Dr. Charlotte Stilwell assesses the strategic use of implant overdenture abutments with removable partial dentures
Missing teeth have an enormous impact on psychosocial and physical well-being. As dentists, we have an important role in helping afflicted individuals improve their quality of life.
Educational aims and objectives
This clinical article aims to present the current evidence relating to the use of dental implants with removable partial dentures (RPDs).
Expected outcomes
Implant Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize the rationale for using implant overdenture abutments in combination with RPDs and the suggested approach for their use.
- Realize the advantages and disadvantages of RPDs.
- Recognize the strategic use of implants for support and/or retention.
- Identify some strategic implant configurations for RPDs.
 Conventional fixed and removable prosthodontic solutions are increasingly assisted by the strategic advantages that implant therapy can offer. There has been consensus agreement since 2002 (Feine, et al., 2002) that a complete denture retained by two implants should be regarded as the minimum standard of care for the edentulous mandible. Equally, for replacement of a single anterior tooth with adjacent virgin teeth neighbors in an otherwise sound dentition, an implant-supported crown is considered the evidence-based option of choice (Pjetursson and Lang, 2008). These two examples represent the extremes in the edentate spectrum. They also represent fairly clear-cut indications in favor of implant assistance. This is not always the case.
Conventional fixed and removable prosthodontic solutions are increasingly assisted by the strategic advantages that implant therapy can offer. There has been consensus agreement since 2002 (Feine, et al., 2002) that a complete denture retained by two implants should be regarded as the minimum standard of care for the edentulous mandible. Equally, for replacement of a single anterior tooth with adjacent virgin teeth neighbors in an otherwise sound dentition, an implant-supported crown is considered the evidence-based option of choice (Pjetursson and Lang, 2008). These two examples represent the extremes in the edentate spectrum. They also represent fairly clear-cut indications in favor of implant assistance. This is not always the case.
Prosthodontic treatment planning is a multifactorial exercise in addressing and satisfying the wishes and needs of the individual patient. The best option in some cases may therefore not be a choice between conventional and implant-assisted options. It could also include a combination of options.
A particular and emerging example of such prosthodontic combinations is the indication for the strategic use of implants in the prosthodontic area of removable partial dentures (RPDs). This article will discuss the treatment planning principles for RPDs in general and the advantages that may be offered by combining RPDs with implant therapy.
RPDs: a gray area in dentistry
RPDs are traditionally associated with lower patient satisfaction and a potential negative impact on oral health.
 The biological risks to the remaining dentition, in general, and to abutment teeth, in particular with ensuing tooth loss, are extensively documented in the literature. RPDs also represent a particular professional challenge. Each partially edentulous dentition is unique (Figures 1A-1C) and requires bespoke design and construction for the RPD to be really effective and acceptable.
The biological risks to the remaining dentition, in general, and to abutment teeth, in particular with ensuing tooth loss, are extensively documented in the literature. RPDs also represent a particular professional challenge. Each partially edentulous dentition is unique (Figures 1A-1C) and requires bespoke design and construction for the RPD to be really effective and acceptable.
In the RPD situations with free-end saddles, these also require an understanding (on the part of both clinician and dental technician) of how best to compensate for missing strategic tooth support. The difference in resilience between teeth and soft tissues must be reconciled to achieve a functional and stable RPD.
RPDs may be seen as the economical prosthodontic solution, but they remain a mainstay of prosthodontic care for partially edentulous patients. If appropriately designed, they can be a comprehensive, effective, and successful prosthodontic rehabilitation (Lynch, 2012).
RPD indications
A literature review from 2005 (Wostman, et al., 2005) concluded that there were no evidence-based indications per se. The published literature only offers limited treatment planning principles to assist clinical decision making for RPDs.
In support of choosing RPDs, the literature lists the presence of sound abutment teeth and/or the need for lower cost prosthodontic solutions. Against RPDs are the presence of individual risks factors for biological complications, caries and periodontal disease, and lack of patient acceptance.
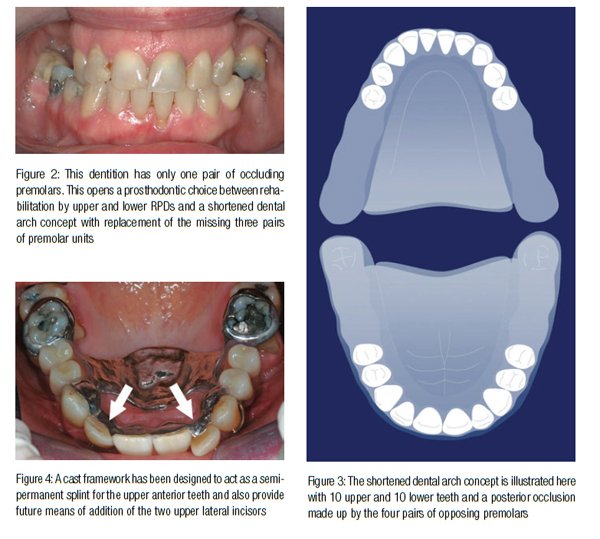
A particular contraindication for RPDs is the presence of — or potential for (Figure 2) — a sound and stable shortened dental arch occlusion (SDA) (Kaeser, 1989) (Figure 3).
In patient cases where an SDA configuration will provide adequate esthetics and function, the SDAs have been shown to perform well and last in excess of 27 years (Gerritsen, et al., 2013). Additional replacement of missing posterior teeth with free-end saddle RPDs is not recommended for these cases.
Prosthodontic advantages of conventional RPDs
In spite of the limited literature support for RPDs, there are undoubtedly clinical situations where RPDs are both indicated and able to offer significant advantages over other options. Based on empirical experience these include (Stilwell, 2010):
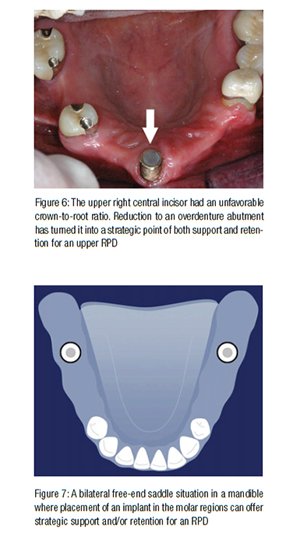
Design versatility. In the presence of teeth with a guarded prognosis, the RPD can be designed with addition of these in mind. Equally, in the event of mobile teeth, the RPD can serve as a semi-permanent splint. This is illustrated in Figure 4.
 Replacement of lost hard and soft tissue contours. A carefully constructed and tinted RPD acrylic flange can make up for missing volume in the alveolar process. This also allows the RPD teeth to emerge in harmony with the remaining natural teeth as seen in Figure 5. This is a noninvasive and, in some cases, more predictable alternative to surgical hard and soft tissue augmentation procedures.
Replacement of lost hard and soft tissue contours. A carefully constructed and tinted RPD acrylic flange can make up for missing volume in the alveolar process. This also allows the RPD teeth to emerge in harmony with the remaining natural teeth as seen in Figure 5. This is a noninvasive and, in some cases, more predictable alternative to surgical hard and soft tissue augmentation procedures.
Strategic use of overdenture abutments. For teeth that have an unfavorable crown-to-root ratio, a reduction to gingival level can improve their prognosis. As over-denture abutments, they will still provide valuable support and thereby can be of strategic value to avoid free-end saddles. They can also provide retention for the RPD; an example is seen in Figure 6.
Combining implants and RPDs
Similar to the support and retention that can be offered by teeth converted to overdenture abutments, there is emerging evidence that strategic implants can serve the same purpose. Two separate literature reviews (Shamiri and Atieh, 2010; de Freitas, 2012) have evaluated the effect of this type of implant assistance for uni- and bilateral free-end saddle RPDs (Figure 7).
The reviews looked at patient satisfaction, implant survival rates, and prosthetic complications and maintenance. Both reported limited but positive and promising evidence for a definite increase in patient RPD satisfaction. The data also indicated high implant survival rates and complications and maintenance that were comparable to those of RPDs in general.
As such, both reviews concluded that strategic use of implants for support and/or retention has great promise as a valuable advantage for free-end saddle RPDs and as a simple, economical, and less invasive prosthodontic treatment option for rehabilitation of the partially edentulous patient (Figure 8).
 Implant indications for RPDs
Implant indications for RPDs
The implant indications can be divided into the assistance they lend specifically to RPDs and the advantages they can offer for forward prosthodontic planning.
RPD assistance
This includes improvement of support, retention, and esthetics. An example of support is seen in Figure 8. A combined example of assistance with retention and esthetics can be seen in Figure 9 — a single strategic implant in the upper right canine site provides hidden but strategic advantages for the patient’s RPD.
Forward prosthodontic planning
This includes ridge preservation, single tooth replacement and gradual conversion to complete removable denture (CRD). The loss of a natural tooth is followed by an atrophy of the related alveolar process (Van der Weijden, et al., 2009). In turn, this atrophy is likely to be further aggravated by the pressure of a soft tissue-supported RPD saddle. The extent of this atrophy can be reduced if not arrested by early recognition and placement of an implant in the tooth site. A delayed realization may lead to a need for bone augmentation.
In a new patient, the clinical situation may not yet be suitable for implant placement. If so, the option of future implant placement can be facilitated by either maintaining the tooth in the short term as an overdenture abutment or by performing a ridge preservation procedure at the time of tooth removal.
Strategic implant configurations for RPDs
 For the planning of implant assistance for RPDs, it is helpful to consider the optimal RPD situation.
For the planning of implant assistance for RPDs, it is helpful to consider the optimal RPD situation.
The Kennedy classification is often used to describe partially edentate configurations. The optimal choice in this classification is a Class III where the RPD can derive support and/or retention from a tooth in each corner of the design; this situation is illustrated in the diagram in Figure 10.
In the Class I bilateral free-end saddle, Class II unilateral free-end saddle, and Class IV anterior saddle seen in Figures 11-13, the implants would take the place of the missing strategic teeth and convert the three examples back into Class III.
In planning for a gradual conversion to a CRD, it would seem sensible to aim for the recommended minimum implant configurations for full edentulous arches. The current recommendations are a minimum of two implants in the mandible and four implants in the maxilla (Gallucci, et al., 2014).
General considerations for implant therapy
The general treatment planning principles for implant therapy in combination with RPDs also apply to these indications. These include:
Risk factors
In common with treatment planning for implant therapy in general, the patient’s social, medical, and dental risk factors in remaining dentition should be considered. Risks posed to the outcome of implant therapy by, for example, smoking, diabetes, and periodontal disease may outweigh any strategic benefit.
History of previous implant complications with peri-implantitis or implant loss together with the patient’s motivation and ability to care for the implant, remaining natural teeth, and RPD are also important. Specific instruction and support may be needed for the elderly RPD patient.
Suitable conditions for implant placement
The atrophy of the edentulous alveolar processes in most long-standing RPD patients precludes adequate bone volume for safe placement. Early recognition prior to or soon after loss of an abutment tooth is therefore important to ensure that adequate hard and soft tissue conditions still exist.
The continuing improvements in implant surfaces and alloys may allow use of reduced diameter and/or shorter implants for the RPD indications, but the evidence for these options is limited at present.
 Hygienic and effective RPD design
Hygienic and effective RPD design
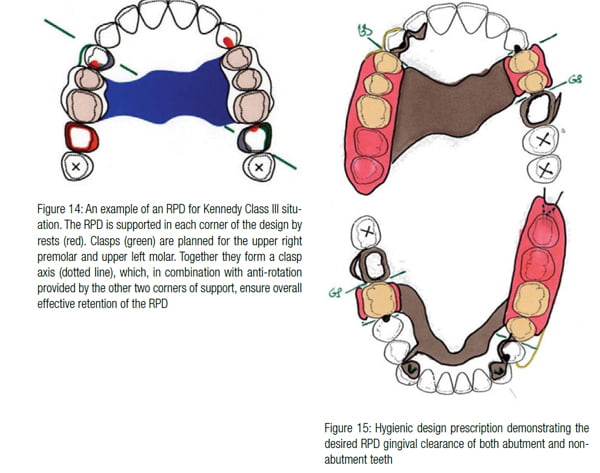
 The literature support for biomechanical RPD principles is at best ambivalent. However, it would seem logical that an RPD design should take advantage of the scope for tooth support and retention. An example of this for a Kennedy Class III configuration can be seen in Figure 14 with appropriate use of rests and clasps (Stilwell, 2010).
The literature support for biomechanical RPD principles is at best ambivalent. However, it would seem logical that an RPD design should take advantage of the scope for tooth support and retention. An example of this for a Kennedy Class III configuration can be seen in Figure 14 with appropriate use of rests and clasps (Stilwell, 2010).
By contrast, there is definite evidence that open hygienic RPD design can be of benefit to long-term health of teeth and soft tissues (Owall, 2002; Rehmann,et al., 2013).
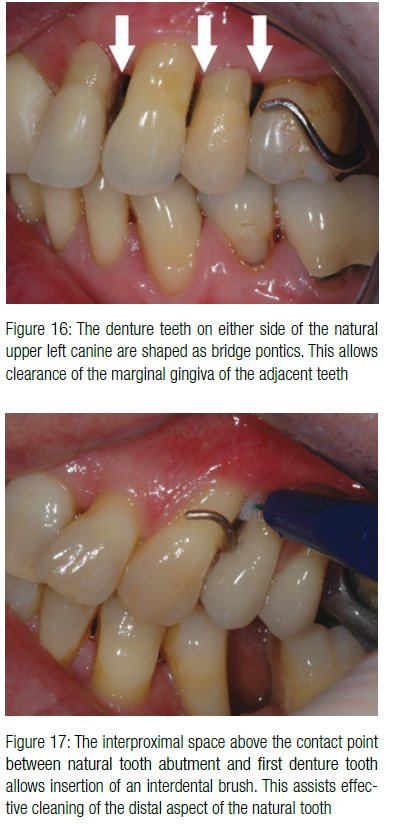
The denture components need to be designed, as seen in Figure 15, to reduce risks of tissue injury as well as providing gingival clearance. In the upper and lower RPD examples shown, the major connectors are kept away from both abutment teeth and non-abutment teeth, and there is an interproximal space below the contact points between the first denture tooth and the neighboring natural abutment tooth (Figure 16). The first denture tooth is shaped as a bridge pontic to mimic a natural interproximal space. This also allows access for interdental brushes even when the denture is in situ (Figure 17).
Implant prosthodontic options
A multicenter study (Wismeijer, et al., 2013) reported significant improvement in patient satisfaction between a conventional Kennedy Class I mandibular RPD and the same RPD supported by single strategic implants placed under each free-end saddle. Initially, traditional healing caps provided the support. A further significant increase in patient satisfaction was recorded when the healing caps were replaced by retentive anchors (ball attachments).
There are a range of attachments available; these include other types of retentive anchors and magnets (Figures 18 and 19). The choice of attachment is determined by the same factors that apply to any overdenture situation: space requirement, degree of desired retention, ease of use and cleaning, and cost.
 Patient example
Patient example
A partially edentate patient was first provided with an RPD in 1979. At the time, she had only seven upper natural teeth of her own. The extensive tooth loss at the early age of 32 had both shocked and motivated her to adopt optimal oral hygiene, and this was maintained forthwith.
The upper RPD had one unilateral free-end saddle (Class II) and used a molar and the two canines for support and retention via precision attachments. The RPD was successfully replaced in 1994, and after a further 16-year period, replacement was considered again in 2010.
At this point, concerns were arising about the longevity of the upper three precision attachment abutment teeth. Strategic implant placement was agreed to provide for eventual loss of the upper and lower RPD abutments and, at the same time, to carry forward the long-standing RPD abutment configuration. It was further agreed to also place an additional strategic implant in the upper left molar region to convert the upper RPD configuration to a Class III.
The implant situation can be seen in Figures 20 and 21 at the 5-year follow-up in 2015.
Summary and conclusions
This article has addressed the specific indications for strategic use of implants to provide support and retention for RPDs. There is emerging evidence that use of implants in this way offers positive functional and esthetic benefits and a significant increase in patient RPD satisfaction. The literature also suggests that it is a simple, economical, and less invasive use of the implant treatment modality.
The article suggests that the specific planning principle for use of strategic implants in combination with RPDs is to preserve or convert Kennedy Class I, II, and IV situations to more favorable Class III configurations. The article also explains that conventional prosthodontic and implant planning principles and considerations still apply.
Acknowledgment
International Team for Implantology (ITI) for modifiable graphics.
References
- de Freitas RF, de Carvalho Dias K, da Fonte Porto Carreiro A, Barbosa GA, Ferreira MA. Mandibular implant-supported removable partial denture with distal extension: a systematic review. J Oral Rehabil. 2012;39(10):791-798.
- Feine JS, Carlsson GE, Awad MA, et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants. 2002;17(4):601-602.
- Gallucci GO, Benic GI, Eckert SE, et al. Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants. 2014;29 (Suppl):287-290.
- Gerritsen AE, Witter DJ, Bronkhorst EM, Creugers NH. An observational cohort study on shortened dental arches — clinical course during a period of 27-35 years. Clin Oral Investig. 2013;17(3): 859-866.
- Kayser AF. Shortened dental arch: a therapeutic concept in reduced dentitions and certain high-risk groups. Int J Periodiontics Restorative Dent. 1989; 9(6):426-449.
- Lynch CD. Successful removable partial dentures. Dent Update. 2012;39(2):118-120, 122-126.
- Owall B, Budtz-Jörgensen E, Davenport J, et al. Removable partial denture design: a need to focus on hygienic principles? Int J Prosthodont. 2002;15(4):371-378.
- Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007;18 (Suppl 3):97-113.
- Rehmann P, Orbach K, Ferger P, Wöstmann B. Treatment outcomes with removable partial dentures: a retrospective analysis. Int J Prosthodont. 2013;26(2):147-50.
- Shahmiri RA, Atieh MA. Mandibular Kennedy Class I implant-tooth-borne removable partial denture: a systematic review. J Oral Rehabil. 2010;37(3):225-234.
- Stilwell C. Revisiting the principles of partial denture design. Dent Update. 2010;37(10): 682-684, 686-688, 690.
- Van der Weijden F, Dell’Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009;36(12):1048-1058.
- Wismeijer D, Tawse-Smith A, Payne AG. Multicentre prospective evaluation of implant-assisted mandibular bilateral distal extension removable partial dentures: patient satisfaction. Clin Oral Implants Res. 2013;24(1):20-27.
- Wöstmann B, Budtz-Jørgensen E, Jepson N, et al. Indications for removable partial dentures: a literature review. Int J Prosthodont. 2005; 18(2):139-45.



