Educational aims and objectives
This clinical article aims to present a study to assess the clinical success of implant placement by a single specially designed drill compared with the conventional placement using the sequential drills.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize how the use of single drill is compared to the use of sequential drills
- Recognize what the benefits of shortening the operative time and simplicity can mean for surgeons and patients.
- Identify what drill geometry in general should be used to prepare sites for screw-shaped implants and cylindrical implants.
- Observe some results of several studies that examined the osteotomy preparation temperature produced by drilling with a single drill versus sequential drills.
Drs. Amr Zahran, Ahmed Mortada, and Basma Mostafa present a randomized clinical study on the use of a single drill for implant placements compared to sequential drills
Dental implant success is evident now-adays with the predictable functional and esthetic results obtained (Karaca and Aksakal, 2013). Simplified techniques and approaches are preferred for the convenience of both the patients and operators (Eriksson, et al., 1982).
Current research is focusing on decreasing the number of instruments used, shortening of the operation time, and performing flapless approaches for implant placement whenever possible. This is done to reduce the postoperative complaints such as pain, swelling, and bleeding, thus decreasing the need for analgesics and minimizing the occurrence of morbidity (Eriksson and Albrektsson, 1984).
Using surgical drills under specific rotational speed and torque with copious amounts of irrigation, the implant fixture is placed into bone through preparation of the alveolar bone bed. The osteotomy preparation is usually performed by a sequential set of drills increasing in diameter size or by a simplified osteotomy protocol using a reduced number of drills (only pilot and final drill). The latter technique has the benefit of reduced operative time as compared to the conventional sequential drilling technique (Jimbo, et al., 2013).
Guazzi, et al. (2013), examined the use of single bur compared to sequential drilling for the preparation of the implant bed. They found both techniques resulted in implant osseointegration, but the single-bur technique required less surgical time and revealed less postoperative morbidity.


When considering drill geometry in general, twist drills and taps are used to prepare sites for screw-shaped implants, and triflute drills are used to prepare sites for cylindrical implants (Cordioli and Majzoub, 1997). The OsteoCare™ Ultra 3.25 mm profile drill design is based on the concept of double triflute geometric form. To enable the preparation of a tapered osteotomy, the drill is designed with two cutting planes.
The first trifaceted cutting plane at the point of the drill is at an acute angle to the osteotomy site, is self-stabilizing, and enables accurate initial positioning. The second trifaceted cutting plane, extended along the entire outer edge of the drill, enables cutting along the length of the osteotomy site and produces the tapered form.
The drill may be used for single drilling technique; this shortens the procedure time and reduces the friction between the drill and the bony surface inside the osteotomy during preparation, which reduces the temperature of bone drilling induced by the procedure (Garber, et al., 2001).
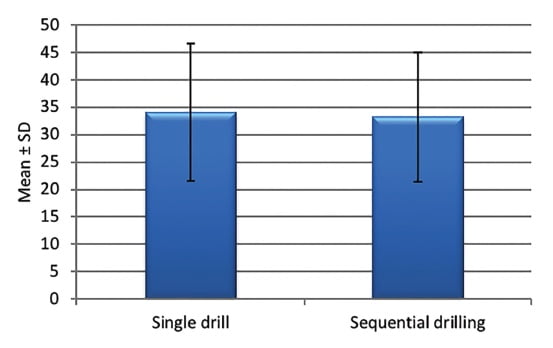
Several studies have examined the osteotomy preparation temperature (Sharawy, et al., 2002). Gehrke, et al. (2015), compared the heat produced by drilling with a single drill versus the use of sequential drills. They concluded that the single drill technique did not generate more heat than sequential drilling. Bulloch, et al. (2012), also reported no significant difference in temperature rise between the use of single drills and sequential drills in 3.5 mm and 4.2 mm diameter implants. The aim of the present study was to assess the clinical success of implant placement by a single, specially designed drill compared to conventional placement using sequential drills.




Materials and methods
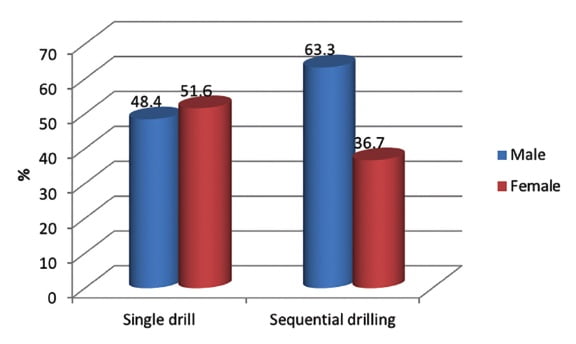
A total of 161 implants were placed: 31 patients received 82 implants placed by a single drill as the test group, and 30 patients received 79 implants placed by the conventional way using sequential drills as a comparative group. Randomization of the patients and concealment of the assessors were performed to avoid any bias.
Patient selection
This study was carried out on 61 patients (34 male and 27 female). Ages ranged from 21 years old to 73 years old with upper or lower edentulous areas requiring restoration by dental implants. The inclusion criteria included implant recipient sites free from any pathological conditions. Patients who were cooperative, motivated, and hygiene-conscious were selected. Patients unable to undergo minor oral surgical procedures and patients with a history of drug abuse or catabolic drugs were not included. Patients with a history of psychiatric disorder and those with unrealistic expectations about the esthetic outcome of implant therapy were also excluded. Patients with insufficient vertical interarch space on centric occlusion to accommodate the available restorative components and those who had any systemic condition that may contraindicate implant therapy were excluded from the study.
Exclusion criteria also included patients who had any habits, such as heavy smoking and alcoholism, that might jeopardize the osseointegration process. Patients with para-functional habits that produce overload on the implant, such as bruxism and clenching, were excluded. The medical condition of the subjects was evaluated according to the modified Cornell Medical Index (Brightman, 1994).
Implant selection
OsteoCare™ Maxi Z two-piece, Maxi Z plus, and Maxi-Z flat-end dental implants were used in this study. They are tapered, two-piece implants with either a pointed or flat end, and available in variable lengths and diameters.
Implant fixture
Tapered screw fixtures with flared collar and internal hex connection were used. The implant is made of titanium alloy (6AL-4V ELI). The implant body is threaded with buttress threads, and the surface is grit-blasted and acid-etched. Variable fixture lengths (10 mm, 12 mm, and 13 mm) were used. Variable fixture diameters (3.75 mm and 4.5 mm) were used.


Implant armamentarium
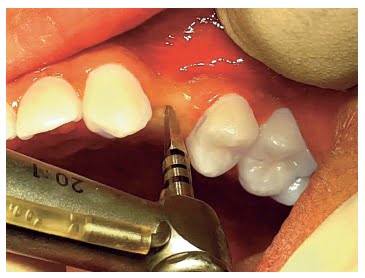
For the test group (group 1), a 3.25 mm diameter stainless steel drill was used. For the control group, four drills (2.2 mm, 2.75 mm, 3.25 mm, and 4 mm diameter), made from either titanium or stainless steel, were used and were mounted on a reduction-speed high-torque, low-speed handpiece. A hex driver (2.2 mm) with different lengths and a ratchet wrench was used for seating the implants. The torque wrench was adjusted at 30 Ncm. A 1.5 mm screwdriver was used to fix the cover screw, as well as to fix the healing collars and abutments postoperatively.
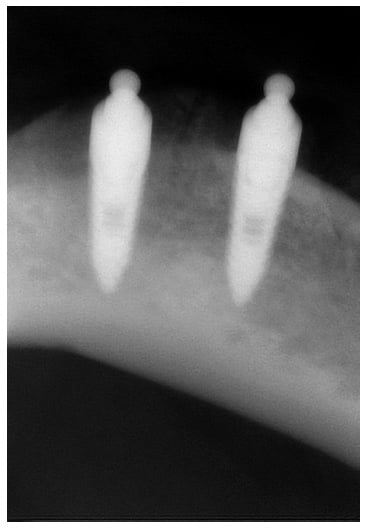
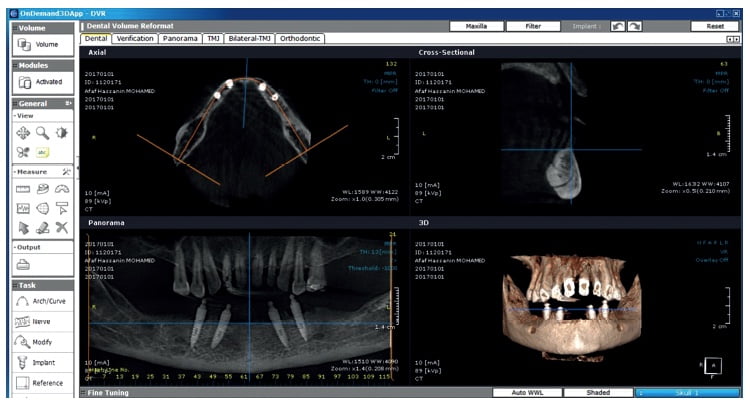
Radiographic assessment
Periapical radiographs were taken for all patients preoperatively, immediately post-operative, and 6 months after implant placement. Cone beam computed tomography was also performed preoperatively for all patients.
Preoperative
Alginate impressions were taken for each patient to obtain study casts for evaluation of the interarch space adequacy and to detect if there was any occlusal discrepancy.
As part of the presurgical preparation, all patients received initial therapy. This included caries removal, restoration, and periodontal debridement. Photographs were also obtained for documentation and comparison.
Surgical protocol
Local anesthesia was induced using articaine with adrenaline 1:100,000. The surgical procedures were flapless in cases where the ridge width was more than 5 mm and free of any bony defects or concavities. In other cases, a full thickness flap elevation was performed, with para-crestal (palatal or lingual) incisions extended by one tooth mesially and distally to the implant site, with two vertical-releasing incisions.
In cases where implants had been immediately inserted in fresh post-extraction sites after atraumatic tooth extraction, the socket was debrided, and the implant was carefully placed in the correct prosthetically driven position, with the implant platform leveled 2 mm below the marginal level of the buccal wall. Implant site preparation was performed using a specially designed tapered triflute drill for group 1 and sequential drills for group 2. The recommended rotation speed is 2000 rpm, and the cooling is obtained by copious irrigation with normal saline. Primary stability was established and checked with the torque wrench to be more than 30 Ncm. After implant placement, the surgical flaps (if performed) were sutured, achieving a soft tissue primary closure.
Postoperative care
Medications were prescribed, including 1,000 mg Augmentin® (GlaxoSmithKline) twice a day for 7 days or Dalacin® C 300 mg (Pfizer) twice a day for penicillin-allergic patients. Paracetamol 500mg was also taken as pain control. Patients were not allowed to use any removable prosthesis. Sutures (where performed) were removed after 10 days.
Follow-up
Clinical evaluation
Each patient was evaluated 6 months postoperatively and examined for the following:
- Discomfort, pain, and tenderness: These were evaluated according symptoms of the patients.
- Condition of the peri-implant tissues: Presence of any abnormalities, including redness and swelling, was checked.
Probing depth was measured on axial surfaces of all implants, according to a standard procedure described by Glavind and Loe (1967) to measure pocket depth that refers to the distance from the peri-implant mucosal margin to the base of the clinical probing depth. The measurements were carried out using a 0.5 mm-thick periodontal probe with Williams calibrations marked from 1 mm to 10 mm. Measurements were taken mesially, buccally, distally, and lingually around the implant. The probing depths were obtained by totaling the four probing depth scores per implant. The sum of these readings was divided by four, and the probing depth score for the implant was obtained.
- Mobility was tested using the Periotest M (Medizintechnik Gulden) to evaluate the clinical stability of the implant. Periotest values -8 to 0 were considered the ideal values to denote successful osseointegration.
- Occurrence of various complications, including:
- biological complications — e.g., peri-implant mucositis, peri-implantitis, fistula, or abscess
- mechanical or prosthetic complications — e.g., fracture of the implant and/or of any prosthetic component, screw loosening.
Radiographic evaluation
Periapical radiographs were taken for all patients preoperatively, immediately postoperatively, and 6 months after implant placement. The known distance between the screw threads or the length of the implant was used to calibrate each image. The implant platform was used as the reference for each measurement.
Radiographs taken at the prosthesis delivery served as the baseline for evaluation of the marginal bone level change over the study period. The linear axial distance between implant platform and the most coronal bone-to-implant contact was measured. To have a single value for each implant, mesial and distal values were averaged.
Oral hygiene level
The presence of plaque and bleeding on probing was evaluated at four surfaces for each tooth or implant and expressed as percentage of positive sites over total sites (full-mouth score).
 Postoperative course
Postoperative course
One week after surgery, patients were asked to complete a short survey to investigate the most common indicators of quality of life in the postsurgical period. Indicators included:
- Pain (on a zero-to-100 visual analogue scale [VAS]) (Hawker, et al., 2011)
- Tissue swelling
- Analgesic drugs taken
Implant success
The success criteria proposed by Buser, et al. (1997), and Cochran, et al. (2002), were adopted at each follow-up visit for each implant. These criteria follow:
- No clinically detectable mobility when tested with Periotest M
- No evidence of peri-implant radiolucency
- No recurrent or persistent peri-implant infection
- No complaint of pain
- No complaint of neuropathies or paresthesia.
Patient satisfaction
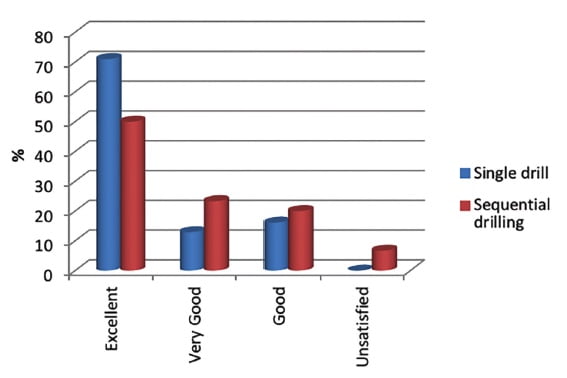
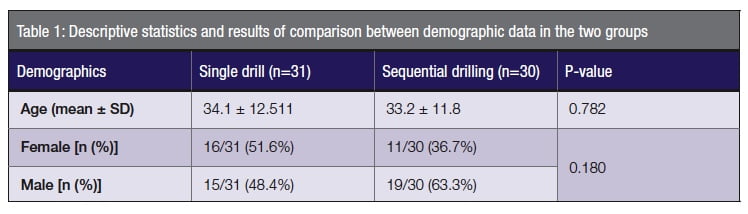
Esthetics, mastication function, and phonetics were assessed using a questionnaire 6 months following placement. The possible answers — excellent, very good, good, sufficient, or poor — were evaluated.
Statistical analysis
Numerical data was explored for normality by checking the distribution of data and using tests of normality (Kolmogorov-Smirnov and Shapiro-Wilk tests). Age data showed normal (parametric) distribution, while bone loss data showed non-normal (non-parametric) distribution.
Data was presented as mean, median, standard deviation (SD), and range values.
For parametric data, the Student’s t-test was used to compare the two groups. For non-parametric data, the Mann-Whitney U test was used. Qualitative data was presented as frequencies and percentages. The Chi-square test (or Fisher’s Exact test when applicable) was used for comparisons regarding qualitative data. The significance level was set at p ≤ 0.05. Statistical analysis was performed with IBM SPSS Statistics Version 20 for Windows.
Results
No biological complications such as peri-implant mucositis, peri-implantitis, fistula, or abscess were aberrant. Also, no mechanical or prosthetic complications such as fracture of the implant and/or of any prosthetic component, screw loosening were detected.
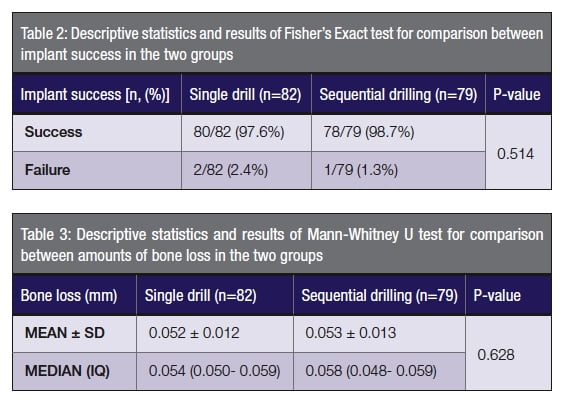
There was no statistically significant difference between mean age values in the two groups (Table 1). There was also no statistically significant difference between gender distributions in the two groups.
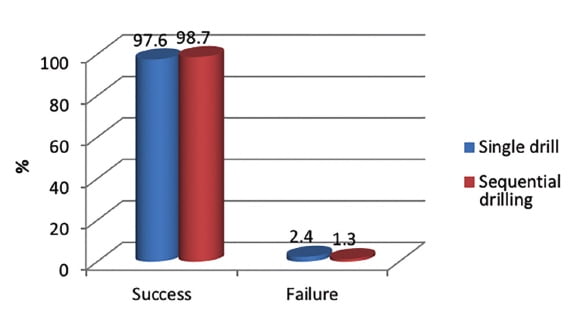
Three implants failed to osseointegrate with bone; mean survival of the implants was 98.2% at the 6-month follow-up. All the remaining implants were in function and stable.
No evidence of peri-implant radiolucency, no suppuration or pain at the implant site, or ongoing pathologic processes were detected.
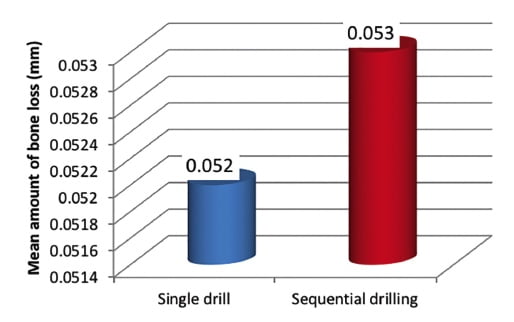
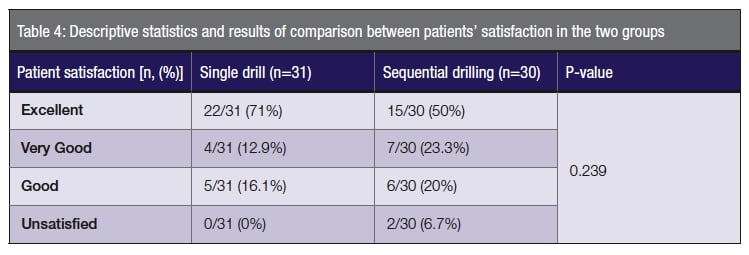
There was no statistically significant difference between implant successes, bone loss, or patient satisfaction in the two groups (Tables 2, 3, and 4).
Discussion
This study reports excellent clinical and radiographic results using a single drill for the preparation of the implant site. Because of fast osteotomy preparation and reduced surgical time, tissues were more preserved, and the postoperative complaints were reduced, providing increased patient satisfaction of the treatment. This could be due to decrease of the osteotomy site temperature (Rafel, 1962).
The Ultra drill is designed to be used with external irrigation, especially at compact cortical bone surfaces where most resistance is found. This allows bone temperature to be kept below the threshold of thermal bone necrosis of 47°C. Maintaining such a high temperature for 1 minute will cause bone resorption and anchorage disturbance of the subsequent implant.
Another important factor when preparing an osteotomy is control of the drill at the start of the procedure, which is usually difficult to achieve when using one-stage drills.
Preventing slippage of the drill will eliminate the risk of injuring the patient and prevent the uncontrolled widening of the osteotomy, which can adversely affect the initial stability of the implant and the final result of implant success. Usual solutions to this are to use site markers to pierce the mucosa and outer layer of bone or to use small diameter pilot drills, but both techniques reduce the advantage of one-stage drilling.
 With the Ultra drill design, the piercing tip of the drill is used to penetrate the soft tissue, when using flapless implant technique, and form an indent in the top layer of bone, preventing slipping even on curved bony surfaces. This is accomplished by the first set of drilling surfaces being at a more acute angle and having only one-fifth of the diameter of the second set of drilling surfaces. This allows the first drilling plane to act as a guide for the second.
With the Ultra drill design, the piercing tip of the drill is used to penetrate the soft tissue, when using flapless implant technique, and form an indent in the top layer of bone, preventing slipping even on curved bony surfaces. This is accomplished by the first set of drilling surfaces being at a more acute angle and having only one-fifth of the diameter of the second set of drilling surfaces. This allows the first drilling plane to act as a guide for the second.
The use of multiset drill points will also eliminate the vibrations that accompany the procedure caused by using the tip of the drill for support on the patient’s bone ridge. This, if combined with shifting from working with a typically complex sequential drilling technique to an enhanced single drilling technique, reduces the working time and the discomfort for the patient. Moreover, due to the design of the Ultra drill and the high angle of the first drill plane, there is a reduction of axial drilling force exerted on the bone by the operator for the osteotomy to be prepared.
The Ultra drill is based on the design to core out the root from the root canal peripherally, but with the added advantage of not requiring an exposed socket. The advantages of the Ultra drill not only affect the practitioner’s work outcome, but also have a positive influence on the patient who experiences shorter procedure times, less pressure forces during osteotomy preparation, and the likelihood of a higher implant success rate (Garber, et al., 2001).
One of the factors that could increase the osteotomy site temperature is the quality of the bone, as the more cortical part may increase the bone density, and the temperature of bone cutting may increase the temperature (Misch, et al., 1999). The conventional way of preparing the implant bed consists of using successive drills increasing in diameter. It’s important to use sharp drills with high-rotational speed to minimize the time of osteotomy and temperature rise.
Conventional protocols consist of different numbers, types of drills used, and different rotation speeds. It has been observed that the use of sharp drills, in combination with high rotation speed, allows the creation of the implant site in a very short time, reducing the risk of developing excessive heat (Tehemar, 1999). The present study found minimum bone loss around the implants using OsteoCare drills (either the sequential or the single drill).
The results of this study showed minimum postoperative complaints (pain, swelling, and bleeding) and minimal use of analgesics due to the minimally invasive approaches either by flapless implant placement or by using the single drill in the test group.
The patients completed a questionnaire at the 6-month follow-up review, and the results showed great satisfaction of the treatment, with no statistically significant difference between the two groups even with the failed implants, which were replaced with new ones after 3 months of healing.
The new era of implant placement regarding the patient-reported outcomes aims to use simplified techniques and quick implant placement, and results in more tissue preservation and patient preference due to the minimal operative and postoperative complications, and maximum osseointegration, functional, and esthetic outcomes.
 Conclusion
Conclusion
The use of the Ultra 3.25 mm single drill is considered an effective approach in implant placement. The clinician benefits are a speedy and simplified technique, while the patient benefits from minimal postoperative symptoms, and maximum functional and esthetic restoration of their lost teeth. For dense bone (D1) in the lower posterior areas, it is advised to combine the single drill technique with sequential drilling.
Beside the use of the single drill technique in implant placement, Dr. Zahran has also co-authored an article outlining the maxillary split-crest technique. Read about it here.
https://implantpracticeus.com/ce-articles/maxillary-split-crest-technique-immediate-implant-placement/.
References
- Brightman VJ. Rational procedure for diagnosis and medical risk assessment. In: Lynch MS, Brightman VJ, Greenberg MS. Burket’s Oral Medicine: Diagnosis and Treatment. 9th ed. Philadelphia, PA: Lippincott; 1994.
- Bulloch SE, Olsen RG, Bulloch B. Comparison of heat generation between internally guided (cannulated) single drill and traditional sequential drilling with and without a drill guide for dental implants. Int J Oral Maxillofac Implants. 2012;27(6):1456-1460.
- Buser D, Mericske-Stern R, Bernard JP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997; 8(3):161-172.
- Cochran DL, Buser D, ten Bruggenkate CM, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13(2):144-153.
- Cordioli G, Majzoub Z. Heat generation during implant site preparation: an in vitro study. Int J Oral Maxillofac Implants. 1997;12(2):186-193.
- Eriksson A, Albrektsson T, Grane B, McQueen D. Thermal injury to bone. A vital-microscopic description of heat effects. Int J Oral Surg. 1982;11(2):115-121.
- Eriksson A, Albrektsson T. The effect of heat on bone regeneration: an experimental study in the rabbit using the bone growth chamber. J Oral Maxillofac Surg. 1984;42(11):705-711.
- Garber DA, Salama MA, Salama H. Immediate total tooth replacement. Compend Contin Educ in Dent. 2001;22(3):210-216.
- Gehrke SA, Bettach R, Taschieri S, et al. Temperature changes in cortical bone after implant site preparation using a single bur versus multiple drilling steps: an in vitro investigation. Clin Implant Dent Relat Res. 2015;17(4):700-707.
- Glavind L, Löe H. Errors in the clinical assessment of periodontal destruction. J Periodontal Res. 1967;2(3):180-184.
- Guazzi P, Grandi T, Grandi G. Implant site preparation using a single bur versus multiple drilling steps: four-month post-loading results of a multicenter randomised controlled trial. Eur J Oral Implantol. 2015;8(3):283-290.
- Hawker G, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63(Suppl 11):S240-S252.
- Jimbo R, Giro G, Marin C, Granato R, et al. Simplified drilling technique does not decrease dental implant osseointegration: a preliminary report. J Periodontol. 2013;84(11):1599-1605.
- Karaca F, Aksakal B. Effects of various drilling parameters on bone during implantology: an in vitro experimental study. Acta Bioeng Biomech. 2013;15(4):25-32.
- Misch CE, Dietsh-Misch F, Hoar J, Beck G, et al. A bone quality-based implant system: first year of prosthetic loading. J Oral Implantol. 1999;25(3):185-197.
- Misch CE, Qu Z, Bidez MW. Mechanical properties of trabecular bone in the human mandible: implications for dental implant treatment planning and surgical placement. J Oral Maxillofac Surg. 1999;57(6):700-706.
- Rafel SS. Temperature changes during high-speed drilling on bone. J Oral Surg Anesth Hosp Dent Serv. 1962;20:475-477.
- Sharawy M, Misch CE, Weller N, Tehemar S. Heat generation during implant drilling: the significance of motor speed. Int J Oral Maxillofac Implants. 2002;60(10):1160-1169.
- Tehemar SH. Factors affecting heat generation during implant site preparation: a review of biologic observations and future considerations. Int J Oral Maxillofac Implants. 1999;14(1):127-136
Stay Relevant With Implant Practice US
Join our email list for CE courses and webinars, articles and mores

 Postoperative course
Postoperative course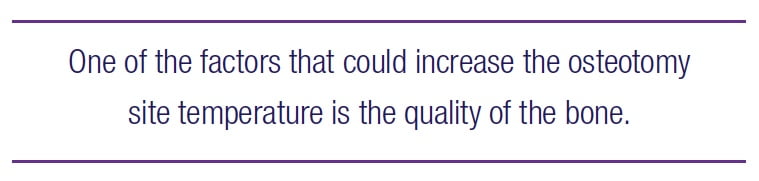 Conclusion
Conclusion
