Educational aims and objectives
This article aims to discuss various types of implant failures and ways to manage them.Expected outcomes
Implant Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Click here for the online quiz for subscribers. Correctly answering the questions will demonstrate the reader can:
• Recognize complications related to implant placement.
• Identify complications related to implant position.
• Realize some complications that could occur during the integration phase.
• Identify some complications that can occur once the implant has been restored.
• Realize some causes and treatment for peri-implantitis.
It is important to appreciate the fact that dental implant surgery is SURGERY. It is invasive and can have irreversible effects on patients. Before dentists begin incorporating implant surgery in to their practice, they must understand the difference between a technician and a doctor. The technician understands, usually quite well, “how” to do a procedure. But in order to be successful as an implant surgeon, it is necessary to be a doctor. There is nothing that we can do in surgery that is without complications. So, in order to properly manage and hopefully avoid most complications, a doctor must also understand the “why,” the “why not,” and the “what if” of the procedure he/she is performing.
One of the most important things we do as part of the treatment planning process is to educate our patients about the benefits and potential risks of surgery. Patients and clinicians both want to think of dental implants as being permanent replacements for missing teeth. I like to tell my patients that “dental implants are as permanent as your permanent teeth.” That is, with good care and a bit of luck, the implants can last them a very long time. But just as their permanent teeth can be lost prematurely, so can dental implants, and no matter how good our technology and surgical skills, we cannot do better than nature. That goes a long way to help them understand the situation when implants do fail. There are a number of reasons that dental implants can fail. These can be due to patient factors, such as diabetes, smoking, medications that impair wound healing, and bone repair,1 as well as parafunctional habits that can put excess biomechanical stress on a dental implant.2 Sometimes implants are doomed to fail because the clinician failed to completely examine the patient and was not aware of an anatomical factor that put the fixture in a compromised position. Other times, it is inadequate surgical technique or peri-operative care that is responsible for implant failure. But sometimes, no matter how well-planned, executed, and cared-for implant treatment may be, good old bad luck may be the culprit. A comprehensive discussion of implant failures and their management would fill an entire textbook and still be incomplete. Due to space limitations, I will only discuss some of the common ones. Implant failure can occur at any point in time, but for discussion, let’s categorize complications into those that occur at the time of placement, those during the integration phase, and those once the implant has been restored.
Complications related to implant placement
Implant position complications
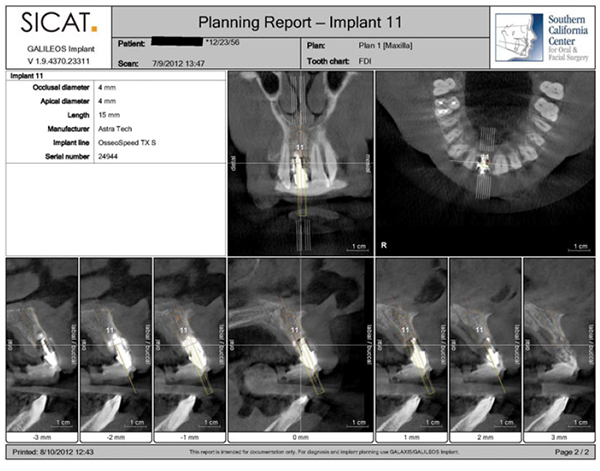
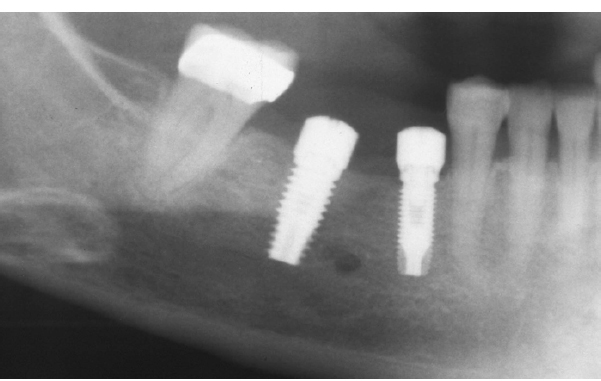
The primary causes of implant failure can be attributed to poor planning and placement. A natural tooth, which is attached to the alveolar bone through a vascularized periodontal ligament space, may be only partially supported within bone. In contrast, it is imperative that there be an adequate volume of healthy bone surrounding a dental implant. Most of the data suggest that there should be at least a thickness of 1.8 mm–2.0 mm of healthy bone on the buccal (facial) and lingual (palatal) aspects of each implant fixture, as well as 1.5 mm or more between an implant and a natural tooth,3 and 3.0 mm between adjacent implants.4 One should keep in mind that these values are minimums. Violation of this minimal bone thickness leads to compromised vascular supply to the surrounding bone at the crest, lower loading handling during function, and ultimately bony resorption, resulting in implant failure, as well as potential loss of neighboring teeth. This is a situation that should be a thing of the past. When I trained in oral and maxillofacial surgery, we used only a panoramic radiograph, study models, and clinical examination to treatment plan implant surgery cases. It was impossible to accurately appreciate the three-dimensional anatomy of the patient’s jaws to determine ridge form and volume. Surgical guides, if they were even used, were only reference appliances for the initial and subsequent osteotomies. Even if the first drill was placed through a sleeve in the guide, there was no depth control, and subsequent drills were all used freehand, so the implant trajectory could deviate during site preparation. As the radiographs being used only provided a 2D image, a clinician could not easily assess the shape of the ridge in the buccal-lingual dimension unless a full flap was placed. This could lead to implant placement outside the confines of the ridge which may not be apparent until failure initiated (Figures 1 and 2). In addition, most implant sites were accessed through surgical flaps. It was not unusual for the implant position, size, and/or angulation to require modification once the ridge was directly visualized.


This type of placement error should now be a thing of the past, as 3D CBCT imaging and treatment planning software are readily available in an increasing number of dental practices, and more implant systems are developing fully guided (CBCT-based) implant surgery kits (Figure 3). These advancements in implantology allow the clinician to fully evaluate the bony and soft tissue architecture based on a prosthetically driven treatment plan helping eliminate any surprises at the surgical phase. This allows the implant positions to be planned on a 3D image of the jaws such that they are within an adequate volume of bone, correctly spaced and in line with the proposed prosthesis (Figure 4). The surgical guide produced from this data, along with the corresponding surgical kit, allows the implant fixtures to be placed as planned, with a minimal margin of error, which is below the threshold of what the human eye can discern. If, during planning, there is determined to be a deficiency in bone volume, that issue can be addressed in a pre-implant surgical procedure or at the time of implant placement, whichever is most appropriate. With today’s technology and surgical techniques, implant placement errors should be a rare occurrence.
Sinus violation
Another potential source of implant failure is the violation of the floor of the maxillary sinus and Schneiderian membrane at the time of surgery. For the most part, minor perforations should have little or any adverse consequences.5 The body has a remarkable capacity for recovery, and minor tears in the membrane will heal uneventfully the majority of the time. When an oral and maxillofacial surgeon performs a Le Fort osteotomy procedure for a congenital jaw deformity, the sinus walls are completely severed, and the sinus membrane is circumferentially divided. Titanium plates and screws are used to stabilize the maxilla in its new position. No attempt is made to repair the sinus membrane, and the circumvestibular incision is closed in two layers. Even with this massive violation, sinus infections and screw failures are extremely rare (Figure 5). So, the fear of a small sinus floor perforation and tear in the lining membrane resulting in implant failure is significantly overrated.

What usually leads to posterior maxillary implant failure is an inadequate thickness of bone to provide primary mechanical stabilization to the implant fixture. With the lower density and thus quality of bone in the posterior maxilla, a minimum of 5 mm of solid bone is required to give a high likelihood of success. When this minimum requirement is violated, implant mobility leading to infection and failure is inevitable.6 Again, 3D CBCT treatment planning combined with an adequate amount of education will prevent most occurrences of this complication.
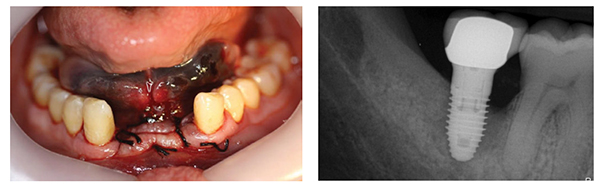
Soft tissue problems
Another factor that frequently leads to implant failure is an inadequacy of keratinized tissue around the fixture, potentiating the possibility of peri-implantitis, which then leads to bone loss and implant mobility. A very common statement I hear from inexperienced implantologists is the belief that having a CBCT, digital plan, and a surgical guide based on this plan, gives them the ability to place implants through a tissue-punch incision. This demonstrates a lack of understanding of implant surgical principles. The ability of performing “flapless” implant surgery is based on having an adequate bone and keratinized tissue volume. If either is deficient and requires modification, than an open surgical approach with a flap is required. A natural tooth has a defined biologic width, which is the sum of the thickness of the connective tissue, junctional epithelium, and sulcus depth. This usually measures 2.0 mm–3.0 mm around a healthy tooth.7 For a dental implant, a minimum of 2.0 mm of attached gingival tissue around the emergence of the fixture is necessary to avoid violation of the biologic width and development of peri-implant soft tissue inflammation. If less than this is available, the tissue should be modified to develop additional keratinized tissue.7
Nerve injury
Another complication related to treatment planning is injury to the inferior alveolar or lingual nerves. Lingual nerve injury can generally be avoided by keeping incisions away from the lingual aspect of the posterior mandibular ridge, and by ensuring that reflection of any lingual tissue is kept in the plane between the periosteum and alveolar bone. A full thickness flap in this area elevates the lingual nerve with the tissue lessening an incidence of damage to this nerve, which may occur if a partial thickness flap was utilized. Injury to the inferior alveolar nerve is caused by violation of the inferior alveolar canal by implant osteotomy drills or fixtures. This is something that is easier to prevent with proper treatment planning and careful surgical technique. The mandibular (inferior alveolar) nerve passes through the mandible from the lingula to the mental foramen, transversing the body of the mandible, then exiting via the mental foramen into the lower lip. The position of the mandibular canal is extremely variable. Periapical radiographs are completely inadequate for determining the distance between the mandibular canal and the alveolar crest due to elongation or foreshortening artifact. At the minimum, a panoramic radiograph is required, taking into account a 20%-25% magnification factor in images taken on a panoramic unit. This magnification varies unit brand to unit brand and is not constant over the width of the panoramic image. The implant surgeon must keep in mind that for most systems, the tip of the osteotomy drills extends up to 0.5 mm beyond the apical end of the implant fixture. A margin of safety of 2.0 mm should be factored in when planning the length of the fixture to be placed.8

If this distance is violated, by either an osteotomy drill or an implant fixture, injury to the inferior alveolar nerve may occur (Figure 6). We categorize the injury by the Seddon Classification, which stratifies severity of injury and prognosis for recovery (Figure 7). The least severe injury is generally due to blunt trauma or stretching of the nerve, is referred to as “neuropraxia.” In this category, there is no physical disruption of nerve fibers. There may be contusion and the resulting hematoma beneath the epineurium, the sheath, which surrounds the bundle of nerve fibers; but there is no loss of continuity of the nerve. Patients will describe a sensation of “tingling” in their lip or tongue, have reduced sensation, but no areas of total lack of sensation or pain. This group has the best prognosis for a full recovery. Next is “axonotmesis” in which there is damage to the nerve fibers, but the perineurium, which surrounds nerve bundles, is intact. This may result due to the implant “crushing” the nerve, and the resulting pressure leads to the deficit. The deficit will be more profound, and recovery will be slower and possibly incomplete. The key to treatment of this type injury when the implant is impinging on the nerve is early identification and either removal of the implant or backing it out of the osteotomy to relieve the pressure on the nerve before implant integration can occur and atrophy of the nerve results. The most severe injury is classified as a “neurotmesis.” Here, there is severance and disruption of individual nerve fibers. It may be partial or complete. These patients will have areas of total anesthesia and may have painful “dysesthesia” (abnormal altered sensation), and have the worst prognosis.

When a patient reports symptoms of a nerve injury after surgery, the first step is explanation to the patient of what occurred, followed by careful examination and documentation of the deficit, followed by a discussion of the severity of the injury, what to expect, and what to do about it. In the case of mandibular nerve injury, immediate imaging with CBCT or medical CT scanning is recommended to determine the extent of violation of the inferior alveolar canal. If imaging shows that the implant fixture is in close proximity or within the mandibular canal, prudent management dictates removal of the implant. The use of corticosteroids may have some benefit to reduce the duration of deficit for neuropraxia or mild axonotmesis cases. Return of sensation may be in days or could take 6 months or more, depending on severity. Gabapentin may help patients with painful sensations. In cases of neurotmesis, especially when there is total anesthesia or dysesthesia, surgical intervention may be indicated if improvement is minimal after 3 months. Referral to a neurologist is appropriate and, when indicated, should be done as early as possible to limit further damage to the nerve.

This complication is a good one to avoid, as it is a common cause of litigation against dentists. With the technology available to the implant surgeon today, it should be extremely rare. Three-dimensional imaging with CBCT allows for very accurate analysis of the position of the inferior alveolar canal at the sites of implant placement. Computerized treatment planning can be used to select the ideal fixture size, width, and position to avoid the mandibular nerve and maximize implant success (Figure 8). Combined with a surgical guide derived from this plan, CBCT-guided surgical techniques control the position, angulation and depth of each osteotomy and fixture placed (Figures 9-10). Following this protocol, inferior alveolar nerve injury can be completely avoided. The only other etiology for injury to either the mandibular, long buccal, or lingual nerve remains that from injection of local anesthetic. For many simple implant cases, a block injection can be avoided by simple infiltration of local anesthetic directly over the surgical site. Since the only innervation to an edentulous region is via the periosteum, good local anesthesia can be obtained for implant placement by infiltration alone.9

Bleeding
Bleeding during implant surgery can come from either inside the bone or from the soft tissues outside the bone. As long as the inferior alveolar vessels are avoided, most intraosseous bleeding encountered during implant site preparation can be stopped by simply placing the implant in the osteotomy. Bleeding from the soft tissue can be much more problematic. The most problematic area is from the sublingual and submandibular regions due to penetration of an osteotomy drill through the lingual cortex of the mandible (lingual perforation). Depending on the degree and location of injury, bleeding can be minor and cause a small hematoma to develop in the floor of the mouth (Figure 11) or result in severe hemorrhage, which can cause life-threatening obstruction of the airway.10 Firm direct pressure over the area of bleeding should be the first response.11 Surgical exposure for the purpose of cauterization or ligation of vessels should be performed by only those experienced in this procedure. The status of the airway should be carefully monitored, and intubation or tracheostomy should be considered if any airway compromise is observed. Those patients who have this issue arise should not be dismissed until the surgeon is confident that the bleeding has stopped or should be transported to the ER for further treatment so that the airway is not compromised. Again, this complication is best avoided by obtaining a 3D CBCT scan prior to surgery in order to identify any anatomic factors, such as concavity below the mylohyoid ridge, which may increase the risk of this complication. Accurate implant placement, utilizing a guided implant protocol will minimize or eliminate this possible risk.
Overheating injury
Overproduction of heat during osteotomy preparation results in necrosis of bone, leading to implant failure. Measures to prevent this include using copious irrigation with isotonic saline to cool and lubricate the drills, using light pressure on drills, utilizing short intermittent strokes to remove drilling debris and facilitate irrigant getting into the osteotomy sites, and reducing drill speeds as the drill diameter increases.12
Complications during the integration phase
Peri-implant soft tissue inflammation
Despite meticulous treatment planning and surgical technique, an implant may present with inflammation, swelling, and pain in the surrounding tissues.13 A periapical radiograph should be taken to rule out severe bone loss or the development of a radiolucent margin between the implant and bone. Both of these findings suggest implant failure, and the fixture should be considered for removal (Figure 12). If the implant is otherwise stable, and there are no radiographic changes, conservative management should include light debridement by the clinician with implant curettes, along with irrigation with chlorhexidine rinse.14 The patient should be placed on a broad-spectrum antibiotic, such as amoxicillin, cephalexin, or clindamycin. For home care, gentle irrigation with a pulsed-water flosser once daily is helpful. Adding a few drops of sodium hypochlorite to the water reservoir will serve as a very effective bacteriocidal agent to sterilize the sulcus around the implant. The patient should be monitored carefully until the situation resolves. This inflammation could be an early sign of implant failure. Occlusion on the implants’ prosthetics should also be evaluated and adjusted as needed to rule out an occlusion component.
Sinusitis
In general, a minor penetration of an implant fixture into the maxillary sinus, even with a small violation of the sinus membrane, does not lead to any untoward sequelae. However, occasionally, patients will report sinus pressure, pain, or drainage in the weeks, or sometimes months, following maxillary implant placement.5 Initial management should be conservative, consisting of antibiotics and sinus irrigation with saline. Augmentin or ciprofloxacin are good empiric choices. Treatment should be for 10–14 days. There are also a number of over-the-counter medications that will reduce swelling in the sinus and improve resolution. These include non-sedating antihistamines such as loratadine or fexofenadine, along with intranasal corticosteroids such as fluticasone or tri-amcinolone sprays. If the patient fails to improve, a Caldwell-Luc osteotomy to drain the sinus may be necessary. If the above treatments are not successful, consideration should be given to removal of the implant, with anticipation that an oral-antral communication will exist and will require surgical closure.
Implant mobility
If implant mobility is detected during the integration stage, the likelihood of the implant integrating is low, and further bone loss will occur if conservative management and observation are employed. The implant should be removed as soon as this is observed, the site thoroughly debrided of the inflammatory and fibrous tissue that formed between the implant and bone, followed by copious irrigation and bone grafting of the defect in anticipation of new implant placement 3 to 6 months in the future following complete site healing and fill of the osteotomy by the osseous graft placed.
Tooth movement
This complication during the integration phase is rarely mentioned because it does not lead to implant fixture failure. But it can lead to restorative failure in some cases. Mesial tooth migration is a known phenomenon. We have all seen mesial tipping of third molars into the second molar space after it has been extracted. Any tooth has the potential to tilt mesially into an edentulous space over time (Figure 13). Teeth may also hypererupt toward the other arch when the opposing tooth is missing. The rate at which this occurs is extremely variable. Patients can be missing a tooth for years, and no movement of the opposing or distal teeth will occur. Or, it can happen in a matter of months. If a dental implant was placed into the edentulous ridge, movement of surrounding teeth can dramatically affect the restorability of the implant. Since it is difficult to predict which patients will exhibit rapid tooth movement, I always recommend some type of space-maintaining appliance be worn until a provisional or final restoration can be placed. My preference is an Essix bridge, which is inexpensive to make and does not rest on the extraction site or implant head. Generally, 8 hours per day of wear is sufficient to prevent this complication.
Complications once the implant has been restored
Peri-implantitis
Most post-restoration implant complications are related to inflammation and resulting bone loss. The signs and symptoms include tenderness, pain, inflammation, purulent drainage, and bone loss.13 Once the integration period has passed, debridement around the implant fixture can be more aggressive versus during the first few months. All surrounding granulation tissue should be debrided using implant-safe curettes, and then copiously irrigated with sterile saline.14 As mentioned with peri-implantitis during the integration phase, a broad-spectrum antibiotic is recommended, as well as intrasulcular irrigation with a pulsed-water flosser once daily. A few drops of sodium hypochlorite added to the reservoir tank helps maintain a relatively healthy sulcus. There may be some gingival recession as the inflammation subsides.
If there is bone loss around the implant, but it is still stable, bone regenerative techniques may be used in addition to the preceding protocol to attempt to improve bone levels and reduce pocket depth. The prosthesis should be removed, and a cover screw placed to facilitate access and allow for coverage with a membrane. In addition, the defect should be treated with citric acid or tetracycline solution, and followed by sterile saline rinses before bone grafting material and a membrane are added. If despite attempts to salvage the implant, bone loss continues and mobility develops, the implant fixture should be removed, the site thoroughly debrided, and bone regeneration techniques employed. Early intervention when these issues are initially identified increases the prognosis of treating an ailing implant, whereas watching and waiting tends to lead to implant loss as the bone loss progresses to the point where salvaging the implant is not possible.
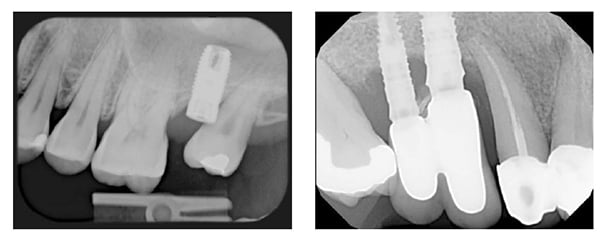
Cement sepsis
Fixed implant-supported prostheses can be either screw-retained or cement-retained. A properly made crown should be closely adapted to the implant abutment, with space for only a thin layer of cement. If an excess amount of cement is used, this will extravasate through the interface between the crown and abutment when the crown is seated extruding into the sulcus. Cement in the sulcus around a dental implant sets up an inflammatory response, and significant bone loss can result (Figure 14), even leading to failure of the fixture when intervention is not initiated soon enough.15 This situation is best avoided by using a very thin layer of a zinc oxide-based temporary cement for implant crowns. A bitewing radiograph may show cement if it is located in the interproximal areas, but it will not be radiographically visible on the lingual or buccal sulci. The margins should be carefully cleaned and checked for excess cement. Ideally, in the posterior non-esthetic regions, cemented margins should be kept supragingival. In the anterior esthetic zone, they should be no more than 1 mm subgingival. Cement sepsis should always be considered when a patient presents with peri-implantitis, especially in the first 6 months after crown cementation. It should be treated using the same technique as for peri-implantitis.
Closing thoughts
Once a dental implant issue is recognized, it should be managed immediately. Implant problems will not get better on their own. One of the basic principles taught in surgical residency is that a clinician should be comfortable managing the most common complications associated with any particular procedure before that clinician ever attempts that procedure. The same principle applies to all dentists who begin placing dental implants in their practice. As I mentioned in the first paragraph of this article, dental implant surgery is invasive and can cause irreversible injury to patients. Clinicians should be sure to educate themselves on both the science and technical aspects of implant surgery before performing their first procedure and then build upon that experience before attempting more advanced cases.
References
- Klokkevold PR, Han TJ. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants. 2007;22 (suppl):173–202.
- Koldsland OC, Scheie AA, Aass AM. Prevalence of implant loss and the influence of associated factors. J Periodontol. 2009;80(7):1069–1075.
- Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
- Jung JH, Choi BH, Zhu SJ, Lee SH, Huh JY, You TM, Lee HJ, Li J. The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(5):602-605.
- Peleg M, Garg AK, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: A 9-year longitudinal experience study of 2,132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006;21(1):94-102.
- Wennström JL, Derks J. Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res. 2012; 23(Suppl 6):136–146.
- Worthington P. Injury to the inferior alveolar nerve during implant placement: A formula for protection of the patient and clinician. Int J Oral Maxillofac Implants. 2004;19(5):731-734.
- Heller AA, Shankland WE 2nd. Alternative to the inferior alveolar nerve block anesthesia when placing mandibular dental implants posterior to the mental foramen. J Oral Implantol. 2001;27(3):127-133.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90(2):121-132.
- Park SH, Wang HL. Implant reversible complications: Classification and treatments. Implant Dent. 2005;14(3):211-220.
- Eriksson RA, Albrektsson T. Temperature threshold levels for heat-induced bone tissue injury: A vital-microscopic study in the rabbit. J Prosthet Dent. 1983;50(1):101-107.
- Khammissa RA, Feller L, Meyerov R, Lemmer J. Peri-implant mucositis and peri-implantitis: clinical and histopathological characteristics and treatment. SADJ. 2012;67(3):122,124–126.
- Persson GR, Samuelsson E, Lindahl C, Renvert S. Mechanical non-surgical treatment of peri-implantitis: a single-blinded randomized longitudinal clinical study. II. Microbiological results. J Clin Periodontol. 2010;37(6):563–573.
- Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998;17:63–76.
- Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol 2009;80(9):1388–1392.

 Jay B. Reznick, DMD, MD, is a Diplomate of the American Board of Oral and Maxillofacial Surgery. He received his dental degree from Tufts University, his MD degree from the University of Southern California (USC) and trained in Oral and Maxillofacial Surgery at LAC+USC Medical Center. His special clinical interests are in the areas of facial trauma, jaw and oral pathology, dental implantology, sleep disorders medicine, laser surgery, and jaw deformities. He also has extensive expertise in the integration of digital photography, 3D imaging, and CT-guided implant surgery in clinical practice.
Jay B. Reznick, DMD, MD, is a Diplomate of the American Board of Oral and Maxillofacial Surgery. He received his dental degree from Tufts University, his MD degree from the University of Southern California (USC) and trained in Oral and Maxillofacial Surgery at LAC+USC Medical Center. His special clinical interests are in the areas of facial trauma, jaw and oral pathology, dental implantology, sleep disorders medicine, laser surgery, and jaw deformities. He also has extensive expertise in the integration of digital photography, 3D imaging, and CT-guided implant surgery in clinical practice.

