Educational aims and objectives
This clinical article aims to discuss a case where complex procedures were used to provide an esthetic implant-borne restoration in order to meet high patient expectations.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article.
Take the quiz by clicking here.
Correctly answering the questions will demonstrate the reader can:
- Identify the treatment-planning process involved in providing this patient with a biomimetic restoration.
- Identify several potential options for this patient’s treatment.
- Realize the treatment objectives.
- Realize the steps for the implant placement and connective tissue graft.
- Realize the protocols followed for the restorative phase.
- Identify some necessary plans for this patient’s future care.
Dr. Rory McEnhill describes the treatment and compliance that led to positive biomimetic results and ultimately an esthetic, long-term outcome.
Dr. Rory McEnhill demonstrates the difficult process of providing an implant restoration that can offer outstanding esthetics for the long term
Background

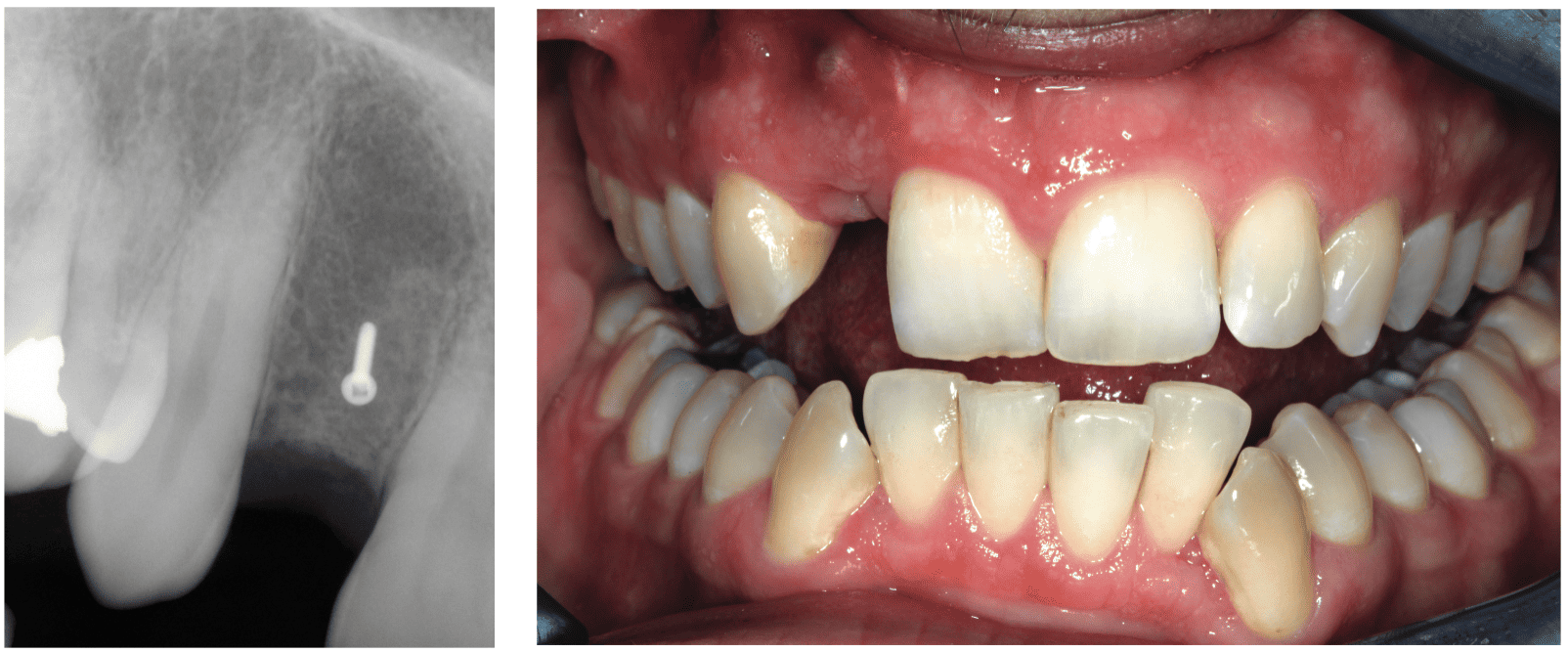
This patient presented with a missing UR2. He was a young man and had already worn a flipper denture and an adhesive bridge. Neither of these treatment options had brought him any satisfaction. In addition, they had been unpredictable with the denture breaking and the adhesive bridge debonding.
This patient’s key clinical features were:
- Upper anterior gap UR2
- Huge hard tissue volume defect
- Good gingival biotype despite some volume loss
- Good interarch space
The patient was referred to the practice in order to deal with the functional and esthetic issues relating to his missing upper right lateral incisor. Examination of his dentition highlighted that everything was healthy and that the sole and primary focus of his treatment would be to provide a biomimetic approach to restore the UR2 site back to its original state. This would involve hard tissue grafting as well as soft tissue bulking.
The patient was very clear about what he wanted to achieve. He wanted a predictable, long-term esthetic solution that would be fixed and permanent. Despite his reticence toward denture and adhesive bridges, we discussed their merits again. However, due to his age, he was willing to undertake the more complex solution, which was to provide the implant. He understood that this would involve bone harvested from the chin and grafted, connective tissue graft, and implantation. He understood the time scale would be approximately 8 to 9 months and was happy to wear an Essix retainer for this period of time.
The patient attended for a primary hygiene appointment to ensure optimum gingival health prior to surgery. We had assessed from the CT scan that a concurrent implant and bone graft was not possible, as the hard tissue defect was too large, and the implant would have been placed outside the protective environs of the bony envelope.
The bone graft was carried out using the Khoury technique using a tunnel flap. The implant was then placed 3 months later, and a connective soft tissue graft was carried out at the same time. Following 3 months of further healing, an apically repositioned flap was used to expose the implant, and a series of temporary crowns was used to sculpt the soft tissue, prior to a final screw-retained implant crown being fabricated.
Examination and assessment
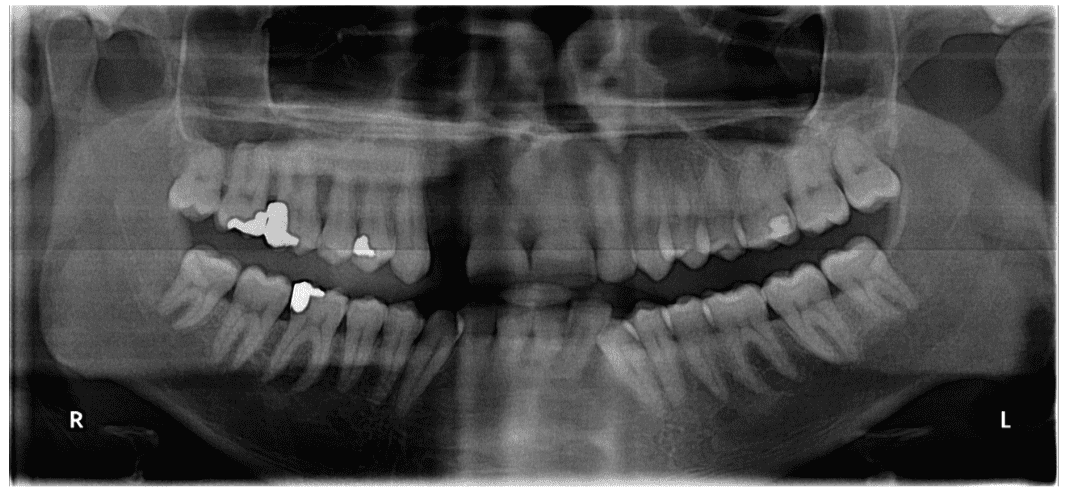
The patient had no significant medical history or dental issues beyond the missing UR2. He had lost this tooth 5 years previously: He had a post crown that endured a root fracture, which was responsible for the bony destruction. Preoperative radiographs highlighted his excellent bone health generally. In the UR2 position, the bone levels could be seen to be diminished. A subsequent CT scan highlighted the bone quality at the donor site and also the size of the defect in the recipient site. A diagnosis of missing upper right lateral incisor with associated hard and soft tissue volume loss was made.
Treatment discussion and planning
The patient was insistent on having an implant-based solution. He wanted to restore this site to what it was pre-tooth loss. Ideally, he wanted the implant to be indistinguishable from his natural teeth.
He understood that the treatment plan would be an involved, complex one but due to his age was very happy to invest his time, effort, and finances into fixing the issue definitively.
The patient was offered several options for treatment:
- New permanent denture
- Adhesive bridge
- Conventional cantilevered bridge
- Implant with hard/soft tissue grafting
He confirmed his desire to go for the fourth option.
This patient was an ideal candidate for treatment. He was very motivated and ambitious with regard to the final result. He was willing to undergo difficult treatments to achieve the ideal esthetic result.
The treatment objectives were therefore:
- To restore the upper right lateral incisor
- Biomimetic reinstitution of hard/soft tissues
- Perfect color match of implant restoration
Treatment
Following the initial consultation, where the patient’s hopes and expectations were established, he was referred to the in-house hygienist. Impressions were taken for a temporary adhesive bridge that the patient could wear during treatment. Due to the fact that a bone graft was to be carried out, no direct pressure was to be applied to the healing graft site. A CT scan was also taken of the upper and lower jaws at this point too. These views allowed us to assess the donor and recipient sites.
The chin was decided on as the donor site, due to the thickness of the soft tissue there, making gum recession less likely. The incisors were short, and the incisal branch of the inferior dental nerve was not close, meaning that paresthesia of the incisors was unlikely. In addition, this patient retained his lower wisdom teeth diminishing the retromolar/ramus sites as less attractive. The palate was also considered, but the roots were uncomfortably close to the palatal side, as well as the palate being relatively shallow. The long-term paresthesia of the incisive papillae was a negative aspect too.
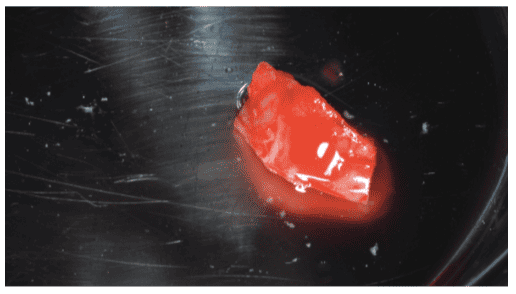
The UR2 site was exposed with one vertical relieving incision with the intention of carrying out a tunnel graft. The site defect was measured, and this value was used to guide us in the harvesting of the chin block. The bone was harvested using a micro saw, ensuring that the bony window was cut with beveled edges. This allowed us to tap the bone plate out with a chisel. Collagen was placed into the defect. Internal 6.0 Vicryl® sutures and external Vicryl interrupted sutures were used to close the donor site up.
The graft was then cut in half lengthways using the Khoury technique. This produced two rectangular bone blocks, one of which was used as the new buccal plate and the other which would be used to fill in the gap between the defect and the new buccal plate. To achieve this aim, a safe bone scraper was used to thin out the samples.
The principal reason for the success of the Khoury technique is the large surface area of the graft, as opposed to a bone block, which has a low surface area. Angiogenesis consequently occurs much more rapidly, and osteoclastic activity is thus dramatically reduced as the grafted bone is revascularized rapidly. In addition, the harvested bone has a high osteoinductive and osteogenic capacity.
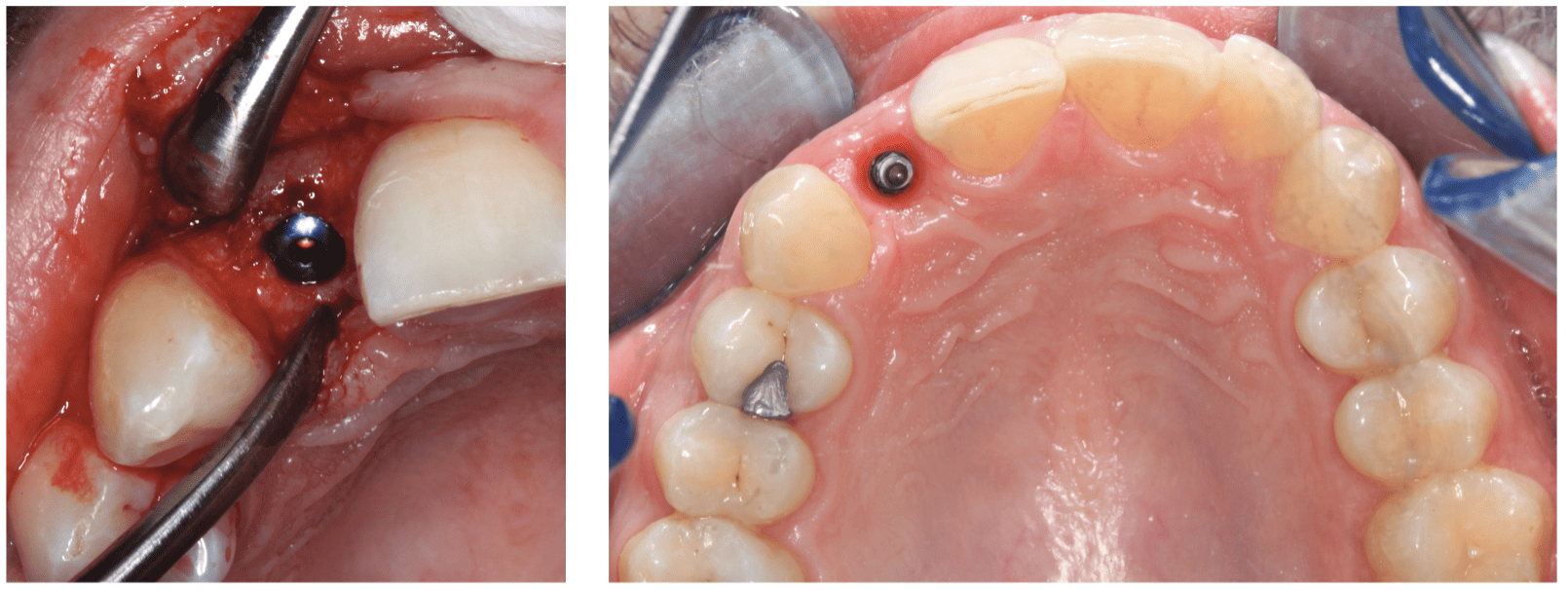
The autogenous bone plate is then trimmed and adjusted to fit the defect intimately, the rough edges are rounded, and a 1.0 mm bone screw was used to fix the plate into position. The harvested cancellous/cortical bone was packed into the defect to fill up the remaining voids. The soft tissue was then reflected back and sutured up with 4.0/6.0 Vicryl. The graft was left for 3 months to mature prior to implant placement.
Implant placement and connective tissue graft
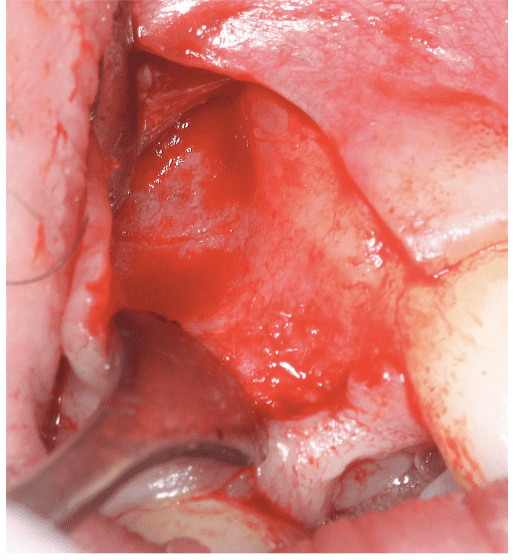
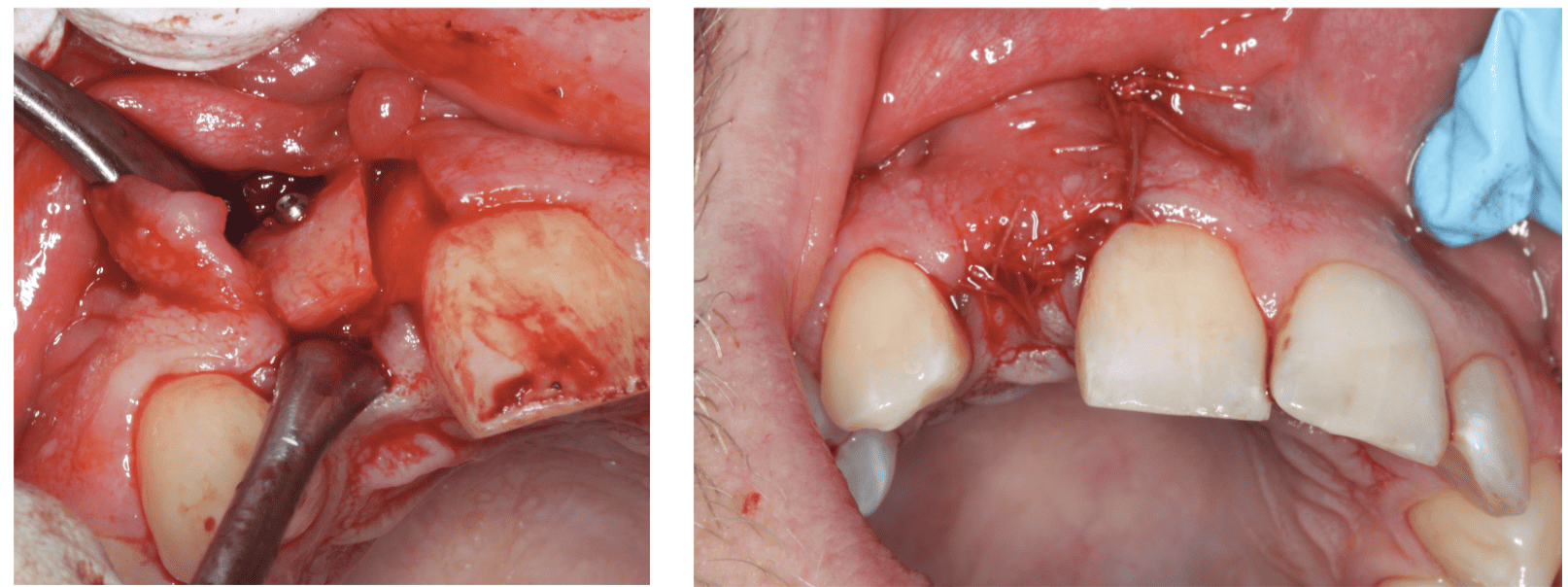
A full thickness flap with two vertical relieving incisions was carried out to expose the graft. The graft was massively revascularized and was red and oozing blood. The bone screw was removed, and the width of the ridge was now 8 mm. Ideally, at least 2 mm of buccal bone and 2 mm of palatal bone are required for predictable long-term implant placements. In this case, there was 3 mm of buccal bone once we had placed a MegaGen AnyRidge® 3.5 x 11.5 mm implant. To bulk up the tissue volume, a connective tissue graft was harvested from the palate, and this was packed into the site and the flap closed over. The site was allowed to heal for 3 months.
Restorative phase
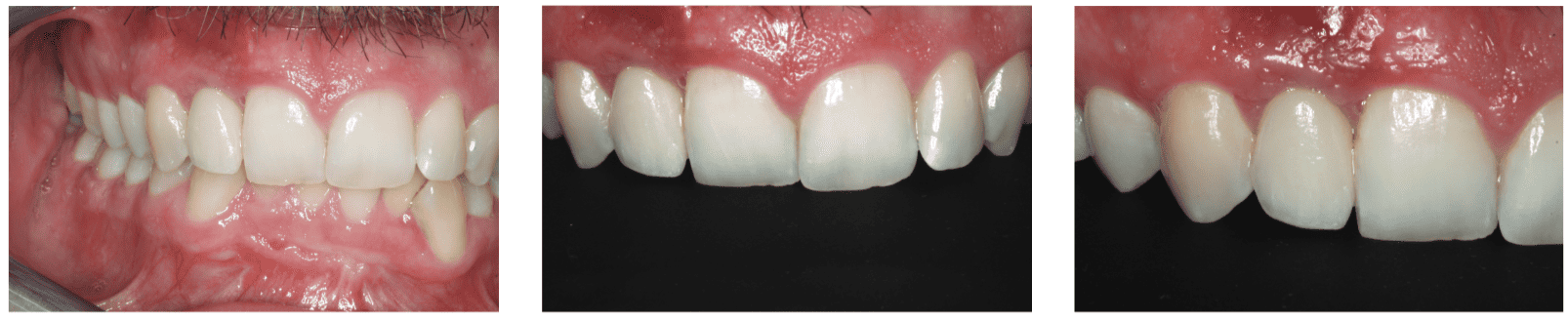
After 3 months of implant integration and soft tissue healing, an apically repositioned flap was carried out to improve the buccal soft tissue bulk further. A sulcus former was placed, and the soft tissue was left to heal for 1 month.
Open-tray impressions were taken to fabricate a screw-retained temporary restoration. This was due to the fact that the soft tissue needed to be sculpted further. The temporary crown had a bulbous buccal emergence profile to effect apical movement of the soft tissue. Following this process, a new open-tray impression was taken, and a porcelain screw-retained crown was fabricated and torqued into position.
The 1- and 3-month review appointments were held to assess a number of potential issues and to assess that the patient was cleansing the site effectively. In addition, photos were taken at the 1- and 3-month appointments for our clinical records.
The patient was informed of the importance of maintaining gingival health and was advised to attend with his hygienist quarterly.
Conclusion
This was a very demanding case. To provide biomimetic dentistry is a high tariff treatment.
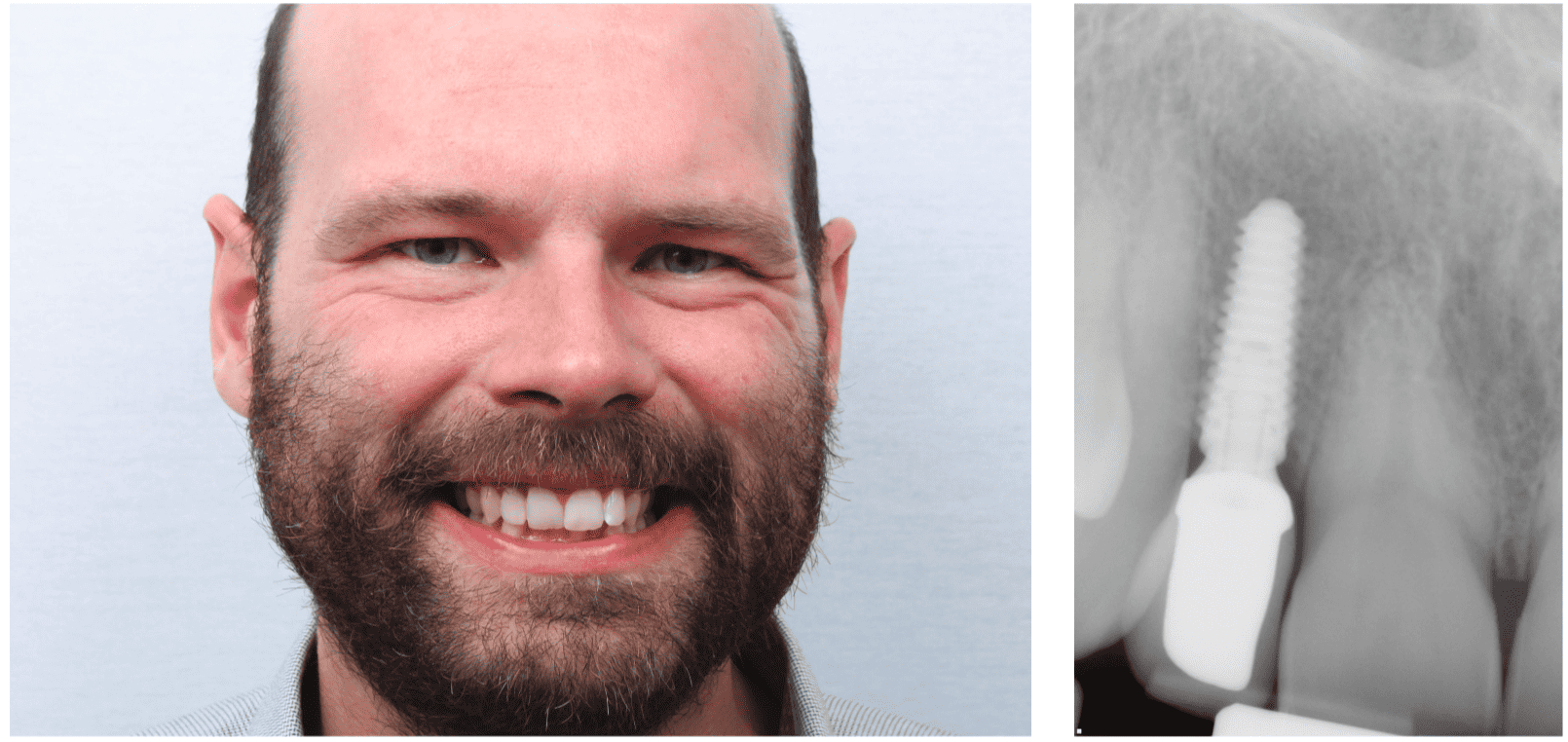
The treatment was very successful on a number of fronts. The goal to achieve a biomimetic result has been achieved with hard and soft tissue redevelopment being very successful. The implant has been restored with a porcelain restoration that is an excellent color match and blends in very harmoniously.
Plans for future care include:
- Implant monitoring appointments
- Biannual hygiene appointment with his GDP.
In terms of the clinical issues, this was a case that worked out due to good clinical planning. A methodical treatment plan allowed us to develop this case systematically. By putting in the hard and soft tissue foundations and tissue sculpting with temporary restorations, we were able to achieve an excellent result.
With regard to the final esthetics, the author feels that the final result is very satisfying, as the soft tissue profile and tooth symmetry are all harmonious and blend well into this patient’s smile.
Achieving biomimetic results takes detailed diagnostics focused on both function and esthetics. Check out Drs. Sajid Jivraj, Mamaly Reshad, and Winston Chee’s article titled, “Treatment planning of implants in the esthetic zone: part 1”.
References
- Khoury F, Antoun H, Missika P. Bone augmentation in oral implantology. Quintessence, UK; 2006.
- Kuchler U, von Arx T. Horizontal ridge augmentation in conjunction with or prior to implant placement in the anterior maxilla: a systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):14-24.
- Levine RA, Huynh-Ba G, Cochran DL. Soft tissue augmentation procedures for mucogingival defects in esthetic sites. Int J Oral Maxillofac Implants. 2014;29(suppl):155-185.
- Ritter RG. Multifunctional uses of a novel ceramic-lithium disilicate. J Esthet Restor Dent. 2010;22(5):332-341.
- Tonelli P, Duvina M, Barbato L, et al. Bone regeneration in dentistry. Clin Cases Miner Bone Metab. 2011; 8(3):24-28.



