Dr. Martin Wanendaya presents an award-winning case study that required careful consideration of the soft tissues to ensure a successful result

[userloggedin]

This patient had worried about her loose “fang” for a number of years, and it had taken two referrals to our practice before she finally attended (Figures 1-9).
Being a teacher to teenagers in an inner city school, the patient was very aware of her smile. She expressed a concern about turning up to school without a tooth or, even worse, having it fall out during a lesson. Ideally, therefore, the patient was looking for the UR3 to be replaced with a fixed solution. She was expressly against dentures.
The UR3 had been loose for a long time and had now started to become visible when she smiled. Though the patient had had previous periodontal disease, her current periodontal condition was stable in all areas, aside from some pocketing around the UR3 and LR6.
An initial radiographic assessment showed extensive bone loss between the UR3 and the UR4 (Figure 10). A periodontal assessment presented probing depths of 6 mm-8 mm on the distal part of the UR3, which was grade 3 mobile. Nevertheless, the patient’s other teeth were unaffected by this localized, yet aggressive periodontal issue.
Treatment
Having extensively discussed the complexity of this case with the patient, she declined bone grafting as a treatment option. Additionally, she refused a temporary denture for the extent of the treatment.
Therefore, the following treatment plan was established:
- Initial assessment and radiographs
- Periodontal treatment on the LR6
- Extract UR3 and Maryland bridge
- Review periodontal health of LR6 and healing around UR3
- Diagnostic wax-up and final diagnostic radiographs
- Final treatment plan
- Surgery — place implant at UR3 and soft tissue manipulation to bring soft tissue from the palatal to the buccal side of the ridge
- Expose UR3 implant, and during the exposure, move tissue from the buccal to the palatal aspect of the ridge
- Provisional crown on UR3, await soft tissue maturation. Further soft tissue surgery, if needed
- When soft tissue has matured and patient is happy with provisional restoration, make final restoration
- Long-term maintenance and regular oral hygiene visits
After consent was obtained, the UR3 was removed and replaced with a provisional Maryland bridge. The tooth’s removal revealed a significant defect (Figures 12 and 13), and while the patient was shown the extent of this defect (Figures 14-16), she was adamant that she did not want a bone graft. Instead, having seen the long tooth present, she decided she was happy to have an implant crown with pink porcelain.




After a period of 6 months, where the patient’s bony and soft tissue had a chance to heal, the clinical situation was revealed. Unfortunately, it remained the case that the patient still presented a very long tooth (Figure 17).
A 3.5 mm x 14 mm ANKYLOS® C/X implant (Dentsply Implants) was then placed 1 mm subcrestally (Figure 18). During placement, a split thickness incision was made, and palatal soft tissue was moved buccally in an attempt to improve the soft tissue defect. An impression was taken at surgery.
From the fixture head impression, an abutment was selected and trimmed (Figure 19), and a temporary crown was fabricated. The metalwork was constructed, and a space for a lateral screw was made palatally (Figure 20).
The implant was then exposed (Figures 21-23) after a period of healing, during which a remote palatal incision was made, and palatal soft tissue was again moved buccally to reduce the soft tissue defect. Careful manipulation of the soft tissue and shaping of the provisional to reduce pressure on the tissue was carried out.


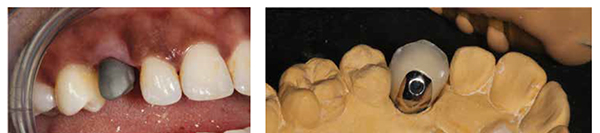
After 8 weeks of soft tissue healing and further shaping of the provisional, a metalwork pickup impression was taken and sent to the laboratory (Figure 24). The final crown was fabricated with palatal access for a lateral screw (Figure 25).

At the final fit appointment, the crown was fitted with both TempBond™ (Kerr) and a lateral screw for added retention. The patient was ecstatic with the result (Figure 26).
The 2-year review showed stable soft tissue, and the formation of mesial and distal papillae (Figure 30). The final result showed the improvement in the papilla as well as the stability of the soft tissue (Figures 31 and 32).


Reflective summary
The patient is delighted with the result of this treatment, and as a clinician, it is always very rewarding to improve function while ensuring an esthetically pleasing result. And indeed, this case provided many interesting learning opportunities.
The main challenge in this case was predicated upon the patient’s early decision to forgo bone augmentation, and that she only wanted to treat the UR3.
She also ruled out two of the other options we discussed:
- Bone graft on the UR3 site — this would have improved the bone height but not to the ideal level as the bone level on the UR4 was halfway down the root, and this level will have been the limit of any vertical augmentation.
- Removal of the UR4 and then grafting the UR3/UR4 site to increase the vertical height of the bone present before placing two implants in the UR3 and UR4 areas. This option would have allowed the best improvement in the vertical bone height, although it would result in the loss of a tooth.
Taking these challenges into consideration, it was thus necessary to utilize either soft tissue grafting or manipulation techniques in order to improve the soft tissue profile of the UR3. During the implant placement and exposure, tissue was moved from the palatal to the buccal side to achieve an improved soft tissue profile. An impression was also taken at the time of surgery, before the cover screw was replaced and the area closed. The abutment, metalwork, and temporary crown were made to the ideal contours, and the implant carefully exposed (at which time the soft tissue was manipulated for the second time) in order to use the abutment and temporary crown to create an adequate soft tissue profile for the restoration.
During the process, the patient was fitted with a Maryland bridge, though this debonded several times. In addition to this, therefore, she was provided with a denture to allow an alternative in the event of emergencies.
The patient had not been attending hygiene appointments as regularly as was preferred prior to the start of treatment, and only after receiving the final crown, did she begin to have regular preventive treatment.
Should a case like this present itself in the future, it would be advisable to encourage a young patient like this to consider grafting if it is needed. While a good result was achieved in this instance without grafting, this may not always be the case.
It would also be beneficial to send the patient for a custom shade. The attendant technician, Khristo Ivanov from Uniqa Dental Laboratory, accomplished a great deal with just some photos to guide him, but a custom shade would have given more information.
The patient’s oral hygiene on the opposing arch was a challenge, and despite many hygienist appointments and instruction on interdental cleaning, this did not improve to the desired extent.
[/userloggedin]
[userloggedout][/userloggedout]
- Allen F, Smith DG. An assessment of the accuracy of ridge-mapping in planning implant therapy for the anterior maxilla. Clin Oral Implants Res. 2000;11(1): 34-38.
- Palacci P, Nowzari H. Soft tissue enhancement around dental implants. Periodontol 2000. 2008;47:113-132.
- Sethi A, Sochor P. The lateral fixation screw in implant dentistry. Eur J Prosthodont Restor Dent. 2000;8(1): 39-43.
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;3(12):995-96.
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
- Yuill R. Consent in dentistry. Dental Profile. 2001;6-8.
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores



