Educational aims and objectives
This clinical article aims to discuss some of the risk factors and preventative measures for peri-implant disease.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article.
Correctly answering the questions will demonstrate the reader can:
- Understand how careful treatment planning can minimize the occurrence of peri-implantitis.
- Recognize some strategies for treatment of the disease.
- Realize some of the reasons for resective treatment.
- Identify some characteristics of the ideal implant surface and how to achieve those goals.
- Identify some essential features of the implant abutment connection for a positive implant protocol.
Risk factors for peri-implantitis can be recognized, and a broad range of therapies is available for its treatment. Read about how to treat this increasingly prevalent condition.
Drs. Ashok Sethi, Thomas Kaus, and Naresh Sharma examine risk factors and management of this increasingly prevalent condition
A rapid increase in the incidence of peri-implantitis has been reported. Prevalences up to 56% at patient level have been reported for periodontitis susceptible patients (Donos, et al., 2012; Heitz-Mayfield, et al., 2014; Monje, et al., 2016). However, incidences as low as 1% at implant level have also been reported (Monje, et al., 2016). This clearly indicates that there are various risk factors that influence the incidence of peri-implantitis.
These factors include known risk factors that predispose to periodontal disease such as poor oral hygiene, smoking, genetic susceptibility, and diabetes. Other factors may be considered iatrogenic such as poor implant placement where the implant is not wholly submerged in bone.
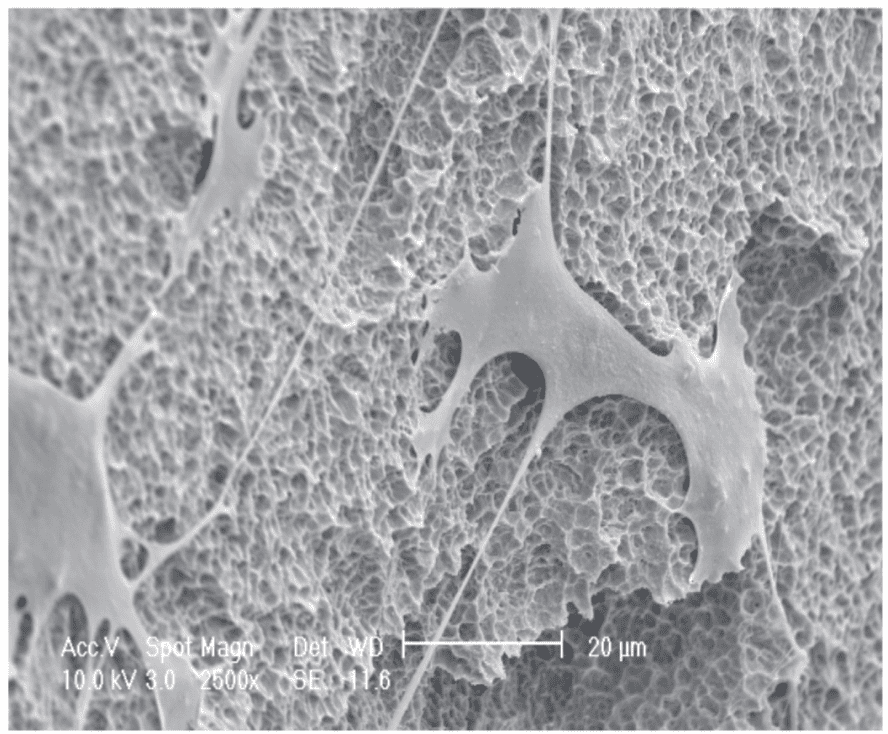
Other factors may be related to the implant. Modern implants are now produced with a rough surface to encourage contact osteogenesis (Figure 1) — in other words, direct deposition of bone by osteoblasts onto the implant surface (Davies 1998). This has considerable advantages such as rapid integration permitting reduced healing times and higher success rates. However, if the implant surface is exposed to bacteria, colonization and formation of biofilms are more likely to lead to peri-implantitis.
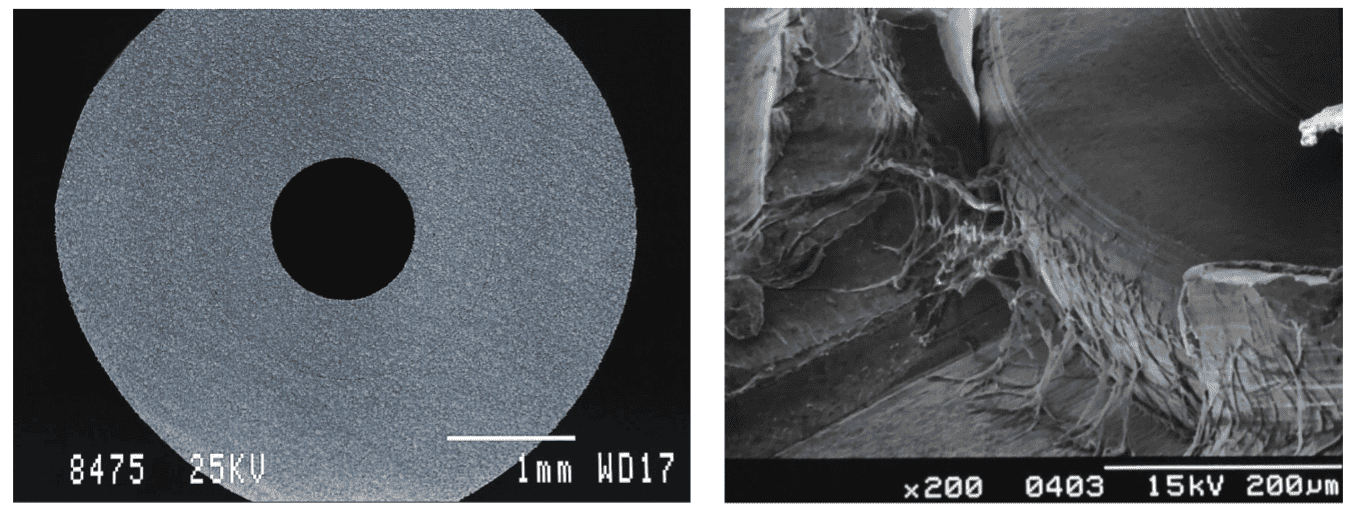
Other factors influencing the presence of bacteria in the peri-implant sulcus are determined by the leakage of bacteria from the abutment implant connection as well as the space between the prosthesis and the abutment. This is especially the case for screw-retained prostheses (Cosyn, et al., 2011; Gross, et al., 1999). The conical connection, however, is reported to be tight enough to prevent bacterial contamination (Figure 2) (Mairgunther and Nentwig, 1992; Sethi and Kaus, 2002).
Treatment of peri-implantitis
A broad range of therapies have been put forward for the treatment of peri-implantitis.
They essentially involve the removal of the biofilm and subsequent maintenance of the area with adequate oral hygiene protocols. The decision-making process will involve factors such as level of bone loss and the implant location. Three strategies are normally considered.
Resective treatment
Resective treatment involves the removal of the bacterial biofilm as well as any infected surrounding soft tissues. Some form of implant surface modification to remove any rough surfaces and/or threads is also deemed necessary (referred to as an implantoplasty). The aim of this is to re-establish direct soft tissue contact onto the implant surface. The disadvantage of this technique is exposure of the implant or abutment, which may prove to be an issue in the esthetic zone.
Regenerative therapy
Regenerative therapy is considered when the defect morphology permits it. Hard tissue regeneration may be attempted, which is fraught with the risk of recurrence and is challenging, often requiring the covering of the implant during the healing phase.
Retreatment
In circumstances where excessive bone loss has taken place and is progressive, retreatment may be considered. It is essential to identify the cause of the peri-implantitis prior to considering retreatment. This is most likely to involve bone grafting.
Prevention of peri-implantitis
There are a few general considerations regarding the successful prevention of peri-implantitis. From the outset, it is clear that all the systemic factors need to be favorable. The treatment of periodontal disease prior to implant therapy is therefore prudent. Ideally the removal of all sources of contamination should be implemented. Predisposing factors such as smoking should also be brought under control.
Susceptible patients should be informed and be aware of the risks and willing to maintain a high degree of hygiene. However, specific strategies also exist for the prevention of the disease. These strategies should be aimed at creating an environment where the risk of implant infection is reduced. They relate to choice of technique, implant/component features, and design of the restoration.
Implant
The ideal implant surface has been determined to be a rough surface to promote contact osteogenesis.
Surgical strategy, therefore, should be aimed at positioning the rough implant surface below the crestal bone to permit bone to grow over it, minimizing the risk of bacterial contamination. This, therefore, has to be coupled with components that prevent the harboring of bacteria at the implant-abutment junction.
It should be clear that the implant should be placed within healthy bone, which may have been reconstructed. In the case of immediate implants, the rough surface permits the direct attachment of bone to the implant within the extraction socket where the blood clot has been contained.
Abutment
The essential feature of the implant abutment connection is to be tight enough to prevent leakage. It should also be stable under functional load to avoid deformation and therefore leakage. The feature, which has been well tried in the engineering world and borne out by scientific investigation, is the tapered or conical connection. Therefore this non-indexed connection can be fabricated to a high degree of accuracy by a lathe and be produced to an accuracy that prevents microleakage.
It has been suggested that the attachment of the abutment at the time the per-mucosal entry is created may be of benefit. This means that the definitive abutment is attached at the time of implant placement in the case of an immediate implant. If a staged approach is used, then the abutment is attached at the time of implant exposure. The aim is to establish a hemidesmosomal connection between the abutment surface and the surrounding soft tissues (Figure 3).
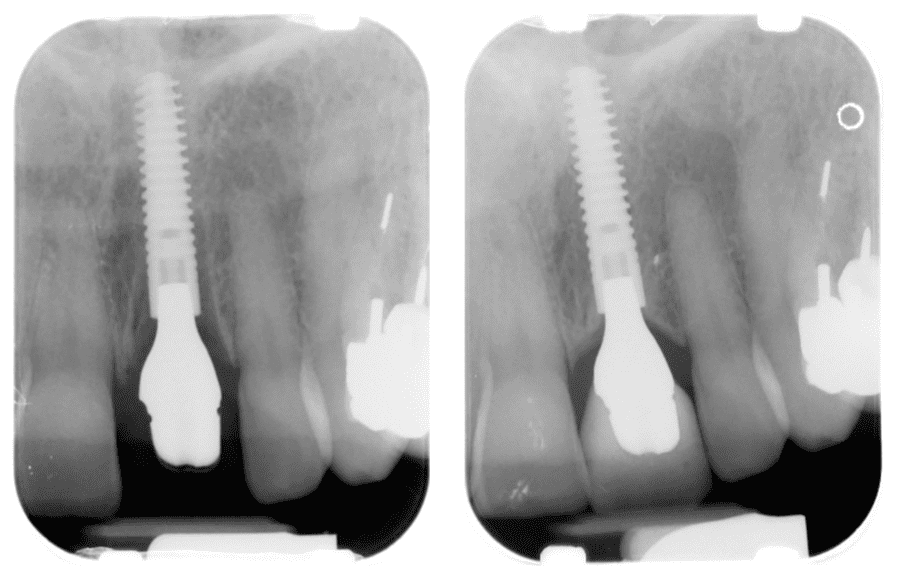
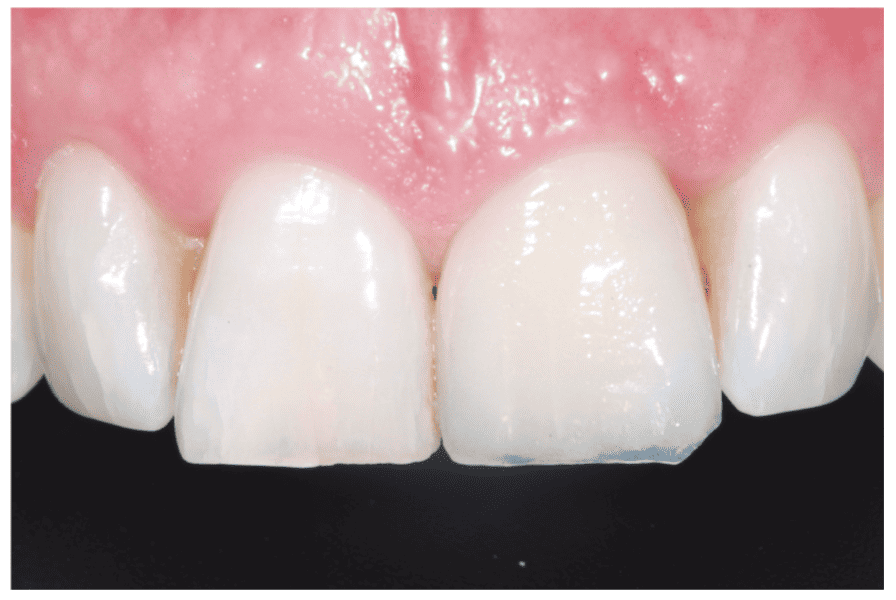
The protocol outlined above would therefore provide two levels of protection — the bone over the implant and the direct connection of the soft tissue to the abutment (Figure 4-6).
Type of restoration
The design of the restoration should be such that access for cleaning is provided. Overhangs and large, adversely contoured flanges should be avoided. The ideal material to penetrate the soft tissues must be biocompatible (either titanium or zirconium oxide). This is often compromised in the esthetic zone by having an intra-sulcular margin to establish the ideal esthetic emergence profile. Screw-retained restorations have the disadvantage of leakage as a result of the inherent space between the component parts. Cement retention eliminates this but adds the additional risk of excess cement being intruded below the gingival margin when an intra-sulcular margin is required for esthetic purposes. The introduction of conical retention, eliminating cement and screws, promises to offer a solution and will be verified as time goes on.
Conclusion
Implant treatment is often the choice for the replacement of missing or failing teeth. High success rates have been reported, and the recent observations of an increased rate of peri-implant disease must be addressed.
Proper understanding of the biology of healing is fundamental to safe practice of implant dentistry. Appropriate training in this field is essential. The protocols outlined are considered fundamental to achieving long-term stability.
The patient’s microbiology may be involved in the risk factors for peri-implantitis. Read this CE on the microbiology of peri-implantitis and discover some new protocols for its treatment.
References
- Cosyn J, Van Aelst L, Collaert B, Persson GR, De Bruyn H. The peri-implant sulcus compared with internal implant and suprastructure components: a microbiological analysis. Clin Implant Dent Relat Res. 2011;13(4):286-295.
- Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11(5):391-401.
- Doos N, Laurell L, Mardas N. Hierarchical decisions on teeth vs. implants in the periodontitis-susceptible patient: the modern dilemma. Periodontol 2000. 2012;59(1): 89-110.
- Gross M, Abramovich I, Weiss EI. Microleakage at the abutment-implant interface of osseointegrated implants: a comparative study. Int J Oral Maxillofac Implants. 1999;14(1):94-100.
- Heitz-Mayfield LJ, Needleman I, Salvi GE, Pjetursson BE. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int J Oral Maxillofac Implants. 2014;29(suppl):346-350.
- Mairgünther R, Nentwig GH. Das Dichtigkeitsverhalten des Verbindungssystems beim zweiphasigen NM-Implantat. [The tightness behavior of the connection system of the 2-phase Ankylos implant]. Z Zahnärztl Implantol. 1992;8:50-53.
- Monje A, Aranda L, Diaz KT, et al. Impact of Maintenance Therapy for the Prevention of Peri-implant Diseases: A Systematic Review and Meta-analysis. J Dent Res. 2016;95(4):372-379.
- Sethi A, Kaus T. An implant that does not smell – The Ankylos Implant. Irish Dentist. July 2002.



