Educational aims and objectives
This self-instructional course for dentists aims to review common problems and management at the dental implant-abutment connection.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Understand how platform switching is important in preserving crestal bone.
- Describe the microgap and its importance in implant
- Describe how excessive cement around an implant crown can result in implant failure.
- Explain the role of keratinized tissue around the implant.
- Understand how non-keratinized mucosa around an implant can cause inflammation.
- Explain the oral hygiene process for implant care.
Drs. Stuart Segelnick and Mea A. Weinberg discuss properties of dental implants that could influence long-term success and how to manage the implant-abutment connection.
Drs. Stuart Segelnick and Mea A. Weinberg review typical challenges and management at the dental implant-abutment connection
Introduction
Dental implants have a record of long-term success with a cumulative survival rate of about 96% up to 10 years post-loading.1,2 It is important to realize the various factors that can influence implant survival or failure. A higher rate of implant failure occurs in patients with a smoking history, hypertension without medication, and uncontrolled diabetes.3-5 In addition to systemic reasons, there are other properties of dental implants that could influence their long-term success, including crestal bone loss, placement of the platform at or below gingival margin, presence of excess cement from restoration cementation, presence of a microgap between the implant connector and the abutment, and non-submerged versus submerged implants. This article will review common problems and management at the dental implant-abutment connection.
Periodontal issues in implant failure
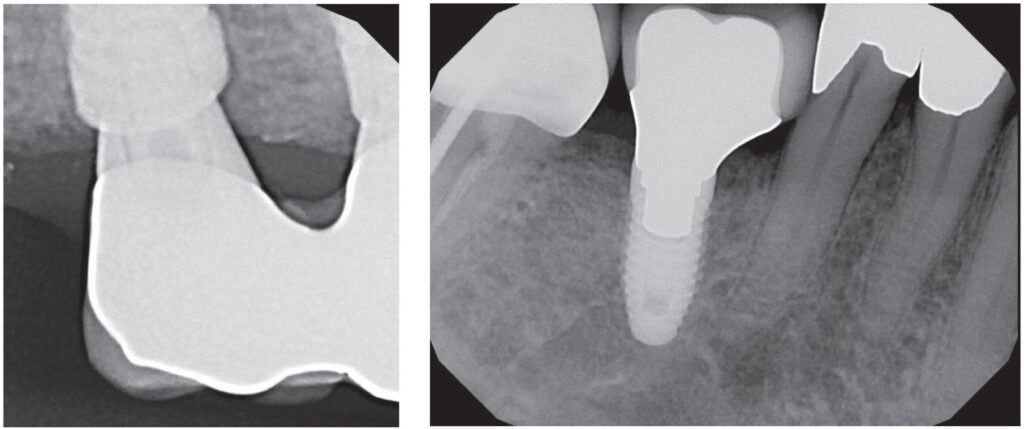
The first issue to consider is the location of the implant-abutment connection (IAC) in regard to the bone level. This is important when considering that excessive marginal bone loss can result in implant failure.6,7 The question is whether there is a difference in success rates between having the platform placed below crestal bone (termed subcrestal implants), or at the level of bone (termed bone-level implants).6,8 There are mixed results regarding bone level placements that reduce marginal bone loss. Some articles found no difference if implants were placed at the level of bone or subcrestally.9,10,6 However, most articles, including a systematic review and meta-analysis article, found that subcrestal placement of implants is ideal because there is less chance for the implant to become exposed, thereby increasing stability and reducing the risk of peri-implantitis.7,11 In the review article, it was concluded that recommendations are to place tissue level implants at the level of the crest and bone level implants subcrestally (Figure 1).12,13
Additionally, non-submerged implants stabilize the soft tissue seal around the implant, preventing abutment movement that affects the soft tissue seal and thus preserving marginal bone.13 On the other hand, non-submerged implants cannot transfer stress or masticatory load as well as submerged implants (implants placed below the gingival margin), which can lead to marginal bone resorption.14 Non-submerged implants are ideal for immediate and early loading.
The microgap, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in periimplantitis and bone loss.
Standard platform implants that range in size from 3.5 mm to 4.2 mm in diameter are available in shorter lengths and narrower diameters, which is ideal for the anterior area. Wide platform implants are ideal for the posterior area; the sizes available are 4.5 mm to 6 mm. To prevent crestal bone loss, the question arises whether the abutment should be platform-matched, whereby the abutment has the same diameter as the platform of the implant (Figure 2), or if the abutment should be platformed-switched (PLS), using a smaller diameter abutment on a larger diameter implant collar, making the implant-abutment connection (IAC) more distinct (Figure 3).15 This type of connection shifts the perimeter of the IAC inward toward the central axis of the implant, allowing a thicker soft tissue cuff around the implant prosthesis, which is easier to maintain. Lazzara and Porter have hypothesized that shifting the IAC inward also shifts the inflammatory cell infiltrate inward and away from the crestal bone.16
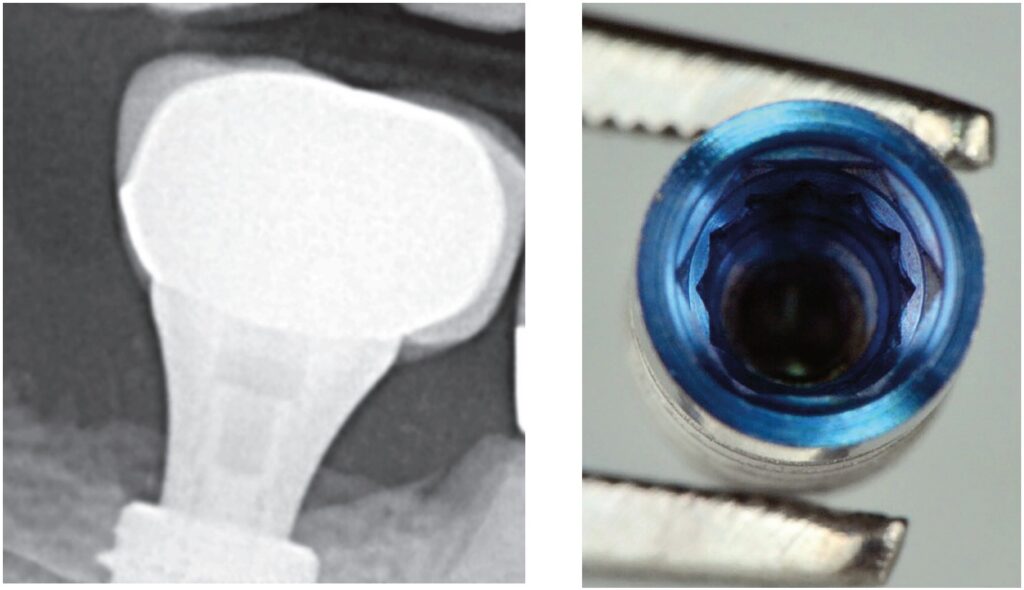
Platform switching, which was initially proposed by Gardner in 2005 and further described by Lazzara in 2006, is an IAC modification to control marginal bone loss (MBL) around an implant.16-18 Additionally, PLS is a process to improve long-term bone maintenance around implants as well as improved tissue response. A 2015 systematic review as well as the majority of more current articles conclude that the majority of clinical studies showed that there was significantly less mean MBL at implants with PLS versus platform-matching implant-abutment configuration.19,20 Mean crestal bone loss that was reported was 0.22 mm in platform-switched implants and 2.02 mm in non-platform-switched implants. Also, the reduction of the abutment width by the platform circumferentially of 0.45 mm is sufficient to avoid peri-implant bone loss.15 Before placing implants, the surgeon should consider using platform-switching, which not only increases the distance between IAC and the crestal bone, but also increases the microgap to crestal bone distance and thus potentially preserving crestal bone.21
The microgap, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in peri-implantitis and bone loss.22 The bacteria adhere and proliferate in this gap causing an increase in inflammation around the IAC during soft tissue manipulation for the crown insertion and during function.22 Since there is no complete seal at the IAC with any implant systems, it is ideal to have the smallest microgap between the implant and abutment and position it a distance from the outer perimeter of the implant. A pumping effect occurs when there is a larger microgap, allowing for bacterial movement inside and outside the connection during pressure changes as the restoration is loaded.6 A clinical review concluded that conical and mixed connections were better than implants with an external connector.22 An advantage of a one-piece implant is that there is no microgap; however, it must be cemented, and then there are possible problems with excess subgingival cement that is not removed. Ideally, the smallest amount of bone loss that occurs around implants is when the microgap between the abutment and implant is placed 1–2 mm above the bone (supracrestally).6,23 Other studies have shown tissue level implants can be restored with a screw-retained crown.24 Different studies found varied results relating the association of abutment height and marginal bone loss. Long abutments showed less interproximal marginal bone resorption than shorter abutments in screw-retained crowns and cement-retained crowns. It is speculated the decreased vertical height of the abutments would cause an encroachment on the supracrestal tissue attachment formation leading to an increase in bone loss around the implant.25,26
There are different implant-abutment connection systems used to support a single or multiunit restoration with the purpose of reducing stress on the prosthetic component and on the bone-implant interface and to provide good prosthetic stability.18 The platform may have an internal (internal hexagon, tri-lobe, and octagon)(Figure 4), conical (Morse taper), external (external hex), or tube-in-tube connection.27 The internal connection is best to reduce bone loss and increase implant stability.6 The majority of articles concluded that dental implants with internal connections showed less MBL than implants with external connections, which was the result of platform switching.28,29 Moreover, abutment disconnection and reconnection multiple times were found to significantly cause marginal bone loss compared to implants with final abutment placement at the time of implant placement.30 Thus, it is recommended to limit the removal of the abutment once it is placed.
Levine, Present, and Wilson described complications with excess cement around dental implants, precisely at the restoration-abutment connection. There are advantages and disadvantages of cement retention versus screw-retention crowns.31 Excessive remaining cement results in peri-implantitis which can lead to implant failure.32,33 Proper cementing technique is helpful to prevent excessive cement.34 Screw-retained restorations had 16.9% less inflammation than cemented restorations.35 One of the disadvantages of cement retention that can affect the IAC is the presence of excessive subgingival cement, and if the margins of the restorations were subgingival, particularly 2 mm or deeper, it made removal of excess cement difficult.36 Additionally, the time after cementation to finding signs of peri-implant disease was from 6 weeks to 4 months but can be up to many years.36 It is recommended that the margin of a restoration be either supragingival or no more than 1.5 mm subgingival.31 Ideally, it is recommended to have the restoration-abutment connection far from the IAC to reduce marginal bone loss and not impede on the implants supracrestal tissue attachment (once known as biologic width).37
Most evidence supports that implants with non-keratinized tissue allow for more oral biofilm (plaque) accumulation, marginal tissue recession, marginal inflammation and patient discomfort.38-41 One article found having < 2 mm of keratinized mucosa around an implant was a good indicator for future peri-implant disease.41
There are benefits in good oral biofilm control as well as regular professional maintenance visits in preventing peri-implant disease.42 It is important to have the proper instruments such as plastic instruments or plastic sleeves on ultrasonic power scalers to prevent damage to the peri-implant tissues as well as the implant.44 Titanium or plastic brushes, curettes, scalers, and lasers have all been used effectively in oral biofilm removal. More recent professional oral hygiene recommendations to reduce peri-implant inflammation include use of glycine powder air polishing and erythritol powder air polishing.45 Time must be taken to scale around implants due to the configuration of the restoration. When the emergence profile on a crown is ≥ 30 degrees and convex, it is more difficult to scale, thus increase the prevalence of peri-implantitis.46
Conclusion
There are many factors of the dental implant-abutment connection that can influence periodontal issues. Management of these potential problems should be addressed when possible by placing the platform subcrestally, platform switching, using longer abutments to place the restorative margin closer to the gingival soft tissue margin, decreasing abutment disconnection and reconnection times, using screw-retained abutments, having adequate keratinized gingiva, and limiting bulbous prostheses. Including these factors in treatment planning can help reduce inflammation, marginal bone loss, and implant failure. Ultimately, patients must be compliant with oral hygiene and maintenance care to have better outcomes of implant success.
After reading about how to avoid issues at the implant-abutment connection (and taking the quiz), read and take a quiz about another challenging issue — ingestion or aspiration of implant components. Read it here: https://implantpracticeus.com/ce-articles/a-serious-and-emerging-complication-in-implant-dentistry-ingestion-or-aspiration-of-implant-components/
References
- Moraschini V, Poubel LADC, Ferreira VF, Barboza EDSP. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg. 2015; 44(3):377-388.
- Howe MS, Keys W, Richards D. Long term (10-year) dental implant survival: A systematic review and sensitivity meta-analysis. J Dent. 2019:84:9-21.
- Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012;2(2):38-41.
- Wu X, Al-Abedalla K, Eimar H, et al. Antihypertensive medications and the survival rate of osseointegrated dental implants: A cohort study. Clin Implant Dent Relat Res. 2016;18(6):1171-1182.
- Wagner J, Spille JH, Wiltfang J, Naujokat H. Systematic review on diabetes mellitus and dental implants: an update. Int J Impl Dent. 2022;8(1).
- Kowalski J, Lappinska B, Nissan J, Lukomaska Szymanska M. Factors influencing marginal bone loss around dental implants: a narrative review. 2021;11(7):865.
- Galindo-Moreno P, Catena A, Pérez-Sayáns, et al. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin Implant Dent Relat Res. 2022; 24(5):630-642.
- Esposito M. Impact of 0.5mm vs 1.5 mm subcrestal implant placement on marginal bone and aesthetics – 3-year results of a multicenter RCT. Clin Oral Implants Res. 2019;30(S19):31.
- Nagarajan B, Murthay V, Lingstone D, Surendra MP, Jayaraman S. Evaluation of crestal bone loss around implants placed at equicrestal and subcrestal levels before loading: a prospective clinical study. J Clin Diagn Res. 2015;9(12): ZC47-ZC50.
- Sargolzaie N, Zarch HH, Arab H, Koohestani T, Ramandi MF. Marginal bone loss around crestal or subcrestal dental implants: prospective clinical study. J Korean Assoc Oral Maxillofac Surg. 2022;30;48(3):159-166.
- Chatterjee P, Shashikala R, Navneetham A. Comparative study of the crestal vs subcrestal placement of dental implants via radiographic and clinical evaluation. J Contemp Dent Pract. 2022;23(6):623-627.
- Palacios-Garzón N, Velasco-Ortega E, López-López J. Bone Loss in Implants Placed at subcrestal and crestal level: A systematic review and seta-analysis. Materials (Basel). 2019; 12(1):154-173.
- Saleh MHA, Ravidà A, Suárez-López del Amo, F, L GH, Asa´ad F, Wang HL. The effect of implant-abutment junction position on crestal bone loss: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018;20(4):617-633.
- Kim JC, Lee M, Yeo IL. Three interfaces of the dental implant system and their clinical effects on hard and soft tissues. Mater Horiz. 2022;9(5):1387-1411.
- Gupta S, Sabharwal R, Nazeer J, et al. Platform switching technique and crestal bone loss around the dental implants: A systematic review. Ann Afr Med. 2019;18(1):1-6.
- Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent.2006;26(1):9-17.
- Gardner DM. Platform switching as a means to achieving implant esthetics. N Y State Dent J. 2005;71(3):34-37.
- Singla S, Kumar L, Rathee M. Know your implant connections. African Journal of Oral Health. 2018;6(2).
- Strietzel FP, Neumann K, Hertel M. Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis. Clin Oral Implantsl Res. 2015;26:342-358.
- Tokgöz SE, Bilhan H. The influence of the implant abutment complex on marginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
- Nayak R, Devanna R, Dharamsi AM, et al. Crestal bone loss around dental implants: platform switching vs platform matching – A retrospective study. J Contemp Dent Pract. 2018;19(5):574-578.
- Lauritano D, Moreo G, Lucchese A, et al., The impact of implant-abutment connection on clinical outcomes and microbial colonization: a narrative review. 2020;13(5):1131.
- Piattelli A, Vrespa G, Petrone G, et al. Role of the microgap between implant and abutment: A retrospective histologic evaluation in monkeys. J Periodontol. 2003;74(3):346-352.
- Agustín-Panadero R, Bermúdez-Mulet I, Fernández-Estevan L, et al. Peri-Implant Behavior of Tissue Level Dental Implants with a Convergent Neck. Int J Environ Res Public Health. 2021; 18(10):5232.
- Blanco J, Pico A, Caneiro L, Nóvoa L, et al., Effect of abutment height on interproximal implant bone level in the early healing: A randomized clinical trial. Clin Oral Implants Res. 2018;29(1):108-117.
- Spinato S, Galindo-Moreno P, Bernardello F, Zaffe D. Minimum abutment height to eliminate bone loss: influence of implant neck design and platform switching. Int J Oral Maxillofac Implants. 2018;33(2):405-411.
- Bittencourt ABBC, Neto CLMM, Penitente PA, et al. Comparison of the Morse Cone Connection with the Internal Hexagon and External Hexagon Connections Based on Microleakage – Review. Prague Med Rep. 2021;122(3):181-190.
- de Medeiros RA, Pellizzer EP, Filho AJV, dos Santos DM, da Silva EVF et al. Evaluation of marginal bone loss of dental implants with internal or external connections and its association with other variables: A systematic review. J Prosthet Dent. 2016;116(4):501-506.
- Kim DH, Kim HJ, Kin S, et al. Comparison of marginal bone loss between internal- and external-connection dental implants in posterior areas without periodontal or peri-implant disease. J Periodontal Implant Sci. 2018;48(2):103-113.
- Koutouzis T, Gholami F, Reynolds J, Lundgren T, Kotsakis GA. Abutment disconnection/reconnection affects peri-implant marginal bone levels: A meta-analysis. Int J Oral Maxillofac Implants. 2017;32(3):575-581.
- Levine RA, Present S, Wilson Jr. TG. Complications with excess cement and dental implants: Diagnosis, recommendations and treatment of 7 clinical cases. Implant Realities. 2014;1:51-159.
- Pesce P, Canullo L, Grusovin MG, et al. Systematic review of some prosthetic risk factors for periimplantitis. J Prosthet Dent. 2015;114(3):346-350.
- Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of periimplant disease – a systematic review. Clin Oral Implants Res. 2017; 28(10):1278-1290.
- Reda R, Zanza A, Cicconetti A, et al. A systematic review of cementation techniques to minimize cement excess in cement—retained implant restorations. Methods Protoc. 2022;5(1):9.
- Agustín-Panadero R, Bustamante-Hernández N, Labaig-Rueda C, et al. Influence of biologically oriented preparation technique on peri-implant tissues; prospective randomized clinical trial with three-year follow-up. Part II: Soft tissues. J Clin Med. 2019;8:2223.
- Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.
- Tokgöz SE, Bilhan H. The influence of the implant-abutment complex on marginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
- Kungsadalpipob K, Supanimitkul K, Manopattanasoontorn S, et al. The lack of keratinized mucosa is associated with poor peri-implant tissue health: a cross-sectional study. Int J Implant Dent. 2020;6(1):28.
- Kamal, RK. Necessity of Keratinized Tissue Around Dental Implants to Maintain Peri-Implant Tissue Health: A Systematic Review. Dental Theses. 2018;33.
- Saltz AE. Impact of keratinized mucosa in dental implant treatment. Decisions in Dentistry. 2020;6(8):40-44.
- Grischke J, Karch A, Wenzlaff A, et al. Keratinized mucosa width is associated with severity of peri-implant mucositis. A cross-sectional study. Clin Oral Implants Res.2019;30(5):457-465.
- Cortellini S, Favril C, De Nutte M, Teughels, Quirynen M. Patient compliance as a risk factor for the outcome of implant treatment. Periodontology 2000. 2019; 81(1):209-225.
- Gulati M, Govila V, Anand V, Anand B. Implant Maintenance: A Clinical Update. Int Sch Res Notices. 2014; 9:908534.
- Baldi D, De Giorgis L, Menini M, Motta F, Colombo J. Efficacy of Instruments for Professional Oral Hygiene on Dental Implants: A Systematic Review. Appl Sci. 2022;12(1):26-44.
- Tan SL, Grewal GK, Mohamed Nazari NS, Mohd-Dom TN, Baharuddin NA. Efficacy of air polishing in comparison with hand instruments and/or power-driven instruments in supportive periodontal therapy and implant maintenance: a systematic review and meta-analysis. BMC Oral Health. 2022;22(1):85-102.
- Yi Y, Koo KT, Schwarz F, Amara HB, Heo-SJ. Association of prosthetic features and periimplantitis: A cross-sectional study. J Clin Periodontol. 2020; 47(3):392-403.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Stuart Segelnick, DDS, MS, is immediate past president of the American Association of Dental Editors and Journalists. He is editor of the Northeastern Society of Periodontists NESP Bulletin and the Second District Dental Society of New York SDDS Bulletin. Dr. Segelnick has co-edited five books on dentistry. He is a Diplomate of the American Board of Periodontology and the International Congress of Oral Implantologists. Dr. Segelnick is an Adjunct Clinical Professor at NYU Dentistry in the Department of Periodontology and Implant Dentistry.
Stuart Segelnick, DDS, MS, is immediate past president of the American Association of Dental Editors and Journalists. He is editor of the Northeastern Society of Periodontists NESP Bulletin and the Second District Dental Society of New York SDDS Bulletin. Dr. Segelnick has co-edited five books on dentistry. He is a Diplomate of the American Board of Periodontology and the International Congress of Oral Implantologists. Dr. Segelnick is an Adjunct Clinical Professor at NYU Dentistry in the Department of Periodontology and Implant Dentistry. Mea A. Weinberg, DMD, MSD, RPh, is a clinical professor in the Department of Periodontology and Implant Dentistry at New York University College of Dentistry. A Diplomate of the American Board of Periodontology, she has published many articles, chapters, and books on periodontics and pharmacology.
Mea A. Weinberg, DMD, MSD, RPh, is a clinical professor in the Department of Periodontology and Implant Dentistry at New York University College of Dentistry. A Diplomate of the American Board of Periodontology, she has published many articles, chapters, and books on periodontics and pharmacology.

