Dr. Charles D. Schlesinger discusses a simple and versatile instrument
Does a clinician really have to have the “latest and greatest”? Believe me, I am a huge advocate of using the very best technology to achieve better results in less time. I wholeheartedly embrace the technologies that not only make me a better practitioner, but also those things with which I surround myself that improve my quality of life.
[userloggedin]
Our industry is chock-full of devices. Dentists love gadgets, and I am no exception. Over my career, there have been those “latest and greatest” things that have looked great and performed as advertised and those that did not live up to their intended greatness.
In implantology, like the rest of dentistry, we are bombarded every day by manufacturers with the newest, the best, and the most innovative products known to man. The problem is there can be the erroneous assumption that “more complex” is analogous to innovation. We can be easily sucked into thinking that the more “gimmicky” a procedure is that it must perform to a higher standard and give better results than the “lower tech” devices we have been using.
When it comes to implantology, one of the most simple instruments is also the most versatile. I am speaking of the crude-looking, often overlooked osteotome. In the right hands and used properly, this simple set of instruments can achieve so much and do it in a predictable, well-proven manner.
 What is an osteotome?
What is an osteotome?
Basically an osteotome is a tapered or straight-walled instrument with a handle that can be manipulated by hand or tapped with a surgical mallet (Figure 1). It comes in two main varieties, convex- (Figure 2) and concave- (Figure 3) tipped, and are also are available in both straight and offset configurations. The offset style allows the osteotome to be placed in the posterior maxilla while allowing the force of the instrument to be directed vertically.
These instruments usually are available in matched sets that start with a small diameter and incrementally enlarge to a wider diameter. There are both generic kits and those that are matched to the taper of the specific implant you are using. My personal choice is to use a set that is tapered to match the implant system I am utilizing since it not only has the correct taper for the implant, but also has the specific implant lengths laser etched on the shaft (Figure 4). When used to either expand or compact bone, it allows for more predictable primary stability upon implant insertion.
Why is an osteotome so versatile, and what can it do?
Depending on the tip style used, osteotomes can be used to expand bone, change the consistency of medullary bone, or up-fracture the sinus floor in a crestal-approach sinus elevation.
Bone expansion
After growth has ceased, the single most important factor governing the gross morphological shape of the bone is related to the presence or absence of the teeth. After tooth extraction, there follows a phase of remodeling that may result in an extensive loss in the height of the jaws.1 It is not uncommon to lose a significant amount of bone volume in a relatively short period of time (Figure 5). This loss in volume can be accelerated as a result of trauma at the time of surgery, advanced periodontal disease, and the constant pressure of a removable appliance. Knife-edge residual alveolar bone ridges or non-space-maintaining defects of the alveolar bone limit or complicate the successful placement of dental implants.2
As the bone is reduced in height by periosteal osteoclastic resorption, there is an accompanying endosteal apposition,3 but at no time is new bone formation seen on the periosteal surface of the residual ridge, which remains porous, never developing a complete cortical layer.4,5 Further internal remodeling results in a loss of organization and a thinning of the trabeculae as well as disruption in the arrangement of the lamellar and Haversian systems.6
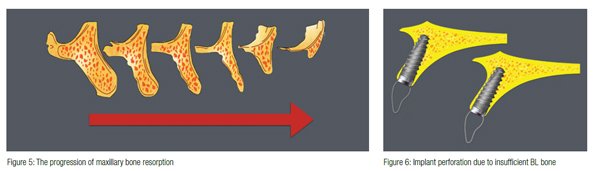 Many times, the loss of horizontal bone volume will not allow a conventionally sized implant to be placed using standard drilling protocols (Figure 6). In these cases, if the osteotomy is created using drills, the removal of bone will result in an insufficient thickness of bone either buccally, lingually, or in both areas. For successful integration, at least 1-2 mm of bone must remain in these areas in order to avoid potential dehiscence of the implant.
Many times, the loss of horizontal bone volume will not allow a conventionally sized implant to be placed using standard drilling protocols (Figure 6). In these cases, if the osteotomy is created using drills, the removal of bone will result in an insufficient thickness of bone either buccally, lingually, or in both areas. For successful integration, at least 1-2 mm of bone must remain in these areas in order to avoid potential dehiscence of the implant.
 In the maxillary arch, with its thinner buccal cortical walls, it is possible to “bend” the bone outward to accommodate the desired implant diameter without compromising the remaining bone thickness. The other side effect of this type of site preparation is the compaction of the bone to help it stand up better to the lateral forces that will be placed against it when the implant is eventually restored. For this type of procedure, an osteotome with a convex profile is recommended.
In the maxillary arch, with its thinner buccal cortical walls, it is possible to “bend” the bone outward to accommodate the desired implant diameter without compromising the remaining bone thickness. The other side effect of this type of site preparation is the compaction of the bone to help it stand up better to the lateral forces that will be placed against it when the implant is eventually restored. For this type of procedure, an osteotome with a convex profile is recommended.
Here we can see a case where there is plenty of vertical bone in the area of tooth No. 10, but is sorely lacking in BL volume (Figure 7). This lack of bone volume necessitates either a mini-implant placement or expansion to accommodate a standard diameter implant. By using a straight, convex-tipped osteotome, the ridge was expanded in order to accommodate a 3.0-mm implant (Figure 8).
Bone compaction
The primary stability of an implant is proportionate to the consistency of the bone in which it is being placed. The literature has defined primary stability as 30N/cm upon seating torque or an ISQ reading of 55 with an Osstell unit.7 Many times the native bone quality will not allow this minimal stability to be achieved, let alone the stability necessary to immediately load a dental implant. The maxillary arch usually demonstrates a bone quality of D3 or D4, but it is not uncommon to also see it in the mandibular arch in geriatric patients (Figure 9). These bone density types have the consistency of balsa wood and Styrofoam™, respectively. You wouldn’t want to try and hang an expensive piece of art on a wall that was made of either of these materials would you?
These poor bone types usually arise from medullary bone that has a sparse or open trabecular pattern and is most commonly found in the posterior maxillary arch. The posterior maxilla has the lowest bone mineral density8 even when compared to the premaxilla and, therefore, may require additional procedures to make the site suitable for implant placement.
Instead of moving through your progression of drills to create your final osteotomy, a series of incrementally increasing diameter osteotomes are used after a pilot hole in the intended trajectory has been established (Figure 10). By using a convex-tipped osteotome, we can condense the trabecular bone and thereby change the consistency of it. By slowly compressing the bone rather than cutting it away, the trabeculae will condense and thereby mimic denser bone in quality, essentially producing bone with better characteristics to achieve sufficient initial implant primary stability (Figure 11).
 Sinus elevation
Sinus elevation
A maxillary sinus can be lifted with either a lateral or osteotome-facilitated crestal approach (Figure 12).
Prior to the use of osteotomes for sinus elevation, the lateral wall or Caldwell-luc approach was the standard of care. In the 1980s, both Tatum9 and Misch reported success with the elevation of the sinus floor through the lateral wall of the maxilla. This procedure works very well and in many cases is still the chosen method for gaining alveolar bone height, but by its nature is a more invasive approach to elevation with a relatively long healing time.
In 1994, Dr. Robert Summers, using a special set of matched and tapered osteotomes, proposed a method for inserting implants in the posterior maxilla. Summers’ method has made the crestal approach less traumatic and invasive when placing implants coronal to the sinus floor.10
The procedure is quite elegant in its simplicity. A pilot drill is used to within 1 mm of the sinus floor to establish the intended implant trajectory. Now, using progressively larger instruments, the osteotomy is created. With the final diameter osteotome, the floor is up-fractured (Figure 13) by gentle tapping with a mallet. Either a convex or concave tip can be used, and each has its advantages and disadvantages.
The convex-tipped osteotome has the advantage of condensing the bone circumferentially around the site and will up-fracture the floor using slightly less force. But the disadvantage of this type of tip is that the up-fracure can be unpredictable. The floor can splinter, and the possibility of perforation of the Schneiderian membrane is potentially higher.
 The concave-tipped style of osteotome will not condense the bone to the same extent as the convex tip since the leading edge of the concave instrument will shave off bone as it progresses. This contributes to the advantage of having bone collecting in the concavity and being pushed ahead of the instrument. This bolus of bone will help buffer the trauma to the floor and have the side effect of decreasing the potential for membrane tearing. This bone along with grafting material of your choice will be added to hydraulically lift the membrane (Figure 14). With this technique being utilized in multiple adjacent sites, it is possible to achieve a significant lift (Figure 15).
The concave-tipped style of osteotome will not condense the bone to the same extent as the convex tip since the leading edge of the concave instrument will shave off bone as it progresses. This contributes to the advantage of having bone collecting in the concavity and being pushed ahead of the instrument. This bolus of bone will help buffer the trauma to the floor and have the side effect of decreasing the potential for membrane tearing. This bone along with grafting material of your choice will be added to hydraulically lift the membrane (Figure 14). With this technique being utilized in multiple adjacent sites, it is possible to achieve a significant lift (Figure 15).
Conclusion
The key to proper expansion, compaction, and elevation is a slow, gradual technique with controlled force application that leads to the desired result with minimal site trauma. The outcome of dental implant placement in terms of implant survival seems to be similar to that of implants placed by means of the conventional implantation technique.11
As a practitioner, my goal is to use the simplest protocols that will give me the consistent results I desire and my patients expect. It is easy to get caught up in the newest device or protocol, and it is our responsibility to explore everything that may prove to be a better way to do things, but do not abandon what is tried and true. Sometimes not being on the “bleeding edge” gives better and more consistent results. So, slap in that 8-track, crank up the volume, and embrace what works!
- Kingsmill VJ. Post-extraction remodeling of the adult mandible. Crit Rev Oral Biol Med. 1999;10(3):384-404.
- Siddiqui AA, Sosovicka M. lateral bone condensing and expansion for placement of endosseous dental implants: a new technique. J Oral Implantology. 2006;32(2):87-94.
- Pudwill ML, Wentz FM. Microscopic anatomy of edentulous residual alveolar ridges. J Prosthet Dent. 1975;34(4):448-455.
- Neufeld JO. Changes in the trabecular pattern of the mandible following the loss of teeth. J Prosthet Dent. 1958;8(4):685-697.
- Atwood DA. Post-extraction changes in the adult mandible illustrated by microradiographs of midsagittal sections and serial cephalometric roentgenograms. J Prosthet Dent. 1963;13:810-824.
- Seipel CM. Trajectories of the jaws. Acta Odontol Scand. 1948;8(2):81-191.
- Schlesinger C. Torque versus RFA in implant placement: a case study. Implant Practice US. 2016;9(4):14-20.
- Devlin H, Horner K, Ledgerton D. A comparison of maxillary and mandibular bone mineral densities. J Prosthet Dent. 1998;79(3):323–327.
- Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30(2): 207-229.
- Drew HJ, Chiang T, Simon BI. The osteotome technique: modifications to the original approach. Inside Dentistry. 2007;3(10):58-65.
- Shalabi MM, Manders P, Mulder J, Jansen JA, Creugers NH. A meta-analysis of clinical studies to estimate the 4.5 year survival rate of implants placed with the osteotome technique. Int J Maxillofac Implants. 2007;22(1):110-116.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Dr. Charles Schlesinger, DDS, FICOI, is a dental implant educator and clinician who has been lecturing internationally for the past 10 years. He graduated with honors from The Ohio State College of Dentistry in 1996. After graduation, he completed a General Practice residency at the VAMC San Diego and then went on to become the Chief Resident at the VAMC West Los Angeles. During his time in Los Angeles, he completed extensive training in oral surgery, implantology, and advanced restorative treatment. Once he completed his residency, Dr. Schlesinger maintained a thriving restorative and implant practice in San Diego, California, for 14 years. In 2012, he relocated to Albuquerque, New Mexico, to become the Director of Education and Clinical Affairs for OCO Biomedical. In 2013, he took over as Chief Operating Officer of OCO Biomedical along with his clinical responsibilities. In 2016, Dr. Schlesinger left OCO Biomedical and founded The CD Schlesinger Group, LLC, to help practitioners gain knowledge and experience with implants and became a Key Opinion Leader for The Hahn Implant System. Additionally, he continues to provide comprehensive implant care to patients in a private practice setting in Albuquerque, New Mexico.
Dr. Charles Schlesinger, DDS, FICOI, is a dental implant educator and clinician who has been lecturing internationally for the past 10 years. He graduated with honors from The Ohio State College of Dentistry in 1996. After graduation, he completed a General Practice residency at the VAMC San Diego and then went on to become the Chief Resident at the VAMC West Los Angeles. During his time in Los Angeles, he completed extensive training in oral surgery, implantology, and advanced restorative treatment. Once he completed his residency, Dr. Schlesinger maintained a thriving restorative and implant practice in San Diego, California, for 14 years. In 2012, he relocated to Albuquerque, New Mexico, to become the Director of Education and Clinical Affairs for OCO Biomedical. In 2013, he took over as Chief Operating Officer of OCO Biomedical along with his clinical responsibilities. In 2016, Dr. Schlesinger left OCO Biomedical and founded The CD Schlesinger Group, LLC, to help practitioners gain knowledge and experience with implants and became a Key Opinion Leader for The Hahn Implant System. Additionally, he continues to provide comprehensive implant care to patients in a private practice setting in Albuquerque, New Mexico.

