Educational aims and objectives
This self-instructional course for dentists aims to delve into the complexities of removing failed dental implants, explore the reasons behind implant failure, observe the surgical techniques involved in extraction, and identify the critical aspects of post-removal rehabilitation.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize early signs of implant failure.
- Identify risk factors that predispose patients to implant
- View failed implants as opportunities for learning and
- View implant removal as a staged process, involving preoperative assessment, surgical intervention, and postoperative rehabilitation.
- Recognize the significance of post-removal rehabilitation techniques.
Dr. Steven Vorholt delves into the complexities of implant removal and replacement.
Dr. Steven Vorholt discusses the importance of identifying and addressing implants that warrant removal
Each year, millions of dental implants are placed worldwide, offering patients a reliable solution for replacing missing teeth and restoring oral function. With an impressive survival rate of around 98%, dental implants have revolutionized modern dentistry, providing long-lasting benefits to countless individuals. However, even with such high success rates, a small percentage of implants may encounter complications, leading to failure and necessitating removal. Considering the staggering volume of implants placed annually — even a 2% failure rate translates to a substantial number of cases requiring intervention. Timely removal of failed implants is crucial to prevent further complications and preserve oral health. When left untreated, failed implants can become sources of infection, leading to bone loss, tissue damage, and potentially compromising neighboring teeth. Therefore, understanding the importance of identifying and addressing failed implants promptly is paramount in ensuring optimal patient outcomes and maintaining the integrity of the surrounding oral structures.
When a dental implant is exhibiting signs of failure, prompt removal is imperative to prevent additional harm to the alveolar process, adjacent teeth or implants, and to ensure the patient’s health and comfort. Common indicators of implant failure include pain, dull sounds upon percussion, purulence, radiographic evidence of bone loss and radiolucency, as well as mobility. However, the necessity for implant removal extends beyond infection and failure. Instances where implants are poorly positioned for restoration, previously integrated implants requiring extraction for full arch implant treatment, or rare but severe patient allergies to dental implants also warrant removal.
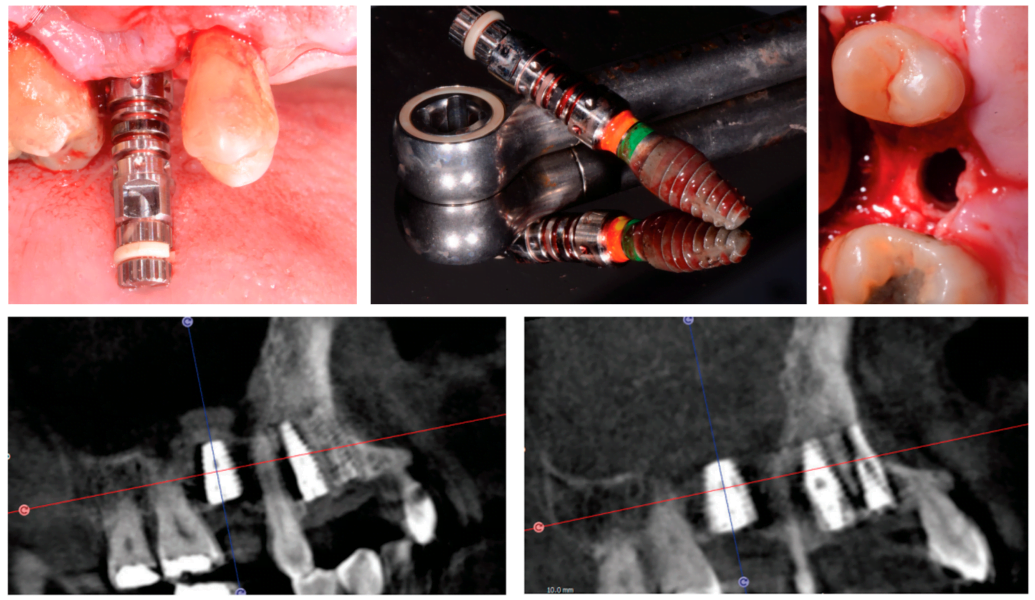
The simplest dental implants to remove are those that fail to osseointegrate. Typically, these implants display mobility and can be extracted using rongeurs or forceps alone. Alternatively, the insertion driver can be utilized, and the implant can be reversed out. However, caution must be exercised when dealing with infected and mobile implants near the maxillary sinus to prevent inadvertent displacement into the sinus cavity. While attempts to retrieve dislodged implants through the osteotomy may be successful, more complex cases may necessitate a Caldwell-Luc approach into the lateral wall of the sinus. To mitigate this risk, it is advisable to refrain from using instruments that exert apical pressure on the implant. Instead, an open tray impression coping or fixed guided carrier can be meticulously engaged into the connection, providing a more secure grip for successful implant removal (Figures 1A-1E).
When dealing with integrated implants that require removal, the initial approach should prioritize conservatism. In cases where osseointegration needs to be broken, employing the insertion driver in reverse, aiming for approximately 60Ncm, can yield success, particularly in the posterior maxilla or implants with considerable crestal bone loss. However, it’s crucial to exercise caution and refrain from applying maximum torque in reverse, as these drivers are typically not designed to withstand torque exceeding 80Ncm. Exceeding this threshold can lead to stripping or fracturing of the driver.
If attempts to reverse-torque the integrated implant are unsuccessful, the next step involves considering a fixture removal kit. Salvin Dental offers a popular kit, and similar options are available in the market. This kit typically includes a reverse-threaded tap, which is inserted into the implant connection and engaged in a counterclockwise direction until it cold welds into the implant. This allows the counterclockwise force to be transferred to the entire fixture. Such kits often come with longer torque wrenches, enabling forces of up to 120Ncm, and are suitable for most implants in the maxilla and posterior mandible. The implant fixture tap will be ankylosed into the implant body and unable to be removed without reversing paired vice grips, and can be expensive to replace.
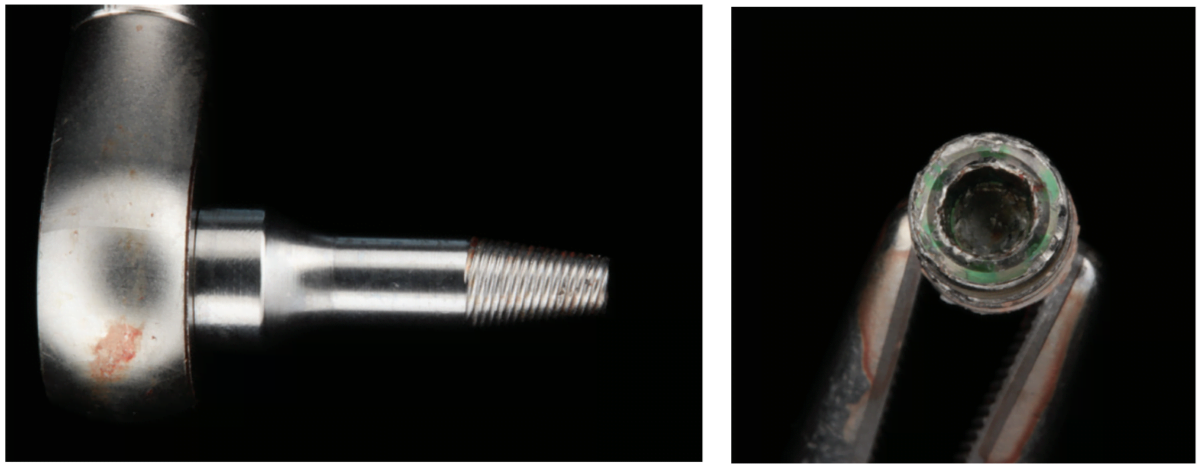
However, potential complications with this technique include fracture of the fixture removal tip or flowering of the dental implant (Figures 2A-2B). Surgeons should be mindful of the material and thickness of the implant being removed. Commercially pure titanium and implants with thinner connection walls are more susceptible to flowering compared to alloy implants with larger platform switches. Understanding these factors is crucial for minimizing complications and ensuring successful implant removal and may force a surgeon to consider skipping the fixture removal tap in favor of a trephine removal technique.
Trephine drills are widely recognized as one of the most aggressive techniques for dental implant removal, offering a high level of predictability. However, they can complicate immediate replacement with a new implant due to the widening of the osteotomy during the removal process. These drills function similarly to core sample drills, cutting a cylindrical section of bone surrounding the integrated dental implant to remove the entire plug of integrated bone and implant. It’s worth noting that it’s often unnecessary to take the trephine drill to full depth. Instead, a step-wise approach is recommended, drilling incrementally to depths such as half, two-thirds, and three-quarters of the implant length. This strategy helps avoid removing more bone than necessary. It’s important to exercise caution when using trephines near vital anatomy, as implants close to critical structures may be contraindicated for trephine use or limited to a depth that does not encroach on vital structures such as the mandibular lingual plate or mandibular nerve canal. This ensures patient safety and minimizes the risk of complications during the removal process.
After the removal of a dental implant, the decision to immediately replace it with another implant should be approached similarly to the decision-making process for placing immediate implants after tooth extraction. Several factors must be considered, including the available bone volume to ensure primary stability of the new implant, the establishment of an appropriate restorative position for future implant restoration, and ensuring adequate space from vital structures.
Furthermore, thorough removal and debridement of the osteotomy site, as well as any infected tissue or bone surrounding the previous implant, are crucial steps in the process. This is akin to the approach taken during immediate implant placement around a chronically infected or periodontally involved tooth. By meticulously cleaning the site and ensuring the removal of any diseased tissue, optimal conditions for successful implant osseointegration and long-term stability can be achieved.
Case examples
Simple removal with reverse torque
During the uncovering phase of a lower overdenture case, a posterior implant was observed to display early crestal bone loss. To address this issue, the implant was carefully removed using reverse torque with the insertion driver, minimizing additional bone removal. Subsequently, the osteotomy site was meticulously cleaned to ensure removal of any debris or infected tissue. A new implant, wider and deeper than the previous one, was then placed into the same osteotomy site.
During the healing process, the newly placed implant was buried, while the other integrated implants were utilized to support the overdenture prosthesis. This allowed for the replacement implant to integrate successfully without bearing load during the initial healing period. Once the replacement implant had fully integrated, it could be uncovered and incorporated into the prosthetic restoration, ensuring optimal function and stability of the overdenture. This approach enabled the successful management of early crestal bone loss while maintaining the integrity of the implant-supported overdenture (Figures 3A-3H).
Implant removal with fixture removal kit
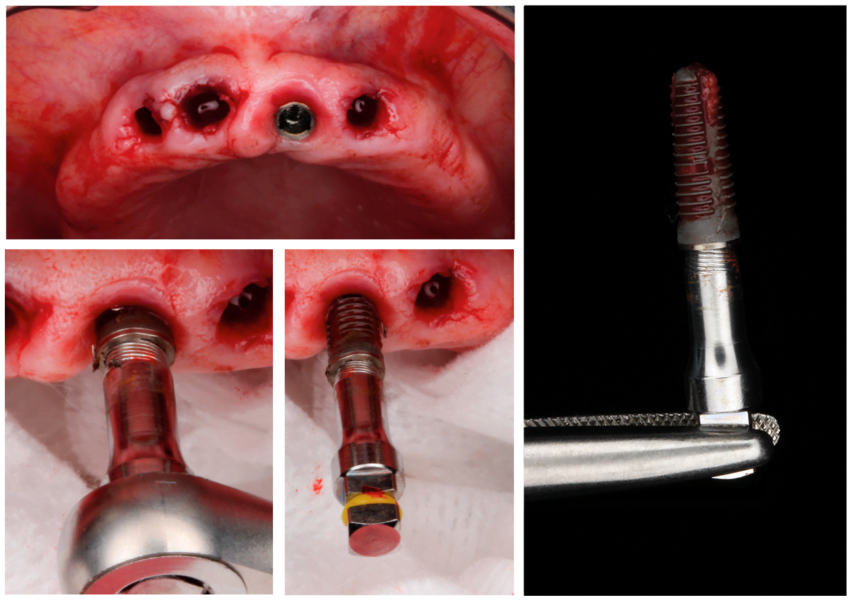
In a case where a patient presents for edentulation of the maxillary arch and requires a conventional denture with a single integrated implant at site No. 9, the surgical approach may vary depending on factors such as implant brand compatibility. In this scenario, if the implant being removed is of a different brand and line than what the surgeon typically has access to, the insertion driver reversal technique may not be feasible.
Instead, the surgeon may opt to use a fixture removal kit, which is universal and not dependent on the implant’s connection type. These kits typically include fixture removal tips of various sizes (narrow, regular, wide) to accommodate different implant dimensions.
Identifying signs of implant failure sets the stage for timely intervention, safeguarding against further complications and preserving oral health.
During the procedure, the appropriate-sized fixture removal tip is selected based on the size of the implant. In cases where the widest available tip is not sufficient, a pro tip suggests that the surgeon can modify narrower tips by cutting off the ends to convert them into larger widths.
The chosen fixture removal tip is then turned counter-clockwise into the implant connection until it cold welds into place. Subsequently, a long, non-breaking torque wrench is attached, and the implant is gently removed in a counter-clockwise direction using a non-invasive technique. This method allows for the safe and effective removal of the implant without compromising surrounding bone or tissue (Figures 4A-4D).
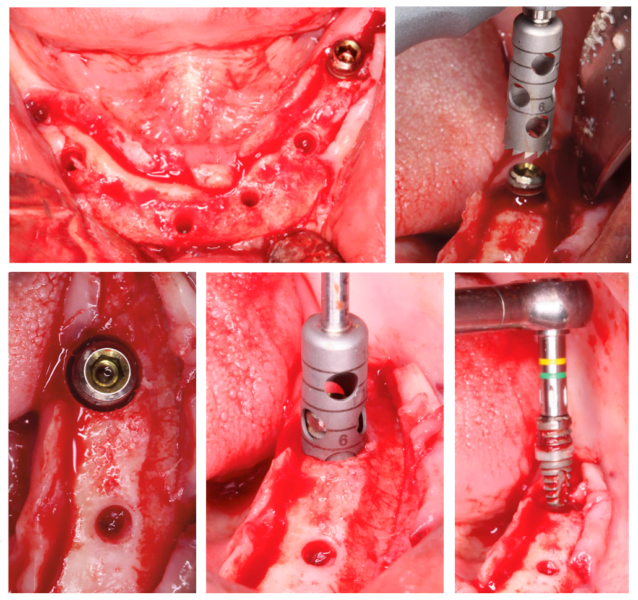
Trephine removal for full arch revision
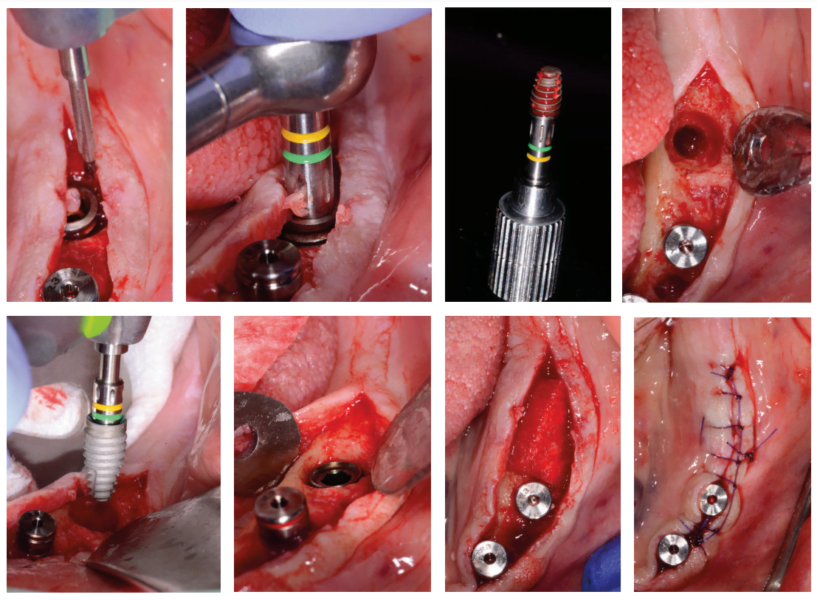
In a case where a patient presented with a completely failing lower fixed arch necessitating revision surgery, the majority of implants were successfully removed using traditional reverse torque techniques due to bone loss and infection. However, implant No. 19 posed a challenge as it was integrated and resistant to atraumatic removal methods.
To address this issue, a trephine drill from Meisinger USA was selected, ensuring it was just large enough to fit over the implant diameter. Depth markers on the trephine drill allowed for precise depth control, and a preoperative CBCT scan was consulted to ensure a safe distance from the inferior alveolar nerve (IAN).
Carefully utilizing the trephine drill to half the length of the implant while maintaining control over the depth avoids any complications with vital structures. Subsequently, reverse torque was successfully achieved using the insertion driver, allowing for the safe removal of the integrated implant.
Following the successful removal of implant No. 19, the surgery proceeded with a traditional All-on-4 revision approach. This case highlights the importance of utilizing appropriate tools and techniques to address challenging scenarios in implant dentistry, ensuring optimal outcomes for the patient (Figures 5A-5E).
Conclusion
In the realm of implant dentistry, the journey from removal to renewal embodies both challenge and opportunity. As we’ve explored the intricate process of addressing failed dental implants, it becomes evident that each case presents a unique puzzle, demanding a tailored approach for optimal resolution.
The pivotal role of early recognition cannot be overstated. Identifying signs of implant failure sets the stage for timely intervention, safeguarding against further complications and preserving oral health. Moreover, embracing failed implants as learning opportunities propels us towards continuous improvement, refining our strategies and enhancing patient care.
Surgical techniques, ranging from conservative to aggressive, offer a spectrum of options for implant removal. Yet, it’s the artful application of these techniques, guided by patient-specific considerations, that truly defines success. From the delicate precision of trephine drills to the strategic finesse of fixture removal kits, each tool in our arsenal serves a purpose, sculpting the path towards restoration.
Crucially, the journey doesn’t end with removal. Post-removal rehabilitation emerges as a cornerstone, fostering an environment conducive to successful implant osseointegration and long-term stability. Through meticulous debridement and thoughtful preparation, we lay the groundwork for the next phase of the patient’s journey – renewal.
In our case examples, we’ve witnessed the transformative power of these principles in action, guiding patients from complication to resolution, from uncertainty to confidence. It’s a testament to the artistry and science of modern implant dentistry, where innovation meets compassion in pursuit of patient well-being.
As we navigate the complexities of implant management, let us remain steadfast in our commitment to excellence. By staying attuned to emerging technologies, sharing insights within our professional community, and nurturing a culture of continuous learning, we equip ourselves to meet the evolving needs of our patients with unwavering skill and dedication.
In the end, it’s not merely about extracting and replacing failed dental implants — it’s about revitalizing smiles, restoring function, and enriching lives. It’s about embracing the journey, with all its challenges and triumphs, and forging ahead with confidence, knowing that each step brings us closer to our shared goal: the pursuit of dental excellence and patient well-being.
Besides implant removal, Dr. Vorholt has shared his expertise on suturing during dental implant surgery. Subscribers can read the article and pass the quiz to obtain 2 CE credits! https://implantpracticeus.com/ce-articles/the-importance-of-suturing-in-dental-implant-surgery/
References
- Young L, Brown T, Lamont TJ. A comparison of techniques for the explantation of osseointegrated dental implants. Evid Based Dent. 2020 Dec;21(4):126-127.
- Roy M, Loutan L, Garavaglia G, Hashim D. Removal of osseointegrated dental implants: a systematic review of explantation techniques. Clin Oral Investig. 2020 Jan;24(1):47-60.
- Tafuri G, Santilli M, Manciocchi E, Rexhepi I, D’Addazio G, Caputi S, Sinjari B. A systematic review on removal of osseointegrated implants: un update. BMC Oral Health. 2023 Oct 13;23(1):756.
- Stajčić Z, Stojčev Stajčić LJ, Kalanović M, Đinić A, Divekar N, Rodić M. Removal of dental implants: review of five different techniques. Int J Oral Maxillofac Surg. 2016 May;45(5):641-648.
- Solderer A, Al-Jazrawi A, Sahrmann P, Jung R, Attin T, Schmidlin PR. Removal of failed dental implants revisited: Questions and answers. Clin Exp Dent Res. 2019 Aug 21;5(6):712-724.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Steven Vorholt, DDS, graduated with a dental degree from The Ohio State University in 2013. Shortly after graduation, Dr. Vorholt started a private practice in the Columbus area. Immersing himself in as much continuing education as possible, he quickly developed a great passion for dental implant surgery. After building a successful general practice in Ohio, Dr. Vorholt followed his passion and moved to Arizona in 2020 to accept a full-time position with Implant Pathway helping to educate over 1,000 dentists place over 15,000 implants on their paths with implant dentistry.
Steven Vorholt, DDS, graduated with a dental degree from The Ohio State University in 2013. Shortly after graduation, Dr. Vorholt started a private practice in the Columbus area. Immersing himself in as much continuing education as possible, he quickly developed a great passion for dental implant surgery. After building a successful general practice in Ohio, Dr. Vorholt followed his passion and moved to Arizona in 2020 to accept a full-time position with Implant Pathway helping to educate over 1,000 dentists place over 15,000 implants on their paths with implant dentistry.

