Educational aims and objectives
This clinical article aims to describe the surgical processes and key principles of partial extraction therapy and present a case illustrating the application of this technique.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the protocols, supporting evidence, and indications of partial extraction therapy (PET).
- Realize some clinical approaches that attempt to address the unpredictability of the soft and hard tissue deficiencies that can interfere with optimal implant positioning and esthetics.
- Observe this approach that allows the preservation of the periodontal ligament and avoids the disruption of the periodontal dynamics, allowing an ideal soft, hard tissue volume preservation and vascularization.
- Realize the benefits for PET for specific clinical cases.
- Observe a case that used PET to treat a coronal fracture of a maxillary lateral incisor, followed by an implant.
Drs. Filipe Amante and Patrik Zachrisson show how the socket shield technique can allow for the preservation of the periodontal ligament, avoiding the disruption of periodontal dynamics. Read how this technique can be helpful for specific types of patients.
Drs. Filipe Amante and Patrik Zachrisson describe the use of partial extraction therapy in a case of coronal fracture of a maxillary lateral incisor
The usage of osseointegrated dental implants to replace missing or hopeless teeth is currently regarded as one of the best treatment options in dentistry worldwide. Since the technique was presented to the world by Brånemark several decades ago, implant dentistry has progressed immensely, fueled by an active and continuous research that has instigated the materials, methods, and techniques to evolve.
Years of experience and clinical data have proven that the peri-implant complex plays an essential role on the short- to long-term stability of implant restorations. Furthermore, the literature has shown that respecting and preserving this delicate and crucial area is essential to achieving long-term success and predictability in implant dentistry.
Following the extraction of a tooth, there is a reorganization of the periodontal area affecting soft and hard tissue volume and irrigation. Numerous publications have confirmed that, following tooth loss, there is a dimensional transformation that takes place on the alveolar ridge contour (Amler, et al., 1960; Schropp, et al., 2003; Araújo and Lindhe, 2005; Fickl, et al., 2008a), which is particularly noticeable in the anterior zone.
Furthermore, the resulting soft and hard tissue deficiencies can interfere with optimal implant positioning and affect the overall esthetic outcome and long-term prognosis of implant-supported prostheses (Hurzeler, et al., 2010).
The immediate placement of dental implants following dental extraction and several guided-bone regeneration (GBR) techniques have been described and used for many years, but despite all the advances in bone augmentation and periodontal surgery, there is still an element of unpredictability when the entire tooth element is removed.
Approaches such as soft and hard tissue augmentation procedures, immediate provisionalization, flapless implant placement, a more palatal placement of the implant, and the use of platform switching (Baumer, et al., 2015) have been used to attempt to address this unpredictability. Despite the positive effects of these techniques, it is widely accepted that an optimal esthetical result can be reached in only specific cases (Khzam, et al., 2015), as the tissue changes cannot be entirely prevented or compensated for (Esposito, et al., 2012; Chen and Buser, 2014; Lin, et al., 2014).
The marked alterations after tooth extraction appear to be attributable to the loss of the periodontal ligament and the consecutive trauma, particularly at the buccal bone plate (Araújo and Lindhe, 2005).
In the past decade, several clinicians and researchers have suggested that, in specific clinical circumstances upon immediately placing a dental implant, rather than extracting the entire hopeless tooth, it may be beneficial to leave a buccal fragment in situ through partial extraction therapy (PET) or the “root membrane technique.”
This approach allows the preservation of the periodontal ligament and therefore avoids the disruption of the periodontal dynamics, allowing an ideal soft, hard tissue volume preservation and vascularization.
Several in vivo and in vitro studies have shown encouraging results to support this approach. In 2010, Hürzeler, et al., described the socket shield technique (SST) with an article that involved the histological evaluation in a beagle dog. The protocol involved the partial extraction of the tooth, leaving a buccal fragment in situ (shield), followed by the immediate placement of a dental implant.
The results showed no resorption of the root fragment and also new cementum formed on the implant surface. Furthermore, there was noted excellent buccal soft and hard tissue preservation and clinically successful osseointegration of the implant. Bäumer, et al. (2015), conducted a pilot study that concentrated on the histological, clinical, and volumetrical observation of the alveolar ridge and implant after a similar protocol. The results were equally promising and concluded that the periodontal ligament of the tooth segment remained healthy; there were minor volumetric change of the ridge contour, and there was evident direct bone-to-implant contact.








Since then, an exponential number of clinical case reports have emerged, with promising results and with longer follow-ups that have observed the clinical appearance and stability of the peri-implant soft and hard tissues, as well as evaluating the volumetric changes of the affected buccal contours in the long term.
The results available so far seem to suggest that the PET may reduce the extent of treatment and decrease patient stress and pain (Hürzeler, et al., 2010).
Furthermore, the technique has additional advantages: There is no added cost for materials; comorbidity is reduced; it can be applied in the presence of apical pathology; and it requires reduced surgical intervention (Chen, 2013). Despite the encouraging results and the potential benefits highlighted by the literature, PET should only be considered suitable for specific clinical cases.
Baumer, et al. (2015), in a 5-year follow-up clinical study, defined the following exclusion criteria for the SST: teeth with present/past periodontal disease; teeth with vertical root fractures on the buccal aspect; teeth with horizontal fractures at/below gum level; teeth with other pathologies affecting the buccal part of the root, for example, external or internal resorptions, except apical pathology; heavy smokers; lack of neighbor teeth; bad oral hygiene; and lack of capacity to provide valid consent.
The aim of this article is to describe the use of the PET in a case of a coronal fracture of a maxillary lateral incisor. A dental implant was immediately placed and later on restored with a crown fabricated in-house using a digital workflow.
Clinical case
The patient, a 63-year-old male, was referred by his GDP for a consultation in view to replace his fractured upper left lateral incisor. The tooth was fractured at gum level after having had a root canal treatment and a crown for several years. The GDP had previous discussed different replacement options such as bridges and dentures, but the patient was adamant he would like to have the tooth replaced with a dental implant.
He was fit and healthy, did not take any medication, and had previously been a regular attender to the dental practice. He presented with a considerably restored dentition, good oral hygiene, no evidence of other active decay or periodontal disease, didn’t smoke, and reported consuming alcohol sporadically.
After discussing the different treatment options, the patient agreed to have a sequence of clinical records taken including a CBCT scan, upper and lower alginate impressions (for study models and a surgical guide), and a maxillary silicone putty/wash impression (for a temporary bonded Maryland bridge), as well as a sequence of intraoral and extraoral photographs.
The implant treatment planning protocol followed at the author’s practice involves the formulation of an extensive and thorough document that encompasses all of the information gathered during the preliminary stages of treatment and is sent to the patient in advance to allow an appropriate time for the information to be read, assimilated, and hopefully fully understood. The patient was presented with two clinical scenarios: a more traditional approach that included the complete removal of the condemned tooth followed by either an immediate or delayed implant placement (possibly involving bone and/or soft tissue augmentation procedures), or the partial removal of the tooth with the immediate placement of the implant without resorting to raising a flap as described by the SST.


Figures 10A and 10B: Intraoral view at 3-months postoperative with scan body in situ


After some deliberation, the patient decided to go ahead with the latter approach, as it was less invasive and more conservative. He confessed that he found the prospect of having a flapless surgical procedure and a better esthetic final outcome quite appealing, despite being aware that this technique wasn’t as documented as the more traditional alternative. The surgical appointment was subsequently booked, and on the day, the patient was given the opportunity of asking questions about the procedure and risks involved, and the consent form was signed.
No new complaints or medical changes were reported preoperatively, and the patient was given a prophylactic dose of anti-biotics — 3g of amoxicillin 1 hour before the procedure. (There were no reports of allergies or hypersensitivity to any medication.) The patient was then anesthetized having received two cartridges of Septanest (articaine) (Septodont) that were infiltrated buccal and palatally. A strict standardized sterilization protocol was then followed to prepare the patient and the surgical room, including the placement of sterile draping on all of the working surfaces, and the usage of sterile gowns and hats on clinical staff and patient.
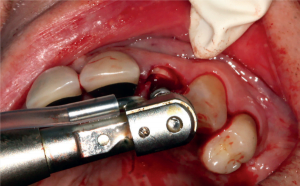
The patient was then disinfected extraorally and intraorally with a 0.20% chlorhexidine + PVP-VA and hyaluronic acid solution, and the surgical procedure started with the section of the retained root. This is a very delicate process that starts with the mesiodistal hemi-section of the root, effectively separating it in buccal and palatal fragments.
Some of the literature advises the usage of slow handpiece burs similar to the ones used in re-root canal treatment, prior to the root hemi-section, particularly in cases of single canal teeth (there are presently PET bur kits available specifically for this purpose). In this instance, it was opted to carefully remove the palatal fragment, but in certain cases the osteotomy can be performed directly through the palatal fragment and, once completed, the removal of the proximal/palatal fragments can take place.
It is of utmost importance to ensure that there is no pressure exerted on the buccal shield upon removing the unwanted portions of the tooth, as it is essential not to disturb the buccal periodontal area, which is critical for the success of the technique. The osteotomy was then performed with a periapical X-ray taken with a parallel pin to confirm the correct angulation and dismiss any other possible problems, and a 4.5 x 11.5mm Osstem TSIII implant was inserted with a torque of approximately 35Ncm.
The position of the implant in the socket followed the original pathway of the root parallel to the neighboring teeth and slightly more palatally to ensure that there was no direct contact with the socket shield. The gap between the implant and the socket shield will then be filled with a blood clot, and there is usually no need to use bone augmentation materials or membranes; in this particular case, a portion of collagen sponge (ParasorbA®, Resorba®) was used.
Some authors believe that using an enamel matrix protein (Emdogain®, Straumann®) can be applied in this gap and help initiate the process of new cementum formation, which could aid in the prevention of root resorption on the long term (Baumer, et al., 2017). A healing cap was placed along with one single suture 6-0 Prolene® (Ethicon) and, as planned, a bonded Maryland bridge was ready to be fitted on the day to adequately provisionalize the area.
The technicians were instructed to construct the bridge with an anatomy that would not exert unwanted pressure on the underlying soft tissue, and the patient was very happy with the result at that stage.
The patient was given comprehensive postoperative instructions, including rinses with 0.12% chlorhexidine mouthwash 3 times per day for the first week, and advised to take paracetamol and/or ibuprofen 3 times per day for the first 72 hours. The patient was reviewed after a week and reported no postoperative discomfort.
Clinically, the soft tissue and temporary bridge were looking fine, with no evidence of inflammation or other ill symptoms. Eleven weeks after this, the patient returned in order to assess the osseointegration of the implant and the appearance of the surrounding soft tissues.
A periapical X-ray view showed a favorable outcome with a satisfactory presence of bone around the implant and in between the threads, and also that the soft tissue volume remained stable and healthy looking. The patient reported no discomfort and had been quite happy with the temporary bonded bridge that was subsequently removed.


A Ti-Base was then fitted and a digital impression taken using the CEREC Omnicam (Dentsply Sirona). An IPS e.max® (Ivoclar Vivadent) crown was made in-house, stained, characterized accordingly, and fitted to the Ti-Base, and was fitted that same day.
A periapical view confirmed the engagement of the implant fixtures, and the crown was torqued to 25Ncm as per the manufacturer’s advice, and the palatal access covered with flowable composite following the placement of some Teflon tape to protect the screw access.
The occlusion was checked and no adjustments were necessary. The patient was then instructed in regard to the oral hygiene (regular visits to the hygienist were recommended) and was advised to return for a review appointment. After 12 months, the patient was again reviewed and reported no problems. Furthermore, the volume of soft tissue seemed to have been maintained, and there were no evidence of pain, inflammation, mobility, or other ill symptoms.
Conclusion
The privilege of being a dentist and to be able to make a difference in people’s lives comes with a great burden and a constant responsibility to keep our skills updated to ensure we provide the best possible care to our patients. The ongoing clinical and scientific research in dentistry is continuously providing us with new and improved treatment options to help our patients in the best possible way, and it is our mission as modern dentists to keep updated with the innovations in our field.
The PET has now been documented for more than a decade. The results obtained are incredibly promising and have been increasingly supported by clinical data that is constantly emerging. However, it is of utmost importance that each clinical case is individually assessed, namely in regard to the case selection and — very importantly – the experience and clinical confidence of the dental surgeon performing the procedure.
The concepts of preservation, diminished comorbidity and ideal esthetic outcomes that are defended by the PET are very attractive, but if the case selection and technical completion of the technique are not adequate, this can be a recipe for disaster.
For this particular clinical case, the PET proved to be extremely helpful, and the results achieved were quite rewarding for both patient and clinicians. The authors agree that further clinical data needs to emerge for this technique to be regarded as a more mainstream approach but, nonetheless, the current state of the art suggests that this technique may become increasingly used in the future of implant dentistry.
Besides the socket shield technique, Dr. Zacchrisson and co-author Dr. Eddie Scher wrote about “mixed bite” patients. Read their CE (subscribers can take the quiz and earn 2 CE credits). https://implantpracticeus.com/ce-articles/intrusion-natural-teeth-connecting-teeth-implants/
References
- Al Dary H, Al Hadidi A. The socket shield technique using bone trephine: a case report. Int J Dent Oral Sci. 2015;5(001):1-5.
- Amante LF, Mamede DM. The socket shield technique: a conservative approach in Implant Dentistry. Implant Dentistry Today. 2018;12(3):33-38.
- Abadzhiev MN, P Velcheva P. Conventional immediate implant placement and immediate placement with socket-shield technique – which is better. Int J Clin Med Res. 2014;1(5):176-180.
- Araujo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32(2):212-218.
- Baumer D, Zuhr O, Rebele S, Schneider D, Schupbach P, Hurzeler M. The socket-shield technique: first histological, clinical, and volumetrical observations after separation of the buccal tooth segment – a pilot study. Clin Implant Dent Relat Res. 2015;17(1):71-82.
- Buser D, Warrer K, Karring T. 1990; Formation of a periodontal ligament around titanium implants. J Periodontol. 2015;61(9):597-601.
- Chen C, Pan Y. Socket shield technique for ridge preservation: a case report. J Prosthodont Implantol. 2013;2(2):16-21.
- Cherel F, Etienne D. Papilla preservation between two implants: a modified socket-shield technique to maintain the scalloped anatomy? A case report. Quintessence Int. 2014;45(1):23-30.
- Fickl S, Zuhr O, Wachtel H, Stappert CF, Stein JM, Hurzeler MB. Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J Clin Periodontol. 2008a;35(10):906-913.
- Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler M. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J Clin Periodontol. 2008b;35(4):356-363.
- Filippi A, Pohl Y, von Arx T. Decoronation of an ankylosed tooth for preservation of alveolar bone prior to implant placement. Dent Traumatol. 2001;17(2):93-95.
- Glocker M, Attin T, Schmidlin PR. Ridge preservation with modified ‘socket-shield’ technique: a methodological case series. Dent J. 2014;2(1):11-21.
- Gluckman H, Du Toit J, Salama M. The socket-shield technique to support the buccofacial tissues at immediate implant placement. Int Dent Afr Ed. 2015;5(3):6-14.
- Gluckman H, Salama M, Toit JD. Partial extraction therapies (PET) part 1: maintaining alveolar ridge contour at pontic and immediate implant sites. Int J Periodontics Restorative Dent. 2016;36(5):681-687.
- Gluckman H, Salama M, Toit JD. Partial extraction therapies (PET) part 2: procedures and technical aspects. Int J Periodontics Restorative Dent. 2017;37(3):377-385.
- Gray JL, Vernino AR. The interface between retained roots and dental implants: a histologic study in baboons. J Periodontol. 2004;75(8):1102-1106.
- Groenendijk E, Staas TA, Graauwmans FE, et al. Immediate implant placement: the fate of the buccal crest. A retrospective cone beam computed tomography study. Int J Oral Maxillofac Surg. 2017;46(12):1600-1606.
- Holbrook SE. Model-Guided flapless immediate implant placement and provisionalization in the esthetic zone utilizing a nanostructured titanium implant: a case report. J Oral Implantol. 2016;42(1):98-103.
- Guarnieri R, Giardino L, Crespi R, Romagnoli R. Cementum formation around a titanium implant: a case report. Int J Oral Maxillofac Implants. 2002;17(5):729-732.
- Helsham RW. Some observations on the subject of roots of teeth retained in the jaws as a result of incomplete exodontia. Aust Dent J. 1960;5(2):70-77.
- Herd JR. The retained tooth root. Aust Dent J. 1973;18(3): 125-131.
- Hurzeler MB, Zuhr O, Schupbach P, et al. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855-862.
- Jahangiri L, Hessamfar R, Ricci JL. Partial generation of periodontal ligament on endosseous dental implants in dogs. Clin Oral Implants Res. 2005;16(4):96-401.
- Kan JY, Rungcharassaeng K. Proximal socket shield for interimplant papilla preservation in the esthetic zone. Int J Periodontics Restorative Dent. 2013;33(1):e24-31.
- Lagas LJ, Pepplinkhuizen. JJFAA, Bergé SJ, Meijer GJ. Implant placement in the aesthetic zone: the socket-shield-technique. Ned Tijdschr Tandheelkd. 2015;122(1):33-36.
- Langer L, Langer B, Salem D. Unintentional root fragment retention in proximity to dental implants: a series of six human case reports. Int J Periodontics Restorative Dent. 2015;35(3):305-313.
- Malmgren B. Decoronation: how, why, and when? J Calif Dent Assoc. 2000;28(11):846-854.
- Mitsias ME, Siormpas KD, Kotsakis GA, et al. The root membrane technique: human histologic evidence after five years of function. Biomed Res Int. 2017; doi: 10. 1155/2017/7269467
- Mitsias ME, Siormpas KD, Kontsiotou-Siormpa E, et al. A step-by-step description of PDL-mediated ridge preservation for immediate implant rehabilitation in the esthetic region. Int J Periodontics. Restorative Dent. 2015;35(6):835-841.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. 2009;339:b2535
- Nayyar J, Clarke M, O’Sullivan M, Stassen LF. Fractured root tips during dental extractions and retained root fragments. A clinical dilemma? Br Dent J. 2015;218(5):285-290.
- Ong CT, Ivanovski S, Needleman IG, et al. Systematic review of implant outcomes in treated periodontitis subjects. J Clin Periodontol. 2008;35(5):438-462.
- Parlar A, Bosshardt DD, Unsal B, et al. New formation of periodontal tissues around titanium implants in a novel dentin chamber model. Clin Oral Implants Res. 2005;16(3):259-267.
- Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967;17(1):21-27.
- Saeidi Pour R, Zuhr O, Hürzeler M, et al. Clinical benefits of the immediate implant socket shield technique. J Esthet Restor Dent. 2017;29(2):93-101.
- Salama M, Ishikawa T, Salama H, Funato A, Garber D. Advantages of the root submergence technique for pontic site development in esthetic implant therapy. Int J Periodontics Restorative Dent. 2007;27(6):521-527.
- Sapir S, Shapira J. Decoronation for the management of an ankylosed young permanent tooth. Dent Traumatol. 2008;24(1):131-135.
- Siormpas KD, Mitsias ME, Kontsiotou-Siormpa E, Garber D, Kotsakis GA. 2014; Immediate implant placement in the esthetic zone utilizing the ‘root-membrane’ technique: clinical results up to 5 years postloading. Int J Oral Maxillofac Implants. 2008;29(6):1397-1405.
- Schropp L, Wenzel A, Stavropoulos A. Early, delayed, or late single implant placement: 10-year results from a randomized controlled clinical trial. Clin Oral implants Res. 2013;25(12):1359-1365.
- Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23(4):313-323
- Tonetti MS. Risk factors for osseodisintegration. Periodontol 2000. 1998;17:55-62
- Tonetti MS. (1999) Determination of the success and failure of root-form osseointegrated dental implants. Adv Dent Res. 13:173-180
- Troiano M, Benincasa M, Sánchez P, Calvo-Guirado J. Bundle bone preservation with Root-T-Belt: case study. Ann Oral Maxillofac Surg. 2014;2(1):7
- Wadhwani P, Goyal S, Tiwari S, et al. Socket Shield Technique: A new concept of ridge preservation. Asian J Oral Health Allied Sci. 2013;2015;5(2):55-58.

 Filipe Amante, LMD, MSc, is in private practice in London and Cambridgeshire. He has completed extensive postgraduate training in implant dentistry, oral surgery, and digital and cosmetic dentistry in Brazil, Portugal, UK, and Italy. Dr. Amante has been shortlisted for numerous professional awards, including Best Young Dentist (2017, 2018, and 2019) and Digital Rookie (2018, 2019).
Filipe Amante, LMD, MSc, is in private practice in London and Cambridgeshire. He has completed extensive postgraduate training in implant dentistry, oral surgery, and digital and cosmetic dentistry in Brazil, Portugal, UK, and Italy. Dr. Amante has been shortlisted for numerous professional awards, including Best Young Dentist (2017, 2018, and 2019) and Digital Rookie (2018, 2019). Patrik Zachrisson, LEG,TDL KI Swe, is the owner of Wensleydale Dental Practice and Wensleydale Dental Laboratory. He is vice president of the International Digital Dentistry Academy (IDDA) and visiting assistant professor at College of Medicine and Dentistry, Birmingham.
Patrik Zachrisson, LEG,TDL KI Swe, is the owner of Wensleydale Dental Practice and Wensleydale Dental Laboratory. He is vice president of the International Digital Dentistry Academy (IDDA) and visiting assistant professor at College of Medicine and Dentistry, Birmingham.

