Editor’s intro: In this case study, Dr. Robert J. Mikhli shows treatment of atraumatic extraction and socket preservation, reviews steps to achieve predictable and successful socket preservation, and discusses recommended materials and instruments.
Dr. Robert J. Mikhli discusses a technique for predictable and reproducible atraumatic extraction and socket preservation
Introduction
As procedures and techniques in dentistry continue to progress, several treatment techniques should be well understood to achieve predictable and successful clinical outcomes. Atraumatic extractions and proper bone grafts in dentistry are critical to achieve desirable esthetic results as well as an adequate foundation for implant placement. As practitioners, we need to know what steps are essential to properly accomplish an atraumatic extraction and socket preservation, and what some of the preferred instruments and materials are recommended. The purpose of this article is to examine the proper technique for atraumatic extraction, review steps to achieve predictable and successful socket preservation, and to discuss recommended materials and instruments.
Case description
A 62-year-old-female patient presented to the office with terminal case type III perio-dontitis1 with grade III mobility on tooth No.17 and terminal case type III periodontitis with grade II mobility, recurrent decay, open margins, and distal overhang on tooth No. 19. The patient desired a treatment plan that would remove tooth No. 17 immediately due to discomfort and persistent food trap and restore or replace tooth No. 19. The evaluation for an implant, No. 19, was made utilizing a visual clinical assessment, digital radiographs, and 3D CBCT.




Prior to surgery
Proper patient consent was obtained verbally and in writing. Blood pressure was obtained. Written details of the procedure were sent to the referring provider.



Stage 1: atraumatic extraction and bone grafting (conducted in two visits — due to patient need)
- Atraumatic extraction of tooth No. 17
- Atraumatic extraction of tooth No. 19
- Bone grafting for socket preservation site tooth No. 19
The patient was given 440 mg naproxen at the beginning of the procedure. Anesthetic included 20% benzocaine topical for L IA, LB. The total given was 3 carpules (1.7mL) of Septocaine® (Septodent USA), 4% with epinephrine 1:100,000, injected. Profound anesthesia was acquired.
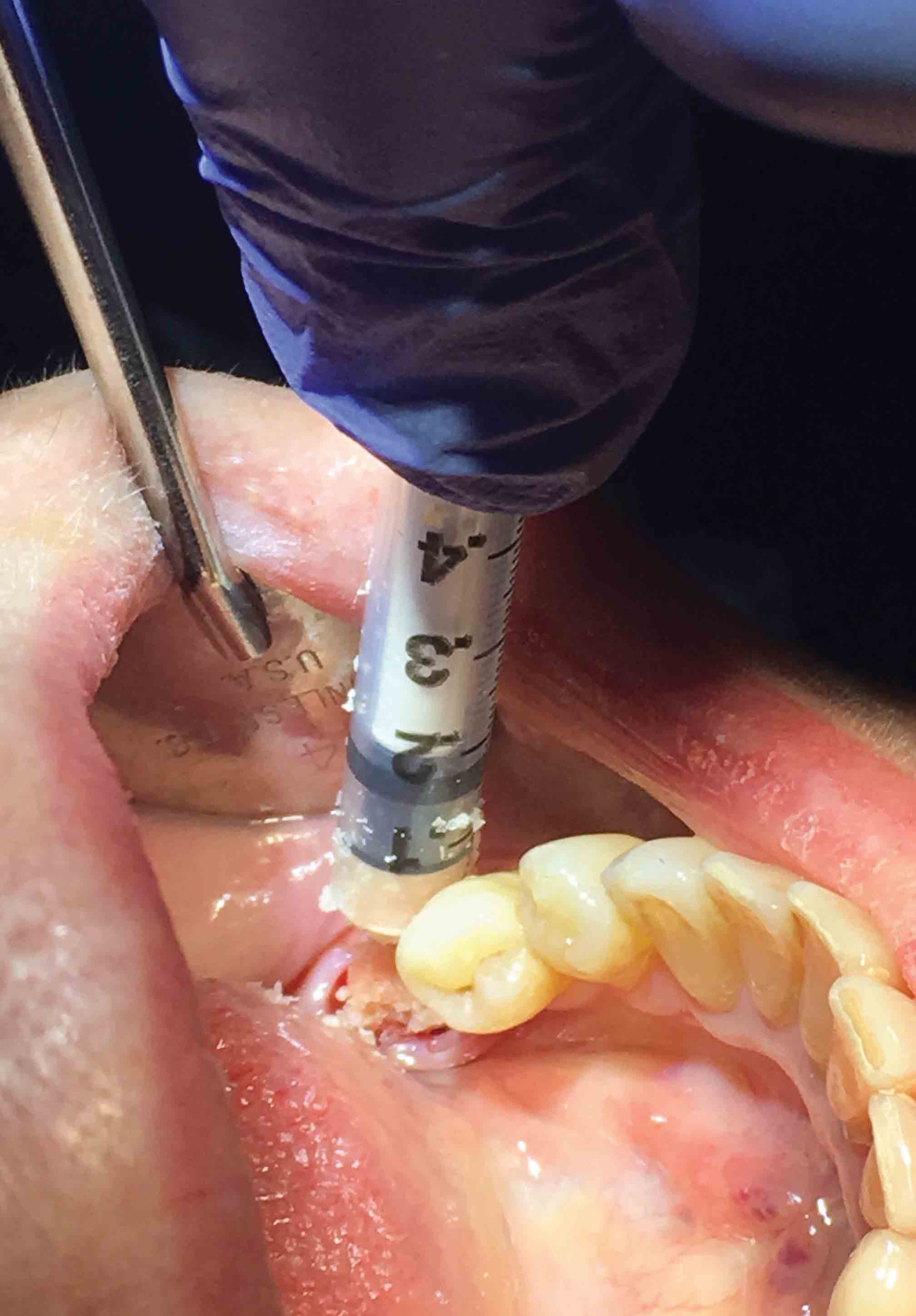
Teeth Nos. 17 (first visit) and 19 (second visit) were extracted atraumatically with an extraction kit (Karl Schumacher) consisting of periotome, proximators, and elevators to sever periodontal ligaments from the socket to preserve surrounding bone. Teeth were sectioned and removed. The socket was thoroughly debrided of all granulomatous tissue, and remaining periodontal ligament fibers with curettes and flushed with 0.12% chlorhexidine gluconate. 2 cc’s of demineralized cortical/cancellous allograft (250-1000 microns) (Karl Schumacher) was placed into the socket; HeliPLUG® (Miltex-Integra) absorbable collagen wound dressing was placed for graft containment; 2 resorbable 4-0 chromic sutures were placed. Postoperative instructions were given to the patient, and she was scheduled for 2-week post-up follow-up.

Stage 2: placement of implant
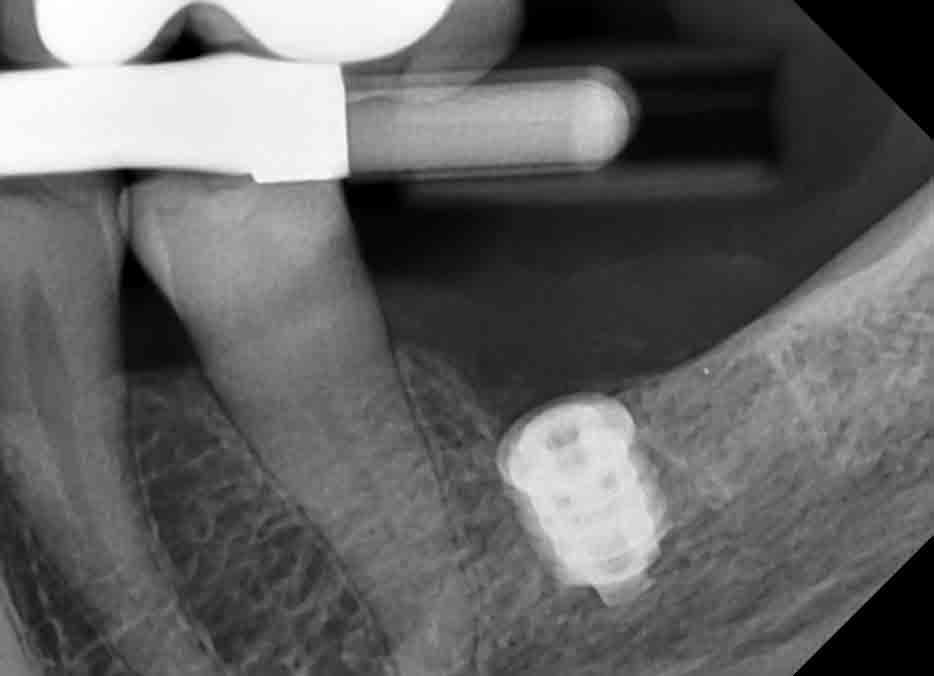
- Preoperative radiograph to evaluate allograft
- Placement of endosseous implant, site No. 19
The patient was given 440 mg naproxen at the beginning of the procedure. Anesthetic included 20% benzocaine topical for L IA, LB. The total given was 4 carpules (1.7mL) of Septocaine®, 4% with epinephrine 1:100,000, injected. Profound anesthesia was acquired.
Tissue was reflected to reveal the ridge. An osteotomy performed into site No. 19, implant (Blue Sky Bio Max) 5.0 x 6 mm placed, 1-2 mm subcrestal and torque of 20N/cm was obtained. A cover screw was placed. Four resorbable 4-0 chromic sutures were placed. Postoperative instructions were given to the patient, and she was scheduled for 2-week post-up follow-up and subsequent surgical uncovering after 4 months of healing, and referred back to referring provider for abutment and crown placement.
Stage 3: completion (at referring provider)
The final stage of the treatment plan, performed at the patient’s referring provider, was the placement of the abutment and crown.
Discussion
There are numerous treatment possibilities for a tooth with a terminal prognosis. What course of treatment and when to begin treatment is a collaborative effort that involves the patient, the dental team, and the referring provider. Proper understanding of the techniques and materials is vital in achieving predictable and successful clinical outcomes. The aforementioned treatment was initiated by the patient to resolve pain, discomfort, and food impaction while retaining at least one molar and maintaining proper occlusion. With the proper atraumatic extraction and preparation of an extraction site, the prognosis for a well-placed and integrated implant is possible. Restorative-wise, as clinicians, we can bypass cantilevers and removable prosthetics with well-placed implants. From the perspective of a patient, restoring a single tooth, having the ability to still place dental floss between his/her teeth, not damaging a healthy proximal tooth, or not having a prosthesis that needs to be removed and inserted periodically are significant motivators to elect for the placement of a dental implant.
Conclusion
Predictable and successful preparation of an area for implant placement is attainable with proper atraumatic extraction technique, proper socket preservation technique, and proper instruments and materials. Through a proper visual clinical exam, digital radiographs, and a 3D CBCT scan to screen the patient, the treatment can be carefully planned for each specific patient. When considering what the patients desire for their clinical outcome and understanding the most effective treatment modality to achieve the ideal outcome, the provider will need to determine the most effective way to educate the patients on the treatment path. Effective communication, addressing the desires of the patient, while conforming to proper clinical technique, will increase case acceptance. The key to effective communication is to make sure patients know what to expect before and after the procedure from their perspective. Most patients do not want to discuss the procedure itself, but rather patients want to know what they will feel, see, hear, and taste during the visits, and what will happen when they get home. Finally, make sure to provide a reasonable time line for surgical procedures. Although there can be additional clinical stages and patient visits, it has been the author’s experience that patients’ expectations are met and often exceeded when communication has been effective from the beginning.
Predictable and successful preparation of an area for implant placement is attainable!
For more information on a comprehensive suite of regenerative products to help with atraumatic extraction and socket preservation and other procedures, visit Implant Practice US’ website here.
- Wiebe CB, Putnins EE. The periodontal disease classification system of the american academy of periodontology — an update. J Can Dent Assoc.2000;66(11):594-597.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Robert J. Mikhli, DDS, is a top-rated dentist offering dental implants and oral surgery at Precision Implant Care, located in Brooklyn, New York’s Midwood neighborhood. Dr. Mikhli utilizes state-of-the-art surgical approaches and technology to restore oral health and enhanced esthetics to patients with damaged, diseased, or missing teeth. Dr. Mikhli is praised for both for his exceptional skill and ability to put patients at ease, including those who have avoided going to the dentist for years. Originally from Cleveland, Ohio, Dr. Mikhli has made New York his home since attending Yeshiva University in Manhattan, where he graduated with a Bachelor of Arts in Economics. Dr. Mikhli continued his education at Stony Brook School of Dental Medicine, earning his Doctor of Dental Surgery. Following dental school, Dr. Mikhli completed a 1-year General Practice Residency at New York Hospital of Queens, followed by an additional 1-year fellowship in oral and maxillofacial surgery and implantology, also at New York Hospital of Queens. The fellowship program provided Dr. Mikhli with extensive training in both the surgical and prosthetic aspects of implant dentistry.
Robert J. Mikhli, DDS, is a top-rated dentist offering dental implants and oral surgery at Precision Implant Care, located in Brooklyn, New York’s Midwood neighborhood. Dr. Mikhli utilizes state-of-the-art surgical approaches and technology to restore oral health and enhanced esthetics to patients with damaged, diseased, or missing teeth. Dr. Mikhli is praised for both for his exceptional skill and ability to put patients at ease, including those who have avoided going to the dentist for years. Originally from Cleveland, Ohio, Dr. Mikhli has made New York his home since attending Yeshiva University in Manhattan, where he graduated with a Bachelor of Arts in Economics. Dr. Mikhli continued his education at Stony Brook School of Dental Medicine, earning his Doctor of Dental Surgery. Following dental school, Dr. Mikhli completed a 1-year General Practice Residency at New York Hospital of Queens, followed by an additional 1-year fellowship in oral and maxillofacial surgery and implantology, also at New York Hospital of Queens. The fellowship program provided Dr. Mikhli with extensive training in both the surgical and prosthetic aspects of implant dentistry.

