Dr. Charles D. Schlesinger discusses the benefits of immediate-loading implants
Would your patients appreciate going from missing a tooth to having one in less than 40 minutes?
Today’s patients do not want to spend a lot of time in the dental chair and definitely do not want to spend 3-4 months to complete their implant treatment. If you are not able to provide what they are looking for, they will find a practitioner that can meet their needs.
[userloggedin]
But, if you treatment plan accordingly, evaluate each case independently, and patients meet the criteria necessary for immediate loading, this can be a reality in your practice.
In 2004, the International Team of Implantology (ITI) defined “immediate loading” as a restoration placed in occlusion with the opposing dentition within 48 hours of implant placement.1
With modern implants and a simplified surgical protocol, the ability to provide expedient and successful implant treatment can be accomplished by anyone with the skills to provide implant treatment. The key to implant success and especially important in immediate-loading treatment protocols is primary stability of the dental implant at the time of surgery.
Immediate loading of dental implants has been shown to be a viable treatment option with success rates that approach those of implants loaded after integration.2 The key to success is primary stability and OCO  Biomedical’s patented implant design. This design results in very high primary stability due its ability to be dual stabilized by the auger tip and the divergent imbedded tapered platform. The design modifies the biology around the implant due to its ability to create tension rather than compression on the bone. Kobayashi showed that this results in an environment conducive to promote accelerated osseointegration.3 The tension increases the expression of TGF-β1 and OPG that recruit osteoblasts and shuts down the activity of osteoclasts. This will prevent the normal dip in stability standard implants experience at 4-6 weeks.
Biomedical’s patented implant design. This design results in very high primary stability due its ability to be dual stabilized by the auger tip and the divergent imbedded tapered platform. The design modifies the biology around the implant due to its ability to create tension rather than compression on the bone. Kobayashi showed that this results in an environment conducive to promote accelerated osseointegration.3 The tension increases the expression of TGF-β1 and OPG that recruit osteoblasts and shuts down the activity of osteoclasts. This will prevent the normal dip in stability standard implants experience at 4-6 weeks.
Without this dip in stability and the high initial mechanical stability achieved with these implants, successful immediate loading is possible.4 The immediate application of mechanical stimulus of moderate intensity may even aid osseointegration, accelerating the response of the bone tissue in the healing phase.5
Clinical case
A 38-year-old female with no significant medical history presented to our clinic with a missing lower left first molar. This tooth had been extracted approximately 2 years prior by her general dentist. A CBCT was taken (Vatech America) at the consultation appointment. A significant amount of bone volume had been maintained with a slight sloping buccal defect (Figures 1 and 2). A 5.0 x 10 tissue level implant along with a flapless approach was treatment planned for the case.
Profound anesthesia was accomplished with 4% Septocaine® (Septodont USA) by local infiltrate of the soft tissue starting at the buccal and walking the anesthetic over the crest of the ridge to the lingual. A No. 8 carbide round bur on a high-speed handpiece was used to create an access through the soft tissue and divot the crestal bone (Figure 3). A 1.8 mm pilot drill with an 8 mm depth stop was taken to length, and then a paralleling pin was placed to assess the proposed implant position (Figure 4).

A 5 mm guided tissue punch was used to gain access to the crestal bone (Figure 5), and the resultant tissue plug removed with a No. 8 round bur. Since there was abundant keratinized soft tissue on the crest, a flapless approach was decided upon to decrease postoperative discomfort and healing time, and to facilitate immediate restoration if sufficient primary stability was achieved. The crestal bone was instrumented with a countersink (Figure 6). The countersink is crucial to assure that the micro-threads of the implant are completely encased in bone, and that the imbedded tapered platform seats without undue pressure on the surrounding crestal bone.
Once the crest has been prepared with the countersink, a 1.8 mm pilot drill with a 10 mm depth stop is taken to full length (Figure 7). This is then followed by a 5 mm osteotomy former (4.7 mm) to complete depth (Figure 8). A two-drill protocol allows for a rapid surgery. This is possible due to the unique step drill design of the osteotomy former, which eliminates the usual serial progression of burs typically associated with other systems. All site preparation was accomplished with an AEU-6000 implant motor and Mont Blanc® handpiece at 1200 rpm (Aseptico). The site is then rinsed with sterile saline, and the integrity of the osteotomy was checked with a small paddle curette.
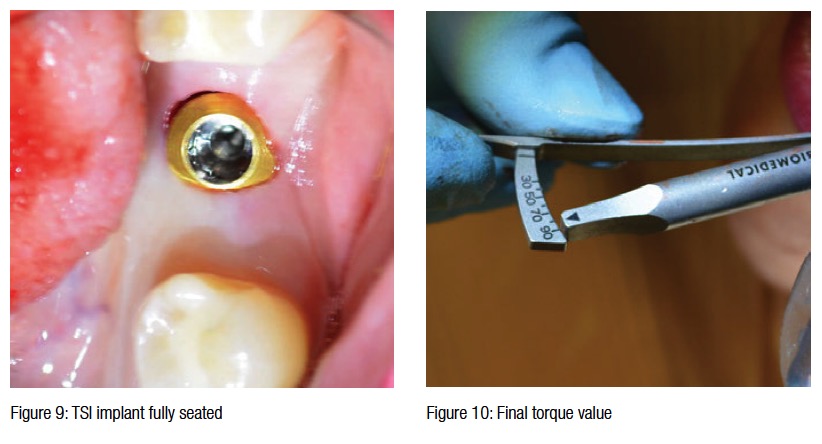
A 5.0 x 10 TSI implant (OCO Biomedical) was delivered to the site with the Ultem™ Delivery Cap. Once resistance was met, the cap was removed, and the implant was then driven to final position with a torque wrench. Final position is indicated when the restorative platform is approximately 1 mm-1.5 mm below the intended free gingival margin (Figure 9). A final delivery torque value of 90 N/cm was achieved (Figure 10). This is well above the 35 N/cm threshold that is required for successful immediate loading.6 Therefore, the decision to place a solid crown and bridge abutment and take the final impression was decided upon. Most implant companies will caution against such high insertion torque values, but with the OCO system, the high value is not from compressive forces, but rather from the implant reaching the bottom of the osteotomy, pulling bone in tension, and then condensing the bone around the auger tip.
 A solid crown and bridge abutment was torqued to 30 N/cm (Figure 11), and a profiling bur was used to remove excess tissue in preparation for the final impression (Figures 12 and 13). A tissue retraction impression pickup (TRIP) impression coping was snapped onto the implant to take the final impression. Light body VPS material was syringed (Figure 14) around and into the impression coping, and then heavy body material in a quadrant tray picked up the rest of the impression (Figure 15). A corresponding metallic implant analog was placed into the impression, and an opposing alginate was taken along with a blue bite registration. Utilizing a Protemp™ crown (3M ESPE) over an acrylic coping, a temporary was fabricated. The temporary was cemented with IRM temporary cement in full occlusion (Figure 16).
A solid crown and bridge abutment was torqued to 30 N/cm (Figure 11), and a profiling bur was used to remove excess tissue in preparation for the final impression (Figures 12 and 13). A tissue retraction impression pickup (TRIP) impression coping was snapped onto the implant to take the final impression. Light body VPS material was syringed (Figure 14) around and into the impression coping, and then heavy body material in a quadrant tray picked up the rest of the impression (Figure 15). A corresponding metallic implant analog was placed into the impression, and an opposing alginate was taken along with a blue bite registration. Utilizing a Protemp™ crown (3M ESPE) over an acrylic coping, a temporary was fabricated. The temporary was cemented with IRM temporary cement in full occlusion (Figure 16).
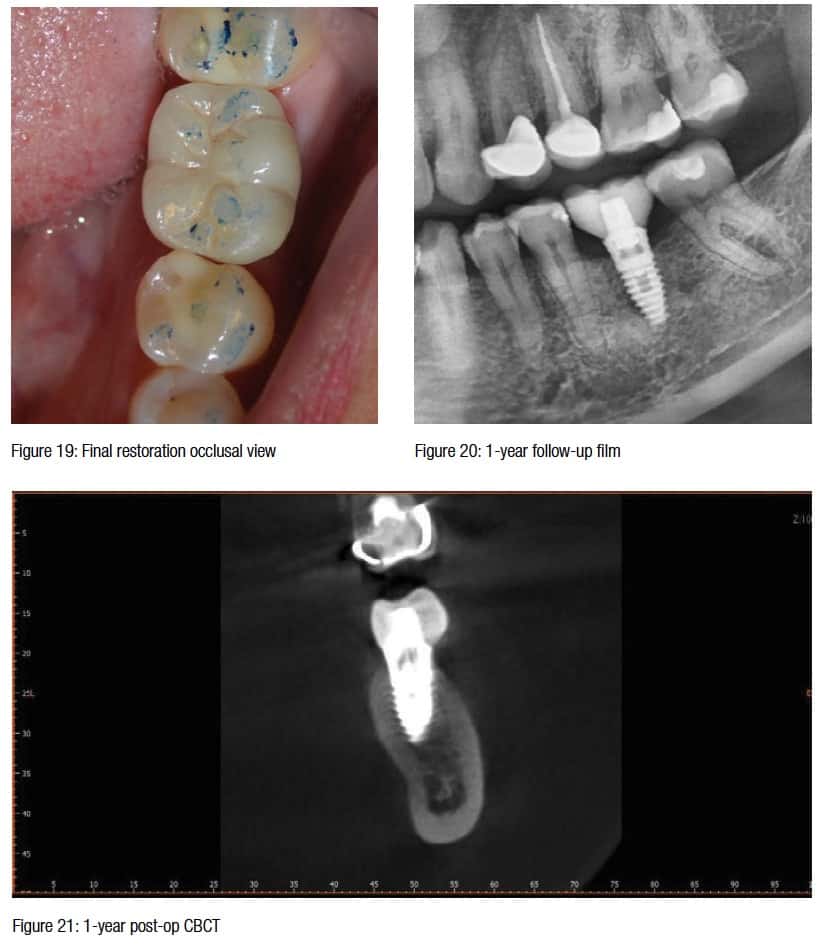
 Ten days later, the patient returned to the clinic for delivery and final cementation of a PFG crown. The temporary was removed, the abutment cleaned with a rotary prophy brush, and dried (Figure 17). The crown was checked for marginal integrity and the occlusion adjusted using articulation paper. Once the adjusted areas were repolished, the crown was cemented with Rely-X™ Dental Cement (3M) (Figures 18 and 19). Excess cement was removed, and the patient was dismissed.
Ten days later, the patient returned to the clinic for delivery and final cementation of a PFG crown. The temporary was removed, the abutment cleaned with a rotary prophy brush, and dried (Figure 17). The crown was checked for marginal integrity and the occlusion adjusted using articulation paper. Once the adjusted areas were repolished, the crown was cemented with Rely-X™ Dental Cement (3M) (Figures 18 and 19). Excess cement was removed, and the patient was dismissed.

The patient was seen 1-year later at follow-up (Figures 20 and 21). This type of healing is characteristic of these TSI implants. The patient has been asymptomatic and said that “Getting her implant hurt less than the crown she just received.”
The satisfaction level this patient experienced by having an implant placed along with the impressions and temporary in less than an hour is priceless when trying to build an implant practice. The single unit implant is the “bread and butter” of implantology. The more efficient the procedure is, the more satisfied your patients will be, and the more production you will produce per chair hour of time. Placing implants can be highly enjoyable when treatment is planned correctly, and practicing implantology this way can also make it one of the most rewarding aspects of your practice.
[/userloggedin]
[userloggedout][/userloggedout]
- Cochran DL, Morton D, Weber HP. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int J Oral Maxillofac Implants. 2004;19(suppl):109-113.
- Rizkallah N, Fischer S, Kraut RA. Correlation between insertion torque and survival rates in immediately loaded implants in the maxilla: a retrospective study. Implant Dent. 2013;22(3):250-254.
- Kobayashi Y, Hashimoto F, Miyamoto H, Kanaoka K, Miyazaki-Kawashita Y, Nakashima T, Shibata M, Kobayashi K, Kato Y, Sakai H. Force-induced osteoclast apoptosis in vivo is accompanied by elevation in transforming growth factor beta and osteoprotegerin expression. J Bone Miner Res. 2000;15(10):1924-1934.
- Schlesinger CD. Predictable Immediate Implant Stabilization and Restoration. J Implant Advanced Clin Dent. 2013;5(8):17-23.
- Linkow LI, Glassman PE, Asnis ST. Macroscopic and microscopic studies of endosteal bladevent implants (six month dog study). Oral Implantol. 1973;3(4):281-309.
- Glauser R, Lundgren AK, Gottlow J, Sennerby L, Portmann M, Ruhstaller P, Hämmerle CH. Immediate occlusal loading of Brånemark TiUnite implants placed predominantly in soft bone: 1-year results of a prospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):47-56.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores