Amit Binderman explains how advances in bone grafting by KometaBio have resulted in converting patient teeth into autologous dentin grafts.
Amit Binderman discusses converting extracted teeth into osseoinductive bone graft material
Alveolar bone regeneration is a crucial element of dental and maxillofacial surgery, particularly for patients requiring dental implants or corrective procedures due to traumatic injuries, periodontal defects, bone loss, or congenital anomalies. Traditional bone grafting methods have been employed to promote bone regrowth, but they often come with numerous limitations — including inflammation at the graft site (foreign material reaction), which hampers healing and impedes regeneration. Many traditional graft materials do not resorb, preventing the conversion of the site into native bone. On the other hand, some materials resorb too rapidly, failing to offer sufficient support for the longevity of newly formed tissue (woven bone). In certain instances, grafting material is susceptible to infection and soft tissue invagination into the graft itself. Furthermore, most materials do not integrate effectively with surrounding bone or dental implants, making them unpredictable when immediate placement is required. Although these limitations may not be critical in some cases such as sinus grafting, they significantly affect alveolar bone regeneration procedures, at times yielding unpredictable outcomes. Moreover, these materials are heavily reliant on the overall health condition of the patient — compromised patients like diabetics, smokers, and those on medication do not respond well to many materials, hindering successful bone regeneration.
Practitioners who rely on autologous bone, considered as the gold standard, resort to bone harvesting. However, these techniques often necessitate a secondary harvesting site, resulting in potential patient discomfort, morbidity, and increased costs. Furthermore, harvested bone frequently fails to provide sufficient volume for the required procedure. Nevertheless, from a biological standpoint, autologous tissue is superior. Autologous tissue possesses osseoinductive and osseoconductive properties, facilitating both bone regeneration and the necessary scaffold for supporting regenerated bone until it matures into lamellar bone.

A novel approach
In the past 15 years, a promising concept has been developed by biotechnology company, KometaBio Inc. (www.kometa bio.com) — the conversion of patient teeth into autologous dentin grafts. This solution harnesses the osseoinductive regenerative potential of human teeth. This concept involves converting extracted teeth into osseoinductive bone graft material, offering a personalized and biocompatible option for alveolar bone regeneration. Given the high similarity in composition between teeth and bone, coupled with the attraction of progenitor cells by dentin, grafts derived from teeth exhibit profound bioactivity.
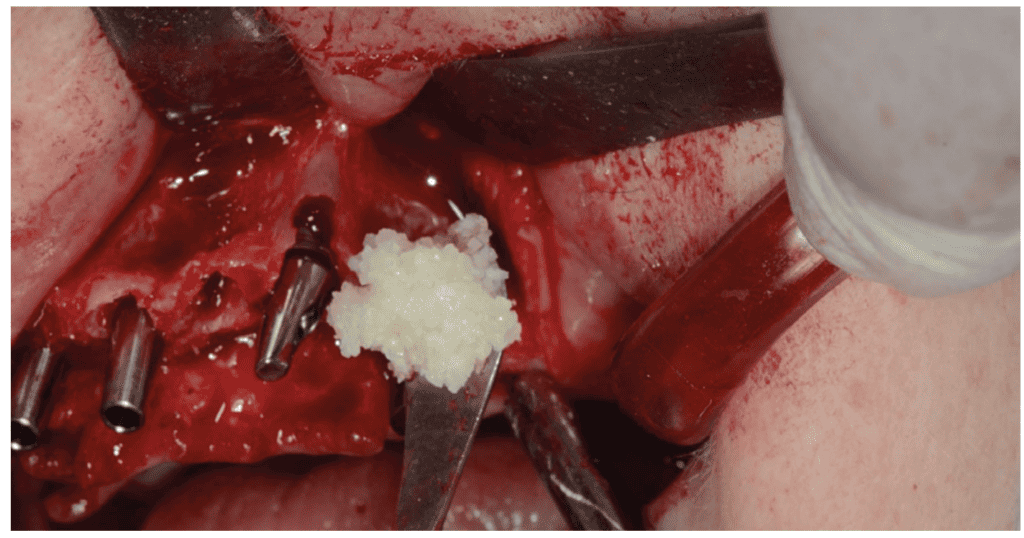
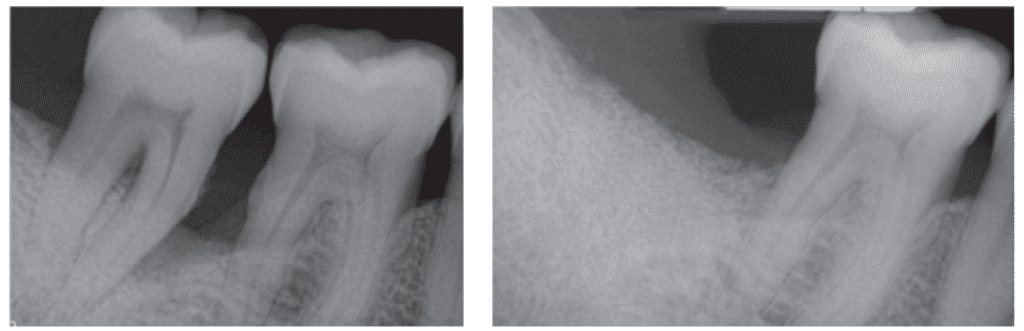
The process begins with the extraction of the patient’s natural tooth, a routine procedure performed by dentists and oral surgeons. The extracted tooth then undergoes mechanical and chemical cleansing to eliminate bacteria, infections, and any restorations such as composites, fillings, or endo materials (Figures 1A-1B). The tooth is subsequently pulverized into controlled particle sizes, presenting a user-friendly putty-like format (Figure 2). The resulting acellular scaffold retains the architectural and compositional traits of natural bone, making it an ideal substrate for bone regeneration (Figure 3). A tooth, rich in HA mineral, collagen fiber type I, growth factors, and BMPs, presents an excellent graft material, further enhanced by its autologous nature. The HA scaffold gradually resorbs, the collagen contributes to graft osseoinductive properties, and growth factors accelerate healing by attracting progenitor cells and signaling M2 macrophages, fostering osteoblastic activity. A dental assistant or doctor can transform any extracted tooth into an autologous dentin graft within 7-8 minutes chairside, following this protocol.

Upon implanting the Dentin Graft, a favorable microenvironment encourages osteogenic cell migration to the site. These cells then differentiate into osteoblasts, the bone-forming cells responsible for synthesizing the bone tissue’s extracellular matrix. This process mirrors natural bone formation, resulting in the gradual development of functional alveolar bone. Over time, the Dentin Graft slowly resorbs, revealing more collagen and growth factors, ultimately replacing the dentin with native bone after approximately 10-14 months. The newly formed bone maintains its dimensional integrity as lamellar bone (Figure 3).
Advantages of Autologous Dentin Graft
The use of patient teeth for osseoinductive bone grafting presents several notable advantages over traditional grafting methods:
- Predictability: The most significant advantage of using an autologous graft, like dentin grafts, is the enhanced predictability of treatment success. Studies indicate minimal loss in height and width after grafting with dentin grafts, maintaining horizontal and vertical dimensions close to the original level.
- Biocompatibility: As the graft material originates from the patient’s body, the risk of immune rejection and adverse reactions is significantly reduced, promoting biocompatibility and hastening the natural site healing process with minimal inflammation.
- Reduced morbidity: Unlike autologous bone, which demands a secondary surgical site for bone harvesting, teeth-derived grafts negate the need for additional invasive procedures, minimizing donor site morbidity and patient discomfort.
- Enhanced regenerative potential: The inherent osseoinductive properties of teeth-derived grafts facilitate the natural bone formation process, resulting in robust and functional bone regeneration.
- Sustainability: Repurposing extracted teeth for bone grafting offers a sustainable approach that recycles biological material that would otherwise be discarded.
- Soft tissue invagination prevention: Autologous dentin grafts demonstrate reduced risk of soft tissue invagination into the graft site, potentially eliminating the need for barrier membranes.
- Patient acceptance: Patients, informed about the autologous use of their own extracted teeth, often view grafting procedures more favorably, increasing their willingness to undergo the procedure.
- Cost efficiency: Dentin grafts offer a cost-effective graft option, with a single tooth generating between 1cc – 5cc of grafting material.
Scientific support
Over the past two decades, more than 120 studies have explored the characteristics and clinical aspects of dentin grafting. These studies have compared autologous dentin grafts with conventional grafts and examined specific indications. The common thread across this research is the consistent achievement of alveolar bone regeneration and maintenance over time through dentin grafting.
Conclusion
Bone grafting is increasingly prevalent in dentistry, whether for extraction socket rehabilitation, alveolar bone reconstruction, or implant success enhancement. The predictability of grafting outcomes plays a pivotal role. Opting for the best available options, particularly a matrix capable of inducing bone formation and acting as a long-term scaffold, is crucial. Extracted teeth present a perfect candidate for such a matrix. While teeth have long been used as an alternative graft material, the advances by KometaBio have streamlined their controlled and efficient utilization.
Read this CE by Dr. Armin Nedjat on how autologous bone grafting using extracted teeth devised by KometaBio can provide a readily available and effective grafting material here: https://implantpracticeus.com/ce-articles/autologous-bone-grafting-using-extracted-teeth/
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Amit Binderman holds an MBA degree in International Business from the University of California, Berkeley, and an Undergraduate degree in Physics and Chemistry from Tel-Aviv University, Israel. Prior to KometaBio, Amit built a dental implant company which was later sold. He then worked with various medical device companies and tech companies where he held VP Sales and VP Business Development positions. With KometaBio, Amit focuses on educating dentists from around the world on autologous regenerative solutions as a way of providing more predictable and higher standard of care to patients through the innovations that the company brings. The Smart Dentin Grinder®, KometaBio’s flagship product, enables dentists to repurpose extracted teeth into bioactive autologous grafts. Amit also oversees the scientific and clinical initiatives aimed at advancing autologous applications.
Amit Binderman holds an MBA degree in International Business from the University of California, Berkeley, and an Undergraduate degree in Physics and Chemistry from Tel-Aviv University, Israel. Prior to KometaBio, Amit built a dental implant company which was later sold. He then worked with various medical device companies and tech companies where he held VP Sales and VP Business Development positions. With KometaBio, Amit focuses on educating dentists from around the world on autologous regenerative solutions as a way of providing more predictable and higher standard of care to patients through the innovations that the company brings. The Smart Dentin Grinder®, KometaBio’s flagship product, enables dentists to repurpose extracted teeth into bioactive autologous grafts. Amit also oversees the scientific and clinical initiatives aimed at advancing autologous applications.
