hirsch JM, Ohrnell LO, Henry PJ, Andreasson L, Brånemark PI, Chiapasco M, Gynther G, Finne K, Higuchi KW, Isaksson S, Kahnberg KE, Malevez C, Neukam FW, Sevetz E, Urgell JP, Widmark G, Bolind P. A clinical evaluation of the Zygoma fixture: one year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004 Sep;62(9 Suppl 2):22-29.
- Moraschini V, de Queiroz TR, Sartoretto SC, de Almeida DCF, Calasans-Maia MD, Louro RS. Survival and complications of zygomatic implants compared to conventional implants reported in longitudinal studies with a follow-up period of at least 5 years: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2023 Feb;25(1):177-189.
- Brennand Roper M, Vissink A, Dudding T, Pollard A, Gareb B, Malevez C, Balshi T, Brecht L, Kumar V, Wu Y, Jung R. Long-term treatment outcomes with zygomatic implants: a systematic review and meta-analysis. Int J Implant Dent. 2023 Jul 5;9(1):21.
- Davó R, Fan S, Wang F, Wu Y. Long-term survival and complications of Quad Zygoma Protocol with Anatomy-Guided Approach in severely atrophic maxilla: A retrospective follow-up analysis of up to 17 years. Clin Implant Dent Relat Res. 2024 Apr;26(2):343-355.
- Wang H, Hung K, Zhao K, Wang Y, Wang F, Wu Y. Anatomical analysis of zygomatic bone in ectodermal dysplasia patients with oligodontia. Clin Implant Dent Relat Res. 2019 Apr;21(2):310-316
- Hung KF, Ai QY, Fan SC, Wang F, Huang W, Wu YQ. Measurement of the zygomatic region for the optimal placement of quad zygomatic implants. Clin Implant Dent Relat Res. 2017 Oct;19(5):841-848.
- Kato Y, Kizu Y, Tonogi M, Ide Y, Yamane GY. Internal structure of zygomatic bone related to zygomatic fixture. J Oral Maxillofac Surg. 2005 Sep;63(9):1325-1329.
- Ishak MI, Abdul Kadir MR, Sulaiman E, Abu Kasim NH. Finite element analysis of different surgical approaches in various occlusal loading locations for zygomatic implant placement for the treatment of atrophic maxillae. Int J Oral Maxillofac Surg. 2012 Sep;41(9):1077-1089.
- Ishak MI, Kadir MR, Sulaiman E, Kasim NH. Finite element analysis of zygomatic implants in intrasinus and extramaxillary approaches for prosthetic rehabilitation in severely atrophic maxillae. Int J Oral Maxillofac Implants. 2013 May-Jun;28(3):e151-160
- Ishak M, Rosli M, Jamalludin M, Termizi S, Khor C, Nawi M. Biomechanical assessment of different surgical approaches of zygomatic implant placement on prosthesis stress. 1st Int Conference on Science, Engineering, and Technology (ICSET) 2020. IOP Conf Series: Materials Science and Engineering. 932 (2020) 012108: 1-8.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Dan Holtzclaw, DDS, MS, is Chief Clinical Officer of Advanced Dental Implant Centers and Director of Fixed Arch Services at Affordable Care, LLC, Morrisville, North Carolina. He is a Diplomate of the American Board of Periodontology and Diplomate of the International Congress of Oral Implantologists. Dr. Holtzclaw has published over 60 articles in peer reviewed journals in addition to multiple textbooks. He served as the Editor-In-Chief of the Journal of Implant and Advanced Clinical Dentistry for 13 years in addition to serving as an editorial board member and/or editorial reviewer for several other dental journals.
Dan Holtzclaw, DDS, MS, is Chief Clinical Officer of Advanced Dental Implant Centers and Director of Fixed Arch Services at Affordable Care, LLC, Morrisville, North Carolina. He is a Diplomate of the American Board of Periodontology and Diplomate of the International Congress of Oral Implantologists. Dr. Holtzclaw has published over 60 articles in peer reviewed journals in addition to multiple textbooks. He served as the Editor-In-Chief of the Journal of Implant and Advanced Clinical Dentistry for 13 years in addition to serving as an editorial board member and/or editorial reviewer for several other dental journals.

