Dr. Daniel S. Thoma outlines the treatment undertaken for a patient with fractured central incisors using ridge preservation
Dr. Daniel S. Thoma outlines the treatment undertaken for a patient with fractured central incisors using ridge preservation
A 52-year woman presented with pain in her two central incisors. The patient had fractured both central incisors in her youth. They were subsequently restored with two porcelain-fused-to-metal crowns (Figure 1). At the day of the first examination, CBCT analysis and clinical inspection revealed that tooth UR1 was endodontically treated and had increased periodontal pocket depths with bleeding on probing.
Several treatment options were discussed following the tooth’s extraction:
Crown UL1 with a cantilevered UR1
Fixed dental prostheses UR2 to UL1
Implant placement at UR1 and new crown UL1
A decision was taken to opt for the third treatment modality, which included the replacement of tooth UR1 with a dental implant.
Pre-surgical phase
A full wax-up for teeth UR1 and UL1 was performed on casts by the dental technician to optimize the esthetic outcome prior to implant therapy. This wax-up was transferred to a mock-up that was tried-in intraorally.
Surgical phase
Two weeks later, tooth UR1 was carefully extracted without damaging the surrounding tissues and leaving the papillae intact. The epithelium at the extraction socket was removed using a diamond bur. Subsequently, the height of the buccal and palatal bone plate was measured with a periodontal probe. This revealed that, while on the buccal side the bone plate was almost fully present, the palatal height was reduced by 40%.
 According to Jung and colleagues (2013), a ridge preservation procedure allows bone volume to be maintained by 80% over 6 months. For that reason, a ridge preservation procedure was defined as being appropriate for optimizing the clinical situation, including the hard and soft tissue aspects.
According to Jung and colleagues (2013), a ridge preservation procedure allows bone volume to be maintained by 80% over 6 months. For that reason, a ridge preservation procedure was defined as being appropriate for optimizing the clinical situation, including the hard and soft tissue aspects.
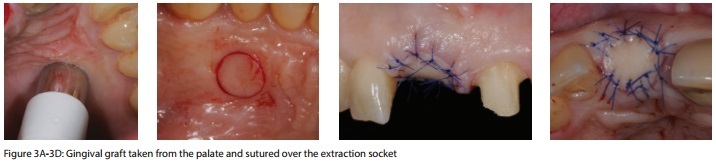
The treatment (Figure 2) consisted of placement of a collagen sponge consisting of 10% collagen and deproteinized bovine bone mineral (DBBM) granules, and a soft tissue punch. The bone substitute material was placed within the extraction socket flush with the bone crest on the buccal side, and exceeding the palatal bone plate by roughly 4 mm and to a level of 3 mm below the mucosal margin. Subsequently, a free gingival graft (FGG) with a thickness of 3 mm and a diameter of 8 mm was harvested at the palate.
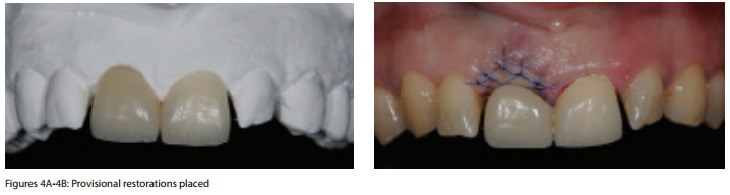
This FGG was sutured on top of the extraction socket using non-resorbable sutures (Figure 3) in keeping with the method described by Jung, Siegenthaler, and Hämmerle (2004). The crown on tooth UL1 was removed and replaced with a provisional restoration including a cantilever to replace tooth UR1 (Figure 4).
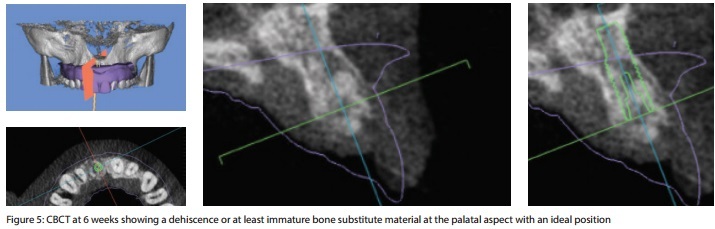
Six weeks later, the clinical situation was healthy, and the former extraction socket was completely closed. A CBCT was taken to assess the bone dimension and to decide whether or not implant placement could be performed.
The CBCT revealed that, with an ideal implant position, a dehiscence defect at the palatal aspect would be present. Due to the fact that guided bone regeneration (GBR) on the palatal side cannot be performed predictably, a longer healing time was discussed with the patient.
Four months later, a second CBCT was taken (Figure 6), and again, the implant position was defined using digital planning software (SMOP Swissmeda AG, Switzerland). A digital scan of the initial clinical situation was matched and superimposed with the CBCT data in the planning software. At this point, the height of the palatal and buccal bone plates returned to a regular height. Bone regeneration had taken place, and the former extraction socket was completely filled with bone substitute material and newly formed bone. This allowed implant surgery planning and the production of a surgical stent for guided surgery.
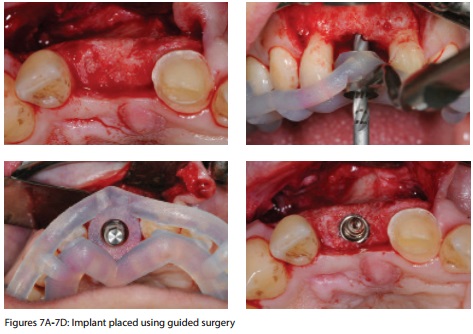
 On the day of implant placement, a full thickness flap was elevated, and a dental implant (Bone Level, Straumann®) was placed using guided surgery, and a surgical guide printed using a three-dimensional printer. The implant was placed in an ideal position, vertically and horizontally (Figure 7).
On the day of implant placement, a full thickness flap was elevated, and a dental implant (Bone Level, Straumann®) was placed using guided surgery, and a surgical guide printed using a three-dimensional printer. The implant was placed in an ideal position, vertically and horizontally (Figure 7).
In order to compensate for an expected loss of volume on the buccal side, GBR with DBBM and a resorbable collagen membrane was performed to optimize the contour (Figure 8). Primary wound closure was obtained. Three months later, the clinical situation revealed a slight loss of the buccal contour. According to a recent clinical study on 16 patients, GBR may contribute for up to 57% of the volume, whereas soft tissue augmentation compensates the remaining 43% of the volume deficiency (Schneider, et al., 2011).
Soft tissue volume augmentation surgery was performed using a classic approach (Figure 9). The patient agreed to be part of an ongoing clinical study comparing autogenous soft tissue grafts to a prototype three-dimensional collagen matrix. For that purpose, a split thickness flap was elevated, a pouch on the buccal aspect of the implant site prepared, and a three-dimensional collagen matrix inserted and sutured in place. Again, primary wound closure was obtained.

 Three months later, abutment connection was performed using a U-shaped incision, and the preparation of a small flap was placed underneath the buccal flap. Following an impression with a standardized impression post, a healing abutment was inserted.
Three months later, abutment connection was performed using a U-shaped incision, and the preparation of a small flap was placed underneath the buccal flap. Following an impression with a standardized impression post, a healing abutment was inserted.
Prosthetic phase
After 1 week, a provisional implant-borne reconstruction with a full contour on the buccal side and a concave contour within the soft tissues was inserted (Figure 10). Within two to three appointments, flowable composite was added to the trans-mucosal part of the provisional restoration (at the implant site) to aim for a more convex contour and to create the emergence profile, mimicking one of the neighboring contra-lateral teeth UL1.
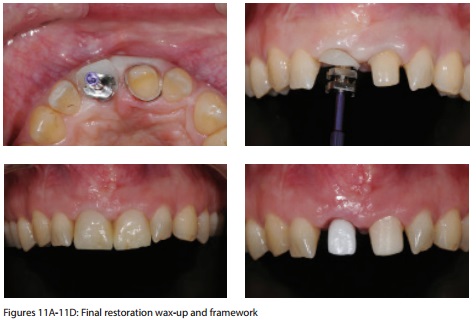
After a healing period of 3 months, an individual impression post was prepared, and an impression was taken for implant UR1 and tooth UL1. The dental technician fabricated a try-in wax-up, which was inserted during the following appointment. Subsequently, an all-ceramic reconstruction based on a zirconia abutment (Cares®, Straumann) for implant UR1 and an all-ceramic single crown for tooth UL1 were prepared by the dental technician (Figure 11). The implant-borne reconstruction was screw-retained and inserted with an insertion torque of 35Ncm. The access hole was closed with composite. The all-ceramic crown on tooth UL1 was cemented with a resin cement.
One week later, the patient was recalled for the follow-up examination. The clinical situation was healthy; no bleeding on probing was observed. The final outcome was judged as being esthetically pleasing, and the patient scheduled for a regular maintenance program.
Final outcome
The final outcome of the case (Figure 12) was considered to be excellent from an esthetic and functional point of view, and the patient was satisfied with the results. The ridge preservation procedure performed at the day of tooth extraction allowed for further optimal implant position and enhanced the clinical situation on the hard and soft tissue level, but prolonged the overall treatment time. GBR and soft tissue volume augmentation contributed almost equally to the volume obtained at the end of the treatment.
The reconstructions manufactured by a skilled dental technician were based on all-ceramic materials, which, in this clinical situation, demonstrated high long-term survival and success rates.